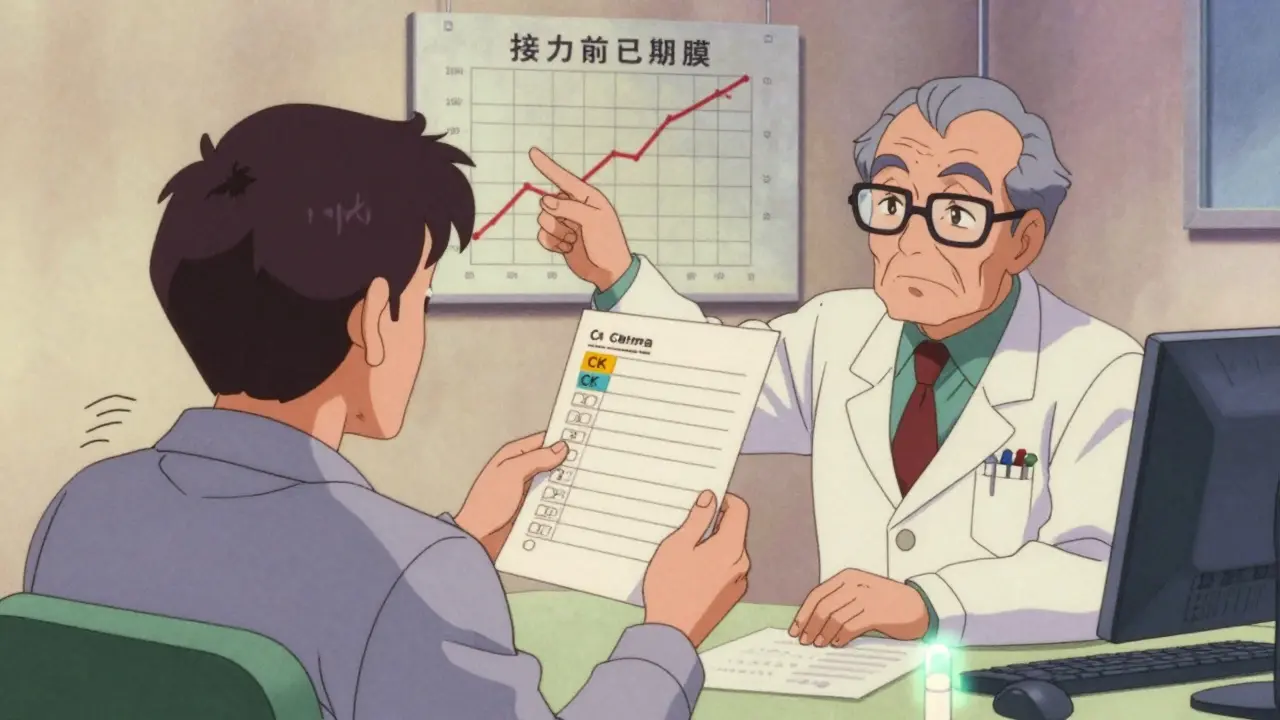
Statin CK Testing Decision Tool
Is Baseline CK Testing Needed for Your Statin?
This tool helps determine if you fall into a high-risk group where baseline CK testing is recommended before starting statin therapy. Based on evidence from medical guidelines and studies.
Your CK Testing Recommendation
Key risk factors identified:
When you start a statin, your doctor might order a blood test for creatine kinase (CK). But is it really necessary? For most people, the answer is no - unless you fall into a specific group. Baseline CK testing isn’t about routine monitoring. It’s about baseline CK testing as a safety net, not a standard step.
