Flu Risk Assessment for Seniors
Personal Information
Risk Assessment Results
Enter your information and click "Assess Risk Level" to see your personalized risk assessment.
Key Recommendations
- Get vaccinated annually
- Practice good hand hygiene
- Manage chronic conditions
- Avoid close contact with sick individuals
- Maintain healthy lifestyle habits
When winter rolls around, Influenza is a viral infection that attacks the respiratory tract and spreads easily through droplets becomes a top health worry, especially for the flu in the elderly. Older adults face higher odds of severe illness, hospital stays, and even death. Understanding why, spotting the signs early, and taking the right steps to protect seniors can turn a scary season into a manageable one.
Why Older Adults Are More Vulnerable
The first thing to grasp is that age changes the body’s defenses. The immune system becomes less responsive to new threats as we age, a phenomenon called immunosenescence. This slower response lets the flu virus replicate longer before the body can fight back.
Adding to the weakened immunity, many seniors live with chronic diseases such as heart disease, diabetes, or chronic obstructive pulmonary disease (COPD). These conditions not only strain the body but also interfere with the effectiveness of the immune response. Research from the World Health Organization (WHO) shows that adults 65+ are three to five times more likely to be hospitalized from flu compared with younger, healthy adults.
Another risk factor is the higher chance of developing respiratory complications like pneumonia, bronchitis, or exacerbations of existing lung disease. In fact, pneumonia accounts for roughly 30% of flu‑related deaths among seniors.
Finally, seniors often live in close‑quarter settings-nursing homes, assisted‑living facilities, or multigenerational homes-where the virus can spread like wildfire. When many people are together, the concept of herd immunity protects the vulnerable by reducing overall virus circulation becomes crucial.
Spotting the Flu Early: Symptoms to Watch
Flu symptoms in younger people are classic: fever, chills, body aches, and a sudden cough. In older adults, the picture can be muddier. A fever may be low‑grade or absent, while confusion or a sudden decline in functional ability can be the first red flag.
- Fever (often < 100°F or none at all)
- Persistent cough, sometimes producing sputum
- Muscle aches, especially in the back and legs
- Fatigue that feels deeper than usual tiredness
- Headache or dizziness
- Loss of appetite and dehydration
- New or worsening shortness of breath
- Sudden confusion, delirium, or falls
When an older adult shows any combination of these, especially confusion or a rapid drop in activity level, call a healthcare professional right away. Early antiviral treatment works best within 48 hours of symptom onset.
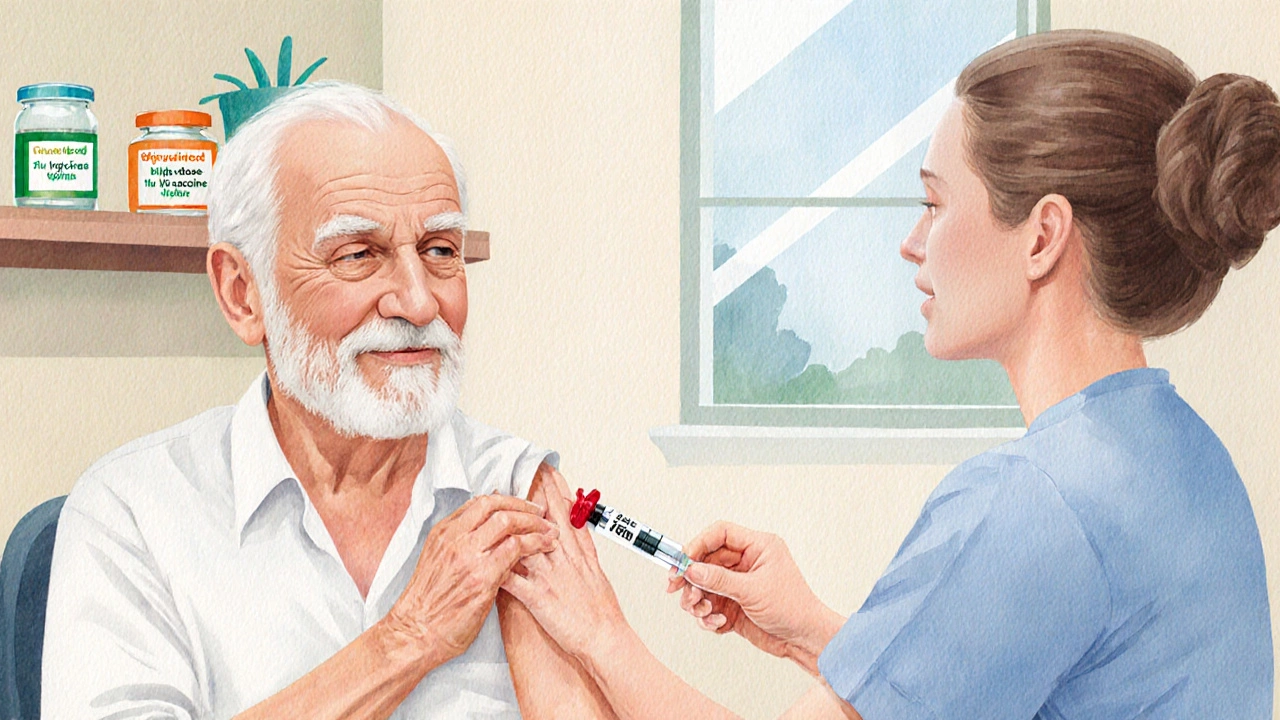
Vaccination: The Cornerstone of Prevention
The most effective shield against flu is the annual influenza vaccine a shot that trains the immune system to recognize the most common flu strains each season. For seniors, there are three main options:
