You wake up with a throat on fire and a pounding in your sinuses. Maybe you’ve dealt with that UTI discomfort—sharp, persistent, impossible to ignore. Or it’s your kid, grumpy and spiking a fever that won’t budge. We live for those days when our bodies work like clockwork. But when bacteria slip in and start a party where they’re not invited, something’s got to kick them out. Enter Ceftin, the go-to fix in the world of prescription antibiotics, not the viral ones; only for the legit, lab-proven, bug-caused chaos. Here’s what separates Ceftin from the rest, and what you want to remember if it lands in your medicine cabinet.
What Is Ceftin and Why Are People Prescribed It?
Ceftin, known to your pharmacist as cefuroxime axetil, is an oral antibiotic from the cephalosporin family. It’s basically a bacterial bouncer. Once in your system, ceftin messes with bacteria’s ability to build their protective walls—no wall, no bacteria, no infection. But this isn’t a free-for-all magical cure. Doctors reach for Ceftin when they suspect bacteria, not viruses. Usually it’s prescribed for things like sinus infections, strep throat, tonsillitis, ear infections (hello, swimmer’s ear), bronchitis, skin stuff (think: cellulitis), UTIs, and even Lyme disease during its early phase. It’s not first choice for every infection—E. coli, Streptococcus, Klebsiella, and Haemophilus influenzae are no strangers to being booted out by Ceftin.
This isn’t just something they hand out loosely at urgent care; Ceftin is usually given after an assessment. Docs factor in things like if you’re allergic to penicillin, if the area you live in has lots of resistant bugs, and if you really have a bacterial infection (versus a viral imposter). Back in the day, Ceftin was a game-changer because it fixed things that plain old amoxicillin couldn’t always handle. Today, it’s often the backup when a simpler antibiotic isn’t cutting it—or, frankly, when penicillin is off the table because of an allergy.
It’s available in tablets (usually 250 or 500 mg) and also as an oral suspension for kids or folks who’d rather skip swallowing big pills. The number of days you take it changes depending on what you’re fighting—a classic 7-10 day course for most, shorter for urinary infections, and up to 20 days for certain cases like Lyme disease. Even the timing matters: you’re supposed to take it twice daily, after food, because it absorbs way better. Missed a dose? Take it when you remember, but if it’s close to the next dose, don’t double up. Overuse is how superbugs happen, and trust me, nobody wants those.
How Ceftin Works in Your Body
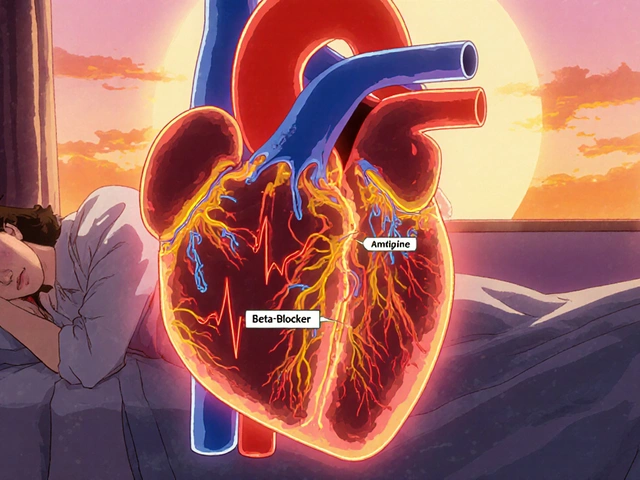
When you swallow that Ceftin tablet, your gut gets to work breaking down the axetil form into the useful cefuroxime. Around an hour or two later, it’s zipping through your bloodstream, on the lookout for unwanted bacterial squatters. The big highlight here is how Ceftin blocks the bacteria from building a cell wall. Human cells don’t have these walls, so Ceftin is like a targeted missile for bacteria, not your own cells. That’s what makes it pretty safe, and why its side effects are usually do-able for most people.
The kicker? Not all bacteria care. Some are basically immune to Ceftin (thanks to natural resistance or having met this drug’s cousins before). That’s why you’ll sometimes see your doctor run a swab, urine, or blood culture before picking an antibiotic. They want proof the bacteria in your case will actually tap out to cefuroxime. Prescribing the wrong antibiotic isn’t just a waste—it trains bacteria to become even bigger jerks down the line. It even comes with a scorecard: back in 2022, a CDC report showed about 35% of urinary E. coli resisted a common group of cephalosporins, making “know your bug, pick your drug” more important than ever.