Why CK Matters with Statins
Statins work by lowering LDL cholesterol, but they can sometimes cause muscle damage. That’s where creatine kinase comes in. CK is an enzyme released when muscle cells break down. High levels in the blood signal possible injury - from mild soreness to rare, dangerous rhabdomyolysis, where muscle tissue breaks down so badly it can damage the kidneys. The problem? Many people feel muscle aches after starting statins - about 5 to 10% do. But in most cases, it’s not actually caused by the drug. Studies show that up to 78% of patients reporting muscle pain have no rise in CK. That means their symptoms aren’t from the statin. Without a baseline CK test, doctors can’t tell the difference between a normal muscle ache and real statin toxicity.When Baseline CK Testing Makes Sense
You don’t need a CK test just because you’re starting a statin. But you should get one if any of these apply:- You’re over 75 years old
- You have kidney problems (eGFR under 60)
- You’re taking other drugs that interact with statins - like amiodarone, fibrates, or certain antibiotics
- You have hypothyroidism (about 1 in 8 statin users do)
- You’ve had muscle pain or high CK levels on statins before
- You’re on high-intensity statins like atorvastatin 40-80 mg or rosuvastatin 20-40 mg
What’s a Normal CK Level?
There’s no single number for “normal.” It varies by sex, age, muscle mass, and ethnicity.- Men: 145-195 U/L (average)
- Women: 65-110 U/L (average)
- African descent: Often 50-100% higher than average

What Happens If Your CK Is High?
If your CK is above the upper limit of normal before starting a statin, your doctor might delay therapy - especially if you’re asymptomatic. But if you already have muscle pain and your CK is 3x or more above normal, that’s a warning sign. Here’s how doctors use CK levels after you start the drug:- CK under 3x ULN, no symptoms? Keep taking the statin. No action needed.
- CK 3-10x ULN with muscle pain? Stop the statin, wait, retest in a week. See a specialist.
- CK over 10x ULN? Stop the statin immediately. This is rhabdomyolysis territory.
Why Some Experts Say Skip It
Not everyone agrees. Some argue baseline CK testing causes more harm than good. Dr. John Kastelein, a leading European cardiologist, points to a Cochrane Review of nearly 48,000 patients. It found no difference in muscle injury rates between people who had baseline CK tests and those who didn’t. He says it leads to false alarms, unnecessary anxiety, and wasted money. Choosing Wisely Canada estimates baseline CK testing costs $14.7 million a year in their country - and only 1.2% of abnormal results changed how patients were treated. That’s a lot of money for very little impact. But here’s the flip side: in real-world practice, clinics that do baseline CK testing see 22% fewer unnecessary statin stops when patients report muscle pain. That’s huge. Stopping a statin in someone with heart disease can raise their risk of heart attack or stroke. Avoiding that is worth more than the cost of the test.What About Genetic Testing?
A gene called SLCO1B1 can make some people more likely to get muscle side effects from statins - especially simvastatin. About 12% of Europeans carry this variant. If you have it, your risk of myopathy goes up 4.5 times. Genetic testing sounds perfect, right? But it’s not ready for prime time. It’s expensive. Not widely available. And it doesn’t cover all cases. Plus, even if you don’t have the gene, you can still get muscle pain from statins - especially if you’re older or on multiple meds. For now, baseline CK remains the most practical tool we have - for the right people.
How to Get an Accurate Baseline CK Test
If you’re getting tested, make sure it’s done right. Otherwise, you’ll get a false high result.- Avoid intense exercise for 48 hours before the test. Even a long walk or heavy gardening can raise CK.
- Don’t get a muscle injection (like a vaccine or steroid shot) in the week before.
- Tell your doctor about all your medications - even supplements.
- Get the test done within 4 weeks before starting the statin. Too far out, and your numbers might not reflect your true baseline.
Who Shouldn’t Get Baseline CK Testing?
If you’re a healthy adult under 65, with no kidney disease, no other meds, no history of muscle issues, and you’re starting a low- or moderate-dose statin - you don’t need this test. Routine CK monitoring while on statins? Not recommended. The ACC, AHA, and ESC all agree: checking CK every few months in someone with no symptoms adds no value. It doesn’t prevent rhabdomyolysis. It just creates noise. The real goal is to keep you on your statin if it’s helping your heart - and stop it only when there’s real evidence of harm. Baseline CK helps with that. But only when used wisely.The Bottom Line
Baseline CK testing isn’t for everyone. It’s not a routine check. It’s a targeted tool for high-risk patients. If you’re in one of those groups - older, on multiple meds, with kidney issues or thyroid disease - get the test. It gives your doctor the data they need to make smart decisions. If you’re not in a high-risk group, skip it. Save the cost. Avoid the anxiety. Focus on how you feel. Muscle soreness? Talk to your doctor. Don’t assume it’s the statin. And don’t stop your medicine without checking. The best way to stay safe on statins isn’t more blood tests. It’s knowing your risk, understanding your body, and working with your doctor to make the right call - with or without a CK number.Do I need a baseline CK test if I’m starting a statin for the first time?
