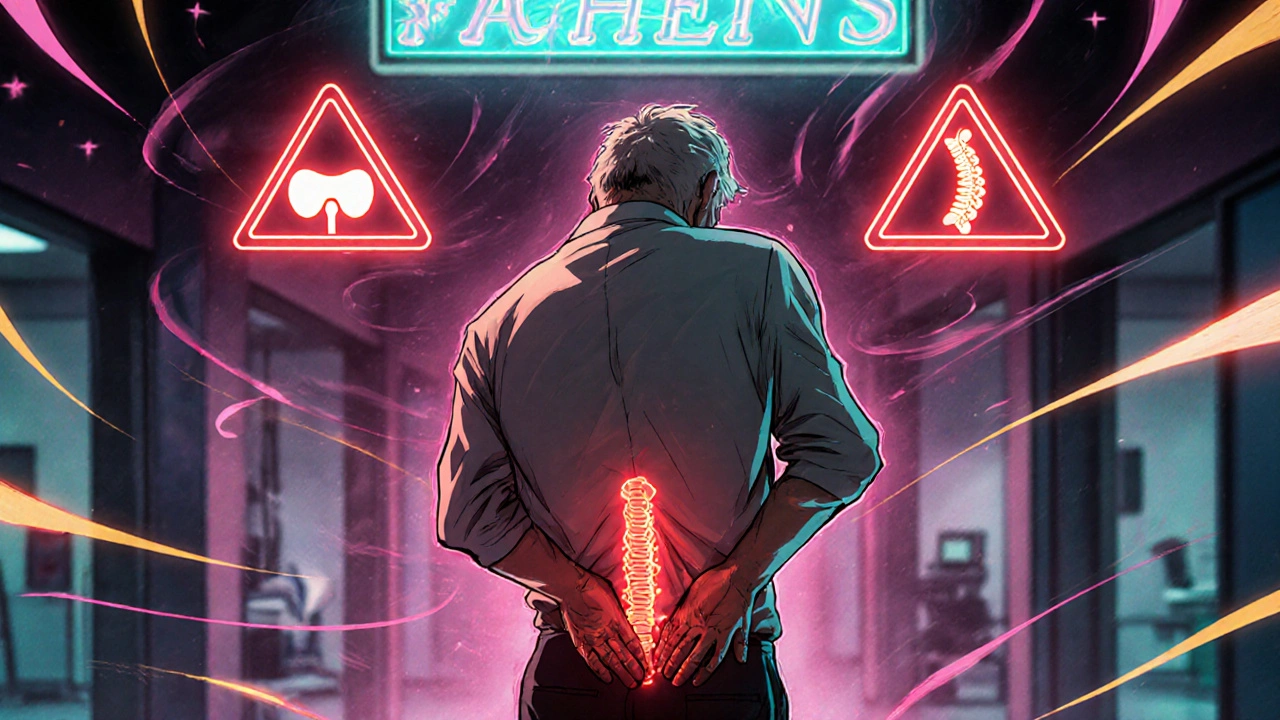
Most people will experience back pain at some point. It’s common, often temporary, and usually gets better with rest, movement, and over-the-counter pain relief. But sometimes, back pain isn’t just a muscle strain-it could be a sign of something serious. Knowing the back pain red flags can mean the difference between a few days off work and permanent nerve damage, or even life-threatening complications.
What Are Back Pain Red Flags?
Red flags aren’t just vague warnings. They’re specific clinical signs that point to serious underlying conditions like spinal infections, tumors, fractures, or nerve compression. These conditions don’t resolve on their own. Delaying diagnosis can lead to paralysis, loss of bladder control, or spread of cancer. According to the American College of Emergency Physicians, about 10% of back pain cases involve serious pathology-and missing those cases is one of the top reasons for malpractice claims in emergency medicine. The goal isn’t to scare you. It’s to help you recognize when it’s time to stop waiting it out and seek urgent care. Most back pain is harmless. But if you have one or more of these signs, don’t wait for it to get worse.Red Flags That Demand Immediate Attention
There are five major red flags that should trigger immediate medical evaluation:- Cauda equina syndrome: This is a neurological emergency. Signs include loss of bladder or bowel control, numbness in the saddle area (around your genitals and inner thighs), or sudden weakness in both legs. If you experience any of these, go to the ER immediately. Surgery within 48 hours is often needed to prevent permanent disability.
- History of cancer: If you’ve had cancer in the past-especially breast, lung, prostate, or kidney cancer-new back pain could mean the cancer has spread to your spine. A 2017 review found that cancer history increases the likelihood of spinal metastasis by 6 to 15 times.