If your infection is due to penicillin-allergy worries, Ceftin can step in most of the time. Its structure is different enough that true cross-reactions are rare (about 1% of penicillin-allergic folks also react), but doctors are careful all the same. Whether it’s ear, throat, lung, or urinary bugs, Ceftin goes to where it’s needed. Its levels peak rather quickly—about two hours after a dose. It’s cleaned out by the kidneys, so if yours work slower than most, your doc will tweak your dose. Skimping on water? That doesn’t help Ceftin either, so washing it down with a full glass makes sense.
There are newer generations of cephalosporins, but Ceftin’s sweet spot is that it covers a “goldilocks zone” of bacteria—not too broad (less harm to your gut microbes), but not too narrow either. It’ll never hit viruses—flu, COVID, and classic colds are untouched, so don’t let anyone talk you into keeping old Ceftin in your drawer “just in case.” You need a fresh prescription, specific to what you’re battling, every time.
Ceftin Side Effects: What to Watch Out For
No medicine is all upside. For Ceftin, most people breeze through a course with low-key issues, if any. The most common side effects are digestive—it’s not unusual for folks to report mild nausea, tummy pain, or feeling like something just isn’t sitting right. After all, your gut is filled with good bacteria, and antibiotics don’t have the best aim when it comes to the “bad only” bacteria. That’s why loose stools or mild diarrhea happen in about 10-15% of adults or kids.
More rarely, Ceftin makes people dizzy or gives them a headache. The rash risk? It’s real, but most rashes are more annoying than dangerous. That said, if itchy hives, swelling around your lips, or trouble breathing show up, that’s allergy territory. Drop everything, call for help, and list Ceftin as an allergy with your pharmacy and doctor from then on. Any severe side effect, especially swelling or trouble swallowing, is an emergency.
Another thing: just because you feel better after three days doesn’t mean the germs are gone. Stopping antibiotics too soon is why resistant bacteria are becoming more common. C. diff, a gut bug that thrives when other bacteria get wiped out, is also a known risk. Symptoms are watery diarrhea (sometimes with blood), belly cramps, and it can happen weeks after you finish antibiotics. If your gut goes wild after a course of Ceftin, don’t just chalk it up to bad luck—let your doctor know quickly.
Special populations need special care. If you’re pregnant, using Ceftin is usually considered safe in the second and third trimesters, but there isn’t tons of data on the first trimester. It does show up in breastmilk, but not in huge amounts, so pediatricians often say it’s fine for nursing. Be honest with your doc if you’re pregnant, breastfeeding, using hormonal birth control (since the old myth that antibiotics reliably mess with the pill isn’t totally backed up for Ceftin, but some absorbency issues with stomach upset can happen), or if you’re juggling other meds—blood thinners and antacids both can do some weird things with Ceftin in your body.
Tips for Taking Ceftin Safely and Getting the Best Results
If you’re handed a Ceftin prescription, a little know-how goes a long way. Always, always take it with food. Skipping that step can mess with how much actually gets into your bloodstream, and you want all of it targeting those germs. Stay consistent: keep the doses as evenly spaced apart as possible, usually every 12 hours. Turn on an alarm if you have to. Forgetting doses or missing days doesn’t just slow down your recovery—it’s how bacteria learn to fight back.
Don’t chew, crush, or break the tablets. That outer coating plays a big role in how the drug’s absorbed, and cracking them open messes with the timing. Oral suspension needs a shake before each dose to guarantee the right mix. Trust the pharmacy—once mixed with water, the liquid version usually keeps for under 10 days in the fridge. Toss it when it expires, and give it a good shake before every use. For kids, use the included oral syringe or dosing cup, not your kitchen spoons.
If you take antacids, heartburn meds, or iron supplements, let your doctor or pharmacist know. These can mess with how Ceftin is absorbed, sometimes making it less effective. Best bet is to separate those by at least 2 hours from your dose. And if you take blood thinners—like warfarin—regular blood tests might need a closer look, because antibiotics can subtly affect how your body handles those meds.