| Vaccine Type | Typical Dose | Key Ingredient | Benefits for Seniors |
|---|---|---|---|
| Standard‑dose | 0.5mL | Inactivated virus | Widely available, good baseline protection |
| High‑dose | 0.5mL (four times antigen) | Inactivated virus, boosted antigen | ~24% better efficacy in preventing hospitalization |
| Adjuvanted | 0.5mL | Inactivated virus + adjuvant | Stronger immune response, useful for very frail seniors |
Most health agencies, including the Centers for Disease Control and Prevention (CDC U.S. public health authority that issues annual flu vaccine recommendations), advise anyone 65+ to get a high‑dose or adjuvanted shot when possible.
Getting the vaccine isn’t a one‑time fix. Because flu viruses mutate, you need a fresh shot each flu season the period, typically from October through March in the Northern Hemisphere, when flu viruses circulate most. Early vaccination (September‑October) gives the body time to build protection before the virus peaks.
Beyond the Shot: Everyday Preventive Measures
Vaccination is powerful, but it works best alongside simple habits.
- Hand hygiene: Wash with soap for at least 20 seconds or use an alcohol‑based sanitizer after touching public surfaces.
- Respiratory etiquette: Cover coughs with a tissue or elbow, and discard tissues immediately.
- Stay active: Light exercise (walking, chair yoga) boosts circulation and supports the immune response.
- Nutrition: Foods rich in vitaminC, vitaminD, and zinc (citrus fruits, fortified dairy, legumes) help maintain immune health.
- Hydration: Seniors can easily become dehydrated; aim for at least 1.5L of fluids daily.
- Regular check‑ups: Keep chronic conditions well‑controlled; blood pressure, glucose, and lung function monitoring reduces complications.
For those living in communal settings, facility staff should enforce visitor vaccination policies and conduct regular flu‑screening during outbreaks.
When Flu Hits: Treatment Options
If an older adult does contract flu, timely treatment can cut the risk of severe outcomes.
Antiviral drugs, such as oseltamivir an oral neuraminidase inhibitor that reduces flu virus replication, are most effective when started within 48hours of symptom onset. Older patients often benefit from a full five‑day course, even if they start a bit later, because the potential to prevent hospitalization outweighs side‑effect concerns.
Supportive care is also key:
- Adequate fluids to avoid dehydration.
- Fever reducers like acetaminophen (avoid NSAIDs if kidney issues are present).
- Oxygen therapy for those with low blood‑oxygen levels.
- Chest physiotherapy to clear secretions in patients with COPD.
Always involve a healthcare provider to adjust medications, especially if the senior is on anticoagulants, heart meds, or steroids.
Planning for the Next Flu Season
Preparation starts long before the first sniffles appear.
- Mark the vaccination window on the family calendar (ideally late September).
- Discuss vaccine type with the doctor-high‑dose or adjuvanted may be recommended based on health status.
- Stock up on basic supplies: hand sanitizer, tissues, a thermometer, and a course of antivirals (prescribed in advance if possible).