- Unexplained weight loss: Losing weight without trying, especially if you’re over 50, can signal an underlying tumor or chronic infection. When paired with back pain, it’s a major red flag.
- Fever or chills: Back pain with fever suggests infection. Spinal osteomyelitis (bone infection) or an abscess can develop slowly but become life-threatening fast. One study found 78% of patients with spinal infections had pain that didn’t improve with painkillers, while only 22% of those with simple muscle strains had the same issue.
- Recent trauma or fall: A car crash, fall from height, or even a hard stumble can cause a spinal fracture, especially if you’re older or have osteoporosis. In people over 70, over a third of back pain cases are due to fractures. Plain X-rays often miss these-CT scans are far more accurate.
Age and Risk Factors That Change the Game
Age matters. Back pain in someone under 18 or over 50 needs more careful evaluation than in a healthy 30-year-old. Why?- Under 18: Conditions like tumors, infections, or congenital spine issues are more common in children and teens than in adults.
- Over 50: Risk of fractures, cancer, and degenerative spine disease rises sharply. Osteoporosis affects nearly half of women over 65. Steroid use, even for asthma or arthritis, weakens bones and increases fracture risk.
When Pain Doesn’t Get Better
Most back pain improves in 4 to 6 weeks. If it doesn’t, that’s a red flag in itself. A 2018 study showed patients whose pain didn’t improve after four weeks were almost 20 times more likely to need surgery than those who got better. This isn’t about laziness or being “sensitive.” It’s about biology. If your body isn’t healing, something else is going on. Persistent pain can mean:- Spinal stenosis (narrowing of the spinal canal)
- Chronic nerve compression
- Early-stage infection or tumor
- Undiagnosed rheumatological condition
Imaging: What’s Needed and What’s Not
You might think MRI or X-ray is the obvious next step. But here’s the truth: 90% of people with back pain don’t need imaging at all. The American College of Radiology says imaging without red flags is rarely appropriate. Why? Because:- Most people over 40 have disc degeneration on MRI-even if they’ve never had pain.
- Up to 79% of asymptomatic 80-year-olds show disc bulges or arthritis on scans.
- Unnecessary imaging leads to more tests, more anxiety, and more surgeries that don’t help.
- For suspected infection or tumor: MRI is the gold standard. It’s 95% sensitive for cauda equina syndrome and detects bone marrow changes before X-rays can.
- For trauma or fracture: CT scan is far better than X-ray. X-rays miss up to 36% of fractures in older adults. CT catches 98%.
- For nerve compression: MRI shows soft tissue, nerves, and discs. X-rays only show bones.
When to See a Specialist
You don’t need to go straight to a neurosurgeon. But you should be referred if:- You have any of the five major red flags listed above.
- You have progressive numbness, weakness, or loss of coordination in your legs.
- You have bowel or bladder changes.
- You have unexplained fever with back pain.
- Your pain has lasted longer than six weeks despite conservative care.
What About Painkillers and Rest?
Resting for days on end is outdated advice. Movement-even gentle walking-helps most back pain. Painkillers like ibuprofen or acetaminophen can help manage discomfort, but they won’t fix the underlying issue if a red flag is present. If pain doesn’t improve with medication, that’s a warning sign. In spinal infections, pain persists despite treatment in 78% of cases. In mechanical pain, it usually improves within days. Don’t rely on painkillers to mask the problem. They’re a tool, not a solution.What’s Changing in 2025?
Guidelines are evolving. The American Pain Society is testing a new risk-stratification tool called STarT Back, which uses questionnaires to predict who’s at risk for serious outcomes-not just red flags, but a mix of physical, emotional, and lifestyle factors. Early results show it’s 83% accurate. Point-of-care ultrasound (POCUS) is also being studied. In emergency rooms, it can quickly check for bladder distension-a sign of nerve compression-without sending patients for full MRI. One 2022 study found POCUS was 92% accurate at detecting this, potentially cutting unnecessary scans by 35%. And machine learning? Hospitals are starting to use AI to analyze patient history and symptoms to predict red flags with 89% accuracy-better than traditional checklists. The future isn’t just about finding red flags. It’s about predicting who’s at risk before they even show up.Final Takeaway
Back pain is common. Serious causes are rare. But they’re real-and they’re dangerous if ignored. If you have:- Loss of bladder or bowel control
- Unexplained weight loss with back pain
- Fever and back pain
- A history of cancer
- Recent trauma and you’re over 50
- Pain that hasn’t improved after a month
Is it normal for back pain to last more than a few weeks?