Only if you’re at higher risk - like being over 75, having kidney disease, taking interacting drugs like fibrates or amiodarone, having hypothyroidism, or having had muscle problems on statins before. For healthy, low-risk adults, it’s not needed.
Can a high CK level mean I can’t take statins at all?
Not necessarily. If your CK is high before starting, your doctor may delay therapy to rule out other causes - like recent exercise or an undiagnosed muscle condition. If no other reason is found, they might start a lower-dose statin or try a different type. Many people with elevated baseline CK can still tolerate statins safely.
Why do some labs say my CK is high when I feel fine?
Because normal CK levels vary a lot between people. Athletes, men, people of African descent, and even those who lifted weights a few days ago can have CK levels above the lab’s reference range - and still be perfectly healthy. That’s why your personal baseline matters more than the lab’s “normal.”
Does taking a statin always raise CK levels?
No. Most people’s CK levels stay the same or change very little. But studies show even asymptomatic people on high-dose statins can have small, harmless rises - around 20 U/L on average. That’s not dangerous. It’s just a sign the drug is having a minor effect on muscle cells, not causing injury.
What should I do if I get muscle pain after starting a statin?
Don’t stop the statin right away. Call your doctor. They’ll check your CK level and ask about your recent activity, other meds, and symptoms. In most cases, the pain isn’t from the statin. If your CK is under 3x the upper limit and you’re not severely weak, you can often keep taking it - maybe at a lower dose. Stopping unnecessarily raises your heart risk.
Is genetic testing better than CK testing for statin safety?
Genetic testing for SLCO1B1 can identify people at higher risk for simvastatin side effects, but it’s not widely used yet. It doesn’t catch all cases, and it doesn’t help with other statins or non-genetic causes of muscle pain. Baseline CK is still the most practical, real-world tool for most patients.
How much does a baseline CK test cost?
In most places, it costs between $20 and $50. But the bigger cost is what happens if you don’t do it: unnecessary statin discontinuation can lead to heart attacks, hospitalizations, and higher long-term care costs - estimated at $2,850 per avoided stop in secondary prevention patients.
Can I skip the test if I’m on a low-dose statin?
Yes - if you’re under 65, healthy, not on interacting drugs, and have no history of muscle issues. Low-dose statins carry a very low risk of muscle injury (under 0.1%). The risk-benefit ratio doesn’t justify routine testing in this group.




MARILYN ONEILL
19 January, 2026 12:55 PMWow. Just wow. I can't believe people still think this is a good idea. My cousin's doctor ordered this test and then told her she couldn't take statins because her CK was 'high'-turns out she'd done 200 squats the day before. This isn't medicine, it's guesswork with a lab coat. And now we're spending millions? Are we serious? I'm calling my senator.
Steve Hesketh
20 January, 2026 15:26 PMHey everyone, I just want to say-this post is beautiful. Truly. I'm from Nigeria, and here, most folks don't even have access to basic blood tests, let alone CK panels. But reading this? It made me feel seen. If you're lucky enough to have a doctor who listens, please don't let fear stop you. Statins saved my dad's life. And yeah, muscle aches? Happened to me too. But I kept going. Talked to my doc. Got my baseline. It wasn't about the number-it was about the conversation. You're not alone. 💪❤️
shubham rathee
21 January, 2026 15:07 PMif you think this is about health you are wrong its about money big pharma and labs make billions off these tests and they push it hard to doctors who dont even read the guidelines anymore its all about billing codes and quotas no one cares if you feel fine or not they just want the next test the next refill the next bill and you are just a number in their system dont believe me check your insurance statement next time you get a statin prescription
Kevin Narvaes
23 January, 2026 08:40 AMso like… is this all just… capitalism? like we’re all just lab rats in a system that wants us to be anxious about every tiny enzyme and pay for the privilege of being told we’re ‘fine’? i mean… if my body is making extra ck because i lifted weights or i’m black or i just walked to the fridge… isn’t that just… my body doing its thing? why do we need a permission slip from a machine to be allowed to live?