- Review chronic disease management plans; update medications and schedule routine labs.
- Educate caregivers and household members about infection‑control steps.
- Consider a flu‑prevention checklist for quick daily reminders (see box below).
- Vaccinated this season?
- Hand‑wash before meals and after outings?
- Wearing a mask in crowded indoor spaces?
- Staying hydrated (≥1.5L water/day)?
- Taking prescribed meds for chronic conditions?
- Scheduled doctor visit for any new symptoms?
By turning these items into habits, families can dramatically lower the chance of a severe flu episode.
Key Takeaways
- Age‑related immune decline and chronic illnesses raise flu risk for seniors.
- Symptoms may be subtle-watch for fever, cough, sudden fatigue, or confusion.
- Annual flu vaccination, preferably high‑dose or adjuvanted, is the most effective defense.
- Hand hygiene, nutrition, and chronic‑disease control add extra layers of protection.
- Early antiviral treatment and supportive care can prevent hospital stays.

Frequently Asked Questions
Can a senior get the flu vaccine if they have a mild cold?
Yes. A mild respiratory infection does not contraindicate vaccination. The immune system can still mount a response, and delaying the shot could leave the person unprotected during the peak season.
What’s the difference between a high‑dose and an adjuvanted flu vaccine?
High‑dose vaccines contain four times the amount of antigen, giving the immune system a bigger target to learn from. Adjuvanted vaccines add a substance that boosts the immune reaction, helping those with weaker responses. Both aim to improve protection for people 65+, but the high‑dose focuses on quantity, while the adjuvant focuses on quality.
If an older adult shows confusion, should I assume it’s the flu?
Confusion can be a flu symptom, but it’s also a sign of many other conditions (UTI, dehydration, medication side‑effects). Call a healthcare professional immediately to rule out serious causes and get proper treatment.
How long does flu immunity last after vaccination?
The protection wanes after about six months, which is why a yearly shot is recommended. Immunity is strongest for the first three months post‑vaccination.
Are antiviral pills safe for seniors with kidney problems?
Oseltamivir is mainly cleared by the kidneys, so dose adjustments are needed for reduced kidney function. A doctor will calculate the right dose based on the patient’s creatinine clearance.






Laneeka Mcrae
4 October, 2025 14:03 PMThe flu in seniors is not just a seasonal nuisance, it’s a major public‑health threat that demands proactive measures.
Age‑related immunosenescence means the immune system responds slower, giving the virus more time to cause damage.
Chronic conditions such as heart disease, diabetes, and COPD further compromise the body's ability to fight infection.
Studies from the WHO consistently show that people over 65 are three to five times more likely to be hospitalized for flu than younger adults.
Hospitalization rates climb sharply once you add multiple comorbidities, with pneumonia accounting for roughly a third of flu‑related deaths in this group.
Vaccination remains the single most effective tool, especially the high‑dose and adjuvanted formulations that deliver a stronger antigenic stimulus.
The high‑dose vaccine contains four times the antigen of the standard shot, translating into about a 24 % reduction in hospitalizations, according to CDC data.
Likewise, the adjuvanted vaccine includes an immune‑boosting compound that enhances the response in frail elders.
Timing matters too; getting the shot in September or early October lets immunity build before the virus peaks in winter.
Hand hygiene, respiratory etiquette, and adequate hydration are low‑cost, high‑impact habits that supplement the vaccine’s protection.
For seniors living in communal settings, staff should enforce visitor vaccination policies and conduct regular symptom screens.
Early antiviral therapy with oseltamivir is most effective within the first 48 hours, but even later initiation can lower the risk of severe complications.
Supportive care-fluids, fever reducers, and oxygen when needed-should be coordinated with a primary‑care provider to adjust existing medications.
Nutritional support, especially adequate vitamin D, vitamin C, and zinc, can help maintain immune competence throughout the season.
Caregivers should keep a checklist handy: vaccine status, hand‑wash supplies, thermometer, and a plan for rapid medical evaluation if confusion or sudden fatigue appear.
In short, combining a high‑dose or adjuvanted vaccine with good hygiene, chronic‑disease management, and early treatment creates a multi‑layered defense that saves lives and reduces health‑care costs.