It’s common for mild back pain to last up to 6 weeks, especially after a strain or overuse. But if your pain hasn’t improved after 4 to 6 weeks, or if it’s getting worse, that’s a red flag. Persistent pain can signal nerve compression, infection, or early-stage spinal disease. At that point, imaging and specialist evaluation are needed-not just more rest or painkillers.
Can an X-ray detect a spinal tumor?
X-rays can sometimes show bone destruction or changes caused by a tumor, but they’re not reliable for detecting early-stage tumors or soft tissue involvement. Most spinal tumors start inside the bone marrow or nerve tissue, which X-rays can’t see. MRI is the best test for tumors because it shows soft tissue, nerves, and bone marrow in detail. If a tumor is suspected, an X-ray might be done first, but an MRI will almost always follow.
Do I need an MRI if I have back pain and am over 60?
Not automatically. Many people over 60 have disc degeneration or arthritis on MRI-even if they have no pain. An MRI is only needed if you have red flags like unexplained weight loss, fever, neurological symptoms, or trauma. If your pain is mild and improving, imaging isn’t helpful and may lead to unnecessary procedures. But if you have any warning signs, don’t delay an MRI.
Can back pain be caused by an infection?
Yes. Spinal infections like osteomyelitis or discitis are rare but serious. They often start slowly and may not cause obvious fever at first. Signs include worsening pain that doesn’t respond to painkillers, night pain that wakes you up, unexplained weight loss, and sometimes chills or fatigue. People with diabetes, IV drug use, or recent surgery are at higher risk. If infection is suspected, blood tests and MRI are essential.
What happens if I ignore red flags?
Ignoring red flags can lead to permanent damage. Cauda equina syndrome can cause lifelong bladder and bowel dysfunction if not treated within 48 hours. Spinal infections can destroy bone and spread to the bloodstream. Untreated tumors can grow and compress the spinal cord. In one study, 12% of malpractice cases involving back pain were due to delayed diagnosis of serious conditions. Early detection saves mobility, function, and sometimes life.
Back pain is rarely an emergency-but sometimes, it’s the only warning you get. Know the signs. Trust your body. And don’t hesitate to ask for help when something doesn’t feel right.






Jeremy Hernandez
18 November, 2025 03:56 AMLook, I’ve seen too many people ignore back pain until they’re in a wheelchair. That cauda equina thing? Real. My cousin waited three weeks because he thought it was ‘just a pulled muscle.’ Now he’s got permanent bladder issues. Don’t be him. Go get scanned if it’s not improving. No excuses.
And stop listening to yoga influencers who say ‘just move more.’ Sometimes your spine is screaming, not asking for a stretch.
Tarryne Rolle
19 November, 2025 02:05 AMInteresting how this article frames everything as binary: either it’s a pulled muscle or you’re one step away from paralysis. What about the 80% of cases that are just… weird? Chronic pain that doesn’t fit neat boxes? The medical system loves red flags because they’re easy to document. But real bodies don’t follow checklists.
Also, why is MRI always the answer? I’ve had three. None helped. Just made me anxious and broke.
Holli Yancey
19 November, 2025 22:27 PMI appreciate how this breaks down the real dangers without fearmongering. I’ve had chronic back pain for years, and I used to feel guilty for not ‘just pushing through.’ But when I started getting numbness in my feet and couldn’t control my bladder after a fall, I went in. Turns out it was a herniated disc compressing a nerve.
It wasn’t cancer. Not an infection. But it was serious enough that waiting would’ve made it worse. Trust your body. Even if it’s not ‘red flag’ level, if something feels off, get it checked.
Jessica Healey
21 November, 2025 21:44 PMokay so like i had back pain for 3 weeks and i was like ‘meh’ and then i woke up one day and couldnt pee properly and i thought i was dying and then i went to er and they were like ‘oh its just a UTI’ and i was like ‘but my spine??’ and they were like ‘nope’ and i cried in the parking lot
but then like 2 weeks later it was fine?? so maybe the red flags are just overhyped?? idk i’m confused now
Levi Hobbs
22 November, 2025 07:11 AMImportant note: The 10% statistic cited-about serious pathology-is widely accepted, but it’s often misinterpreted. It doesn’t mean 1 in 10 people with back pain have cancer-it means 1 in 10 of those who seek care for back pain have something serious. Most people with back pain don’t go to the doctor at all. So the real risk is far lower-but still, if you’re in that 10%, you’re glad you went.
Also: Rest is not always bad. Sometimes, 48 hours of rest is exactly what you need to let inflammation settle. It’s not “outdated advice”-it’s context-dependent.
henry mariono
23 November, 2025 00:21 AMI’ve been a physical therapist for 18 years. I’ve seen people ignore red flags. I’ve also seen people panic over minor aches and demand MRIs they don’t need. The truth is somewhere in the middle.