Most importantly, finish the course—even if you feel like your old self halfway through. Skipping the last few doses risks a comeback from some sneaky leftover bacteria, now tougher to tackle. Watch for signs of an allergic reaction, and if you notice something off, reach out to your healthcare provider. Never share leftover Ceftin, and never start a new course without seeing your doctor—old, expired drugs lose their punch, and the bug you’re fighting now may not match what your last prescription was for.
Hydrate like you mean it. Your kidneys handle clearing this drug, so plenty of water helps keep things moving smoothly. And as with all antibiotics, consider your gut. Some people swear by eating probiotic-rich yogurt or taking a probiotic supplement, but timing is everything—take them hours apart from your antibiotic, or you’re just wasting your money.

Frequently Asked Questions and Lesser-Known Facts About Ceftin
Ever wonder if you can drink with Ceftin? Unlike some antibiotics—think Flagyl—Ceftin and alcohol don’t interact in a dangerous way. Still, heavy drinking isn’t great for your immune system, and your liver is already working overtime clearing this med and fighting infection. Maybe skip the happy hour until you’re feeling better.
If you miss a dose, the rule is simple: take it as soon as you remember, unless it’s almost time for your next one. Doubling up isn’t smart—it means more side effects, not better results. For those asking about driving, Ceftin isn’t known for making people sleepy or foggy. Unless you get dizzy as a side effect (which is rare), you should be good to go.
Ceftin doesn’t make you photosensitive, so sunlight isn’t a major danger, unlike with some other antibiotics. Another plus: it’s gluten free and safe for most folks with celiac disease, but it does contain lactose in the tablets, which might matter for people with severe lactose intolerance.
What about kids? Pediatricians often use Ceftin for stubborn ear infections, especially when amoxicillin didn’t do the trick or when there’s a penicillin allergy. They also count on it for sinus or skin infections in school-aged kids. The flavored suspension tries to mask the bitter taste, but calling it “tasty” is a stretch—have some juice or food handy for a chaser.
Travelers love asking if it’s good prophylaxis for traveler’s diarrhea. The answer: No. Not only does Ceftin not cover most causes, but its unnecessary use could ruin your gut bacteria for no reason. Save it for real, proven bacterial infections. And about the “superbug” talk—yes, misuse fuels resistance. Even one antibiotic dose you didn’t need can push bacteria to get stronger and more stubborn. That’s why doctors are all about matching the right drug to the right bug, not just handing out Ceftin for every sniffle or sore throat.





Gary Levy
13 August, 2025 20:33 PMNice overview — clear and practical. I appreciate that the piece stresses that Ceftin is for bacterial infections only and not some catchall cure for every sore throat or sniffle.
One thing I tell friends: if your doc prescribes an antibiotic, ask what they're targeting and how long the course should be. It cuts down on confusion and makes you less likely to stop early.
Also worth adding: if you get mild stomach upset, try taking the tablet with a small snack plus a full glass of water. Seems to help a bunch.
sourabh kumar
14 August, 2025 21:33 PMgood write up but people must not hoard antibiotics it is dangerous and pointless
i had neighbor who kept old pills in drawer and once used them for a sore throat not even sure it was bacterial
don’t do that
Christian Miller
16 August, 2025 01:20 AMThe summary is thorough, but I want to raise a cautious point: pharmaceutical repackaging and the incentives built into prescribing patterns deserve scrutiny.
Antibiotic selection is influenced by local resistance data, yes, but also by formularies, marketing, and habit. That combination sometimes nudges clinicians to favor drugs that are convenient to prescribe rather than strictly optimal for a given isolate.
Resistance trends cited in the article are worrying and should prompt patients to ask for culture confirmation where feasible. Broad prescribing without diagnostics accelerates resistance and increases the chance of adverse community-level outcomes.
Finally, electronic health records and automated prompts can help, but they can also create blind spots where practitioners rely on defaults. Vigilance is warranted.
Julius Adebowale
17 August, 2025 05:06 AMNot worth keeping leftover meds.
KISHORE KANKIPATI
18 August, 2025 08:53 AMGreat deep dive — thanks for writing this up. A few practical points from someone who's been through the antibiotic maze with kids and elderly parents.
First, the suspension for children: measure carefully. Kitchen spoons are unreliable, and a half-teaspoon variance every dose adds up fast. Use the syringe the pharmacy gives or buy a dedicated dosing spoon. Label the bottle with the time you mixed it and the discard date — pharmacies often print it but it's easy to lose track when life gets busy.