Robert Frith
16 October, 2025 07:39 AMMate, the flue season hit the UK like a warzone, and our seniors are on the front line, proper battlin' it out with a virus that don't give a toss about age. The NHS is swamped, the care homes are makin' headlines, and everyone’s shoutin' about vaccine slots while the old folk are left waitin' in line, numb with cold air and fear. It's not just a sniffle, it's a full‑blown assault, and the government needs to stop playin' politics and start protectin' the elderly, big time. If we don't get high‑dose shots into their arms right now, we're lookin' at a wave of hospital beds that'll crush the system. No more dawdlin', no more half‑measures – get the proper vaccine, stock up on hand‑gel, and keep those doors shut when the streets are full of coughing strangers.
Albert Gesierich
28 October, 2025 00:15 AMJust a quick note: throughout the article the term “flu” is occasionally misspelled as “flue,” which actually refers to a chimney pipe. Also, the phrase “high‑dose or adjuvanted shot” should be hyphenated consistently, and “antigen” is singular, not “antigens.” These minor errors can confuse readers, especially when discussing medical recommendations, so it’s best to correct them for clarity.
Brad Tollefson
8 November, 2025 17:51 PMHonestly, the guide hits most of the key points without overcomplicating things – vaccination, hand‑washing, and keeping an eye on any sudden changes in seniors’ behavior. I’ve seen a few of my grandparents follow the checklist and it really helped them stay on track during the last flu season.
Paul van de Runstraat
20 November, 2025 11:27 AMSure, Brad, but let’s not pretend the checklist is magic. Some of us still end up in the ER because a single missed dose or a forgotten reminder can turn a mild cough into a full‑blown emergency. Still, kudos for the practical vibe.
Suraj Midya
2 December, 2025 05:03 AMIn India, we face a massive flu burden every winter, especially in densely populated cities where multigenerational homes are the norm. The government recommends the quadrivalent high‑dose vaccine for seniors, but availability is patchy, so many rely on the standard dose. Adding to that, air pollution exacerbates respiratory conditions, making the flu even riskier for older adults with COPD. Public health campaigns stress the importance of masks and indoor ventilation during peak months, which has helped curb some of the spread.
ashish ghone
13 December, 2025 22:39 PMYou're spot on, Suraj! 🌟 The combination of poor air quality and crowded living spaces creates a perfect storm for the flu to wreak havoc on our elders. It's crucial that families prioritize vaccination and maybe even consider air purifiers at home to reduce particulate matter. Also, regular check‑ups for chronic conditions can catch early signs of deterioration before the flu hits hard. I've seen neighbors who started using simple saline rinses and saw a noticeable drop in cough frequency during the season. Remember, staying hydrated, getting enough sleep, and eating a balanced diet rich in antioxidants can give the immune system that extra push it needs. Keep spreading the word, and let's push for better vaccine distribution so everyone, regardless of location, gets the best protection possible. 🙏💪
steph carr
25 December, 2025 16:15 PMGreat insights, everyone! It’s encouraging to see so many practical tips surfacing – from vaccine choices to daily habits. Let’s keep the momentum going and make sure our senior loved ones feel supported and safe throughout the flu season.
Vera Barnwell
6 January, 2026 09:51 AMHonestly, Steph, while all that feel‑good advice sounds nice, there’s a shadow side that most people ignore – the pharmaceutical lobby pushing certain vaccines while keeping alternative preventative measures out of the spotlight. The media barely mentions the role of environmental toxins that weaken immunity, and that’s a massive oversight. If we don’t start questioning the narrative, we’ll keep watching our elders suffer under a veil of “standard care.”
David Ross
18 January, 2026 03:27 AMIndeed, Vera; the conversation around flu prevention is complex, and while vaccines are undeniably crucial, it’s also vital to address broader health determinants-nutrition, air quality, and access to care-all of which intertwine to influence outcomes; let’s continue to share comprehensive strategies that empower seniors and their caregivers alike.
Henry Seaton
29 January, 2026 21:03 PMVaccines work, simple as that.
Baby Thingie
10 February, 2026 14:39 PMIt is essential to adhere to the recommended vaccination schedule to mitigate influenza risk in elderly populations. 😊
Abby Elizabeth
22 February, 2026 08:15 AMUgh, another long‑winded article about flu… like we needed more of the same old boring health tips. It’s like they just copy‑paste the same stuff every year and expect us to be impressed. Someone please spice it up!