Dee Monroe
25 January, 2026 00:07 AMI’ve been thinking about this for weeks since my cardiologist mentioned baseline CK testing. It’s not just about the numbers-it’s about how we define normal. Who gets to decide what ‘normal’ is? Is it the lab’s reference range shaped by a 1980s study of mostly white men? Or is it your own body, your own rhythm, your own lived experience? I’m 58, I lift weights, I’m Indian-American, and my CK has always been 280. My doctor didn’t blink. He said, ‘That’s your normal.’ That’s the real win here-not the test itself, but the shift toward personalized care. We’re moving from population averages to individual stories. And that? That’s medicine worth having.
Melanie Pearson
26 January, 2026 11:32 AMIt is imperative to note that the American College of Cardiology, in conjunction with the American Heart Association, explicitly advises against routine baseline creatine kinase testing in asymptomatic individuals. The data is unequivocal. The expenditure of public healthcare resources on this practice is not only inefficient but potentially deleterious, as it fosters unnecessary medicalization and erodes patient trust in clinical judgment. This is not a fringe opinion-it is the consensus of evidence-based medicine.
Jerry Rodrigues
27 January, 2026 18:06 PMMy doc didn’t order it. I asked. I’m 72, on a statin, and had a bad reaction to one years ago. I just wanted to know where I stood. Got the test. My CK was 180. Started the new statin. Two weeks later, I felt weird. Got retested. 210. No big deal. Kept going. No issues. No drama. Just data. Sometimes simple is enough.
Jarrod Flesch
28 January, 2026 03:17 AMBeen a pharmacist for 18 years and I’ve seen this play out a hundred times. Baseline CK? Totally worth it for high-risk folks. But here’s the thing-most docs don’t even explain what to do with the number. I’ve had patients panic because their CK was ‘above normal’ and quit statins cold turkey. Then they come back with chest pain. So yeah, test if you’re in the risk group… but also make sure your doc knows how to interpret it. And maybe throw in a 🤝 emoji when you ask them to write it down. It helps.
Barbara Mahone
28 January, 2026 08:21 AMIn my community, many elders are afraid of statins because they’ve heard horror stories. This post helps. Not because it’s technical-it’s because it’s human. We don’t need more tests. We need more clarity. And someone who says, ‘It’s okay to feel unsure.’ Thank you for that.
Stephen Rock
30 January, 2026 06:00 AMCK testing is a scam. The entire system is rigged. You think your doctor cares about you? Nah. They care about their bonus tied to cholesterol numbers. The test is just a distraction. Real health is sleep, movement, and not eating plastic. But hey-go get your blood drawn. I’ll be here, lifting weights and laughing at the system.
Amber Lane
30 January, 2026 14:58 PMGot mine before starting. Was 210. Doc said, ‘You’re good.’ Kept the statin. No issues. No drama. Just a number. Saved me a year of guesswork.
Malvina Tomja
31 January, 2026 08:28 AMLet me be clear: if you're under 65, healthy, and not on other meds, getting this test is not just unnecessary-it's irresponsible. You're contributing to healthcare inflation. You're normalizing medical anxiety. You're validating a system that profits from fear. This isn't prevention. It's performance. And you're the audience.
Samuel Mendoza
31 January, 2026 19:44 PMWrong. The Cochrane Review says no benefit. End of story. If your doctor pushes this, they’re either ignorant or selling something. Don’t be the sucker who pays for a test that changes nothing.