If you’re under 50, healthy, and the pain is mechanical-worse when sitting, better when walking-then yes, rest and movement are fine.
If you’re over 60, lost 15 pounds, and your pain wakes you up at 3 a.m.? Go. Now.
Sridhar Suvarna
23 November, 2025 01:15 AMAs someone from India where healthcare access is uneven, I appreciate this guide. But let’s be real-most people here can’t afford MRI or even a CT scan. We rely on doctors who may not have time to spot red flags.
So the real issue isn’t just knowing the signs-it’s building systems that make early detection possible for everyone, not just those who can pay.
Also, pain is not weakness. Asking for help is strength.
Joseph Peel
24 November, 2025 03:34 AMThere’s a cultural problem here. In America, we treat pain like a failure of willpower. ‘Just move more.’ ‘It’s all in your head.’ Meanwhile, in Japan or Germany, patients with persistent back pain are evaluated systematically within days.
Our system rewards speed over care. Red flags are a band-aid on a broken system. But they’re better than nothing.
Kelsey Robertson
25 November, 2025 23:29 PMOf course the article says ‘90% don’t need imaging’-that’s what the insurance companies want you to believe. They don’t want to pay for MRIs. They want you to suffer quietly until you’re disabled, then slap you with a ‘pre-existing condition’ label.
And ‘trust your gut’? That’s what they say when they’ve already dismissed you. I’ve had three doctors tell me ‘it’s just stress’-then I ended up in surgery for a tumor.
Red flags are a joke. If you feel wrong, demand imaging. Even if you’re ‘not supposed to.’
Joseph Townsend
26 November, 2025 13:49 PMMY BACK WAS SCREAMING FOR 7 MONTHS AND NO ONE LISTENED.
I thought I was being dramatic. Turns out I had a spinal abscess. I had fever, night sweats, and pain so bad I cried during sex. My doctor said ‘try yoga.’
I had to go to the ER, beg, and threaten to sue before they did an MRI. They found a golf-ball-sized infection wrapped around my spine.
Now I’m on antibiotics for 6 months. And I’ll never trust a doctor who says ‘it’s probably fine’ again.
If you feel like your spine is being eaten by a demon-GO. NOW. DON’T WAIT.
Bill Machi
26 November, 2025 14:57 PMThis is why America is falling apart. We’re told to ‘listen to our bodies’ but then the system punishes us for doing so. You get flagged for red flags? Insurance denies care. You don’t get flagged? You die in pain.
And now we’re letting AI make diagnoses? That’s just replacing one bureaucracy with another. The real problem? Profit-driven medicine. Not lack of red flags.
Elia DOnald Maluleke
27 November, 2025 04:59 AMIn my village in South Africa, we have no MRI machines. We have grandmothers who know when the pain is ‘bad pain’ and when it’s just tired bones. They say: ‘If you cannot stand to pray, it is not just the back. If you cannot laugh without crying, it is not just the back.’
Red flags? Perhaps. But wisdom? That is older than any checklist.
satya pradeep
28 November, 2025 04:11 AMbro i had back pain for 2 months and i was like ‘its just stress’ then i started losing weight and my legs felt like jelly and i went to doc and they were like ‘yo ur spine is full of cancer’
so yeah listen to this article. if you feel like something is wrong even if you dont know what-just go. dont wait. i was 32 and thought i was invincible. i was wrong.
Prem Hungry
30 November, 2025 00:48 AMHey friend, I know how scary this can feel. If you're reading this and you're worried-take a breath. You're not alone. Go to your doctor. Bring this article. Say: ‘I’m scared. I need to rule out something serious.’
You don’t have to be loud. You don’t have to argue. Just be steady. Ask for the right tests. You deserve care.
And if they say ‘it’s nothing’ and you still feel it? Go again. And again. Until someone listens.
Leslie Douglas-Churchwell
1 December, 2025 04:05 AMAI diagnosing back pain? 😏 How cute. Let’s just hand over our bodies to Silicon Valley algorithms trained on biased datasets while Big Pharma profits from unnecessary MRIs. Meanwhile, the real epidemic? Medical gaslighting. Women, POC, and elderly patients are dismissed 7x more often. Red flags are a Band-Aid on a systemic wound.
And don’t get me started on ‘rest is outdated.’ Who wrote this? A gym influencer with a PhD in capitalism? 🤡
Real healing? It’s not in scans. It’s in time, trust, and trauma-informed care. But that doesn’t sell ads.
Stay woke. Stay loud. Demand better.