Second, antibiotics and the pill: the traditional panic about all antibiotics wrecking oral contraceptives mostly overstates the risk for many drugs, but the real issue is vomiting or diarrhea. If your child or partner is seasick after a dose or has prolonged diarrhea, that can reduce absorption and you should use backup contraception or consult a clinician.
Third, probiotics — yes, but timing matters. Take a probiotic several hours after the antibiotic. Many people cram them together and wonder why nothing helped. Yogurt with live cultures can be comforting, but for real recovery after a course, a multi-strain supplement for a few weeks is often more reliable for adults, and pediatric formulations exist for kids.
Fourth, renal dosing. The article mentions dose tweaks for kidney function; follow them. Elderly folks often clear drugs slower, and double dosing can lead to unnecessary side effects. If you see dizziness or odd neuro symptoms, check renal function and ask about dose adjustment.
Fifth, watch for rashes that appear a week or more after starting. Not all allergic reactions are immediate. I've seen delayed rashes that led to stopping the medication; they weren't life-threatening but unpleasant. Any swelling or breathing trouble is an emergency, obviously.
Sixth, storage: liquid suspension usually keeps about 10 days in the fridge; mark that date. Toss anything left afterwards. Tablets should be kept dry and cool; a bathroom medicine cabinet often makes them degrade faster than a bedroom drawer.
Seventh, interactions: antacids, iron supplements, and certain nutritional shakes can lower absorption. Space them by two hours where possible. If you're on warfarin, let your prescriber know — short courses can change INR in some people and monitoring may be needed.
Eighth, if symptoms aren't improving within 48–72 hours, call back. Sometimes the bug is resistant or there's another issue like an abscess that needs drainage. Don’t assume antibiotics always fix everything without follow up.
Ninth, if you or a family member has a documented severe penicillin allergy, Ceftin is sometimes used cautiously but make sure the allergy is verified. Old notes saying "allergic" without detail can lead to unnecessary avoidance or risky exposure. A clear history helps.
Tenth, education matters. Tell whoever is taking it why they’re taking it, the exact schedule, and what to expect. People who know what to watch for are less likely to stop early or misuse the drug. That’s simple but powerful in preventing resistance.
Finally, use antibiotics as tools not talismans. They are lifesaving when used right; they become a problem when treated as a routine fix for everything. Ask questions, follow instructions, and keep the conversation going with your clinician if anything seems off.
Jefferson Vine
19 August, 2025 12:40 PMAgree with the resistance concerns, but let's not pretend doctors are clueless or that there's some grand scheme to overprescribe — many are balancing patient expectations, time pressure, and imperfect data.
That said, patients should push back when an antibiotic is suggested for a likely viral illness. Ask for reasoning, ask for tests, and if you must take an antibiotic, get clear instructions about monitoring and follow-up.
Also this: pharmacy pricing and insurance tiers sometimes push one antibiotic over another. If cost is an issue, ask about generics and if a cheaper option is appropriate. There isn't a one-size-fits-all answer, but informed patients fare better.
Donna Oberg
20 August, 2025 16:26 PMOh my god, yes!!! Thank you for saying this!!!
Doctors, please explain things properly. Please write down dose times, interactions, and how to know if it’s working or not. I can’t tell you how many times I’ve seen people sent home with a prescription and no instructions and then panic halfway through the course.
Also!!! If someone in the house gets a rash or swelling, do not wait, do not "see how it goes" — go to the ER. Allergies escalate SO fast. I mean it.
Garreth Collard
27 August, 2025 15:06 PMNice read, though I come away imagining antibiotics as both savior and slow poison — a delicious irony.
There’s a social choreography to medicine: the handshake between prescriber and patient, the quiet ritual of a pill swallowed, the small domestic art of measuring a suspension in the kitchen. These are mundane acts but they carry consequence. Use them deliberately.
Also, for those traveling soon, remember that throwing antibiotics at every tummy upset cheats you of the chance to let your microbiome adapt naturally. Only use when clearly necessary.
Daniel LaMontagne
4 September, 2025 17:33 PMGood post — concise and helpful 🙂
One tiny add: if taking with dairy for the taste, try to keep it a couple hours from the dose just in case — better safe than sorry.