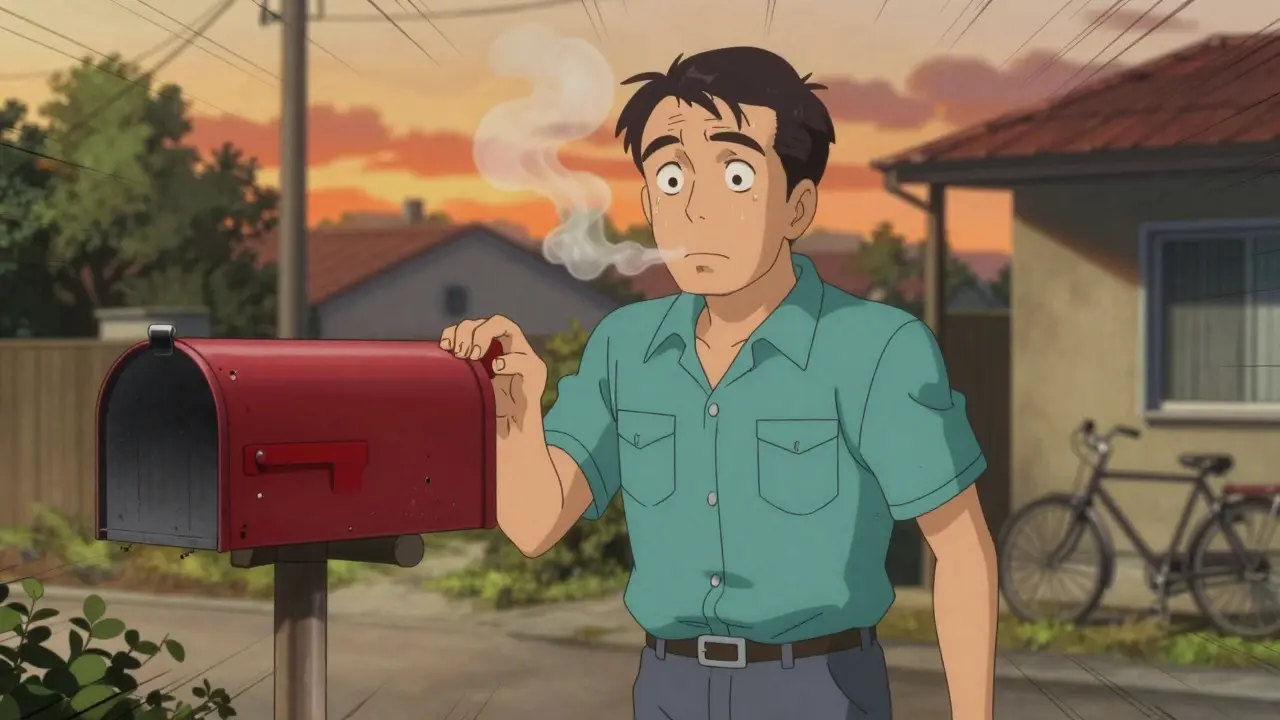
Most people don’t realize they have COPD until it’s already advanced. By then, simple things like walking to the mailbox or tying shoes leave them gasping. The truth? COPD doesn’t sneak up overnight. It creeps in slowly, and if you’re over 40 and smoke-or used to smoke-those little signs of breathlessness aren’t just "getting older." They could be the first stage of something serious.
What COPD Really Means
Chronic Obstructive Pulmonary Disease isn’t one condition. It’s a group of lung diseases that make it hard to breathe because your airways are narrowed and damaged. Most cases are caused by smoking, but long-term exposure to fumes, dust, or pollution can also trigger it. The damage is permanent, but it doesn’t have to get worse fast. The key is catching it early.
The Global Initiative for Chronic Obstructive Lung Disease (GOLD), formed by experts from around the world, created the standard way to measure COPD severity. It’s not just about how bad you feel. It’s about hard numbers from a simple breathing test called spirometry. This test measures how much air you can blow out in one second-called FEV1. Your result is compared to what’s normal for someone your age, height, sex, and ethnicity. If your FEV1 is below 80% of predicted, and your FEV1/FVC ratio is under 70% after using a bronchodilator, you have COPD.
Stage 1: Mild COPD
Stage 1 means your FEV1 is 80% or higher. Sounds okay, right? But here’s the catch: you might already be having symptoms. About 65% of people in this stage get short of breath only during fast walking or climbing hills. Nearly half have a daily cough with phlegm. Many ignore it. They think, "I’m just out of shape." Or, "I’m not as young as I used to be."
That’s the problem. If you’re in Stage 1 and keep smoking, your lungs decline at about 60 mL per year. Quit smoking, and that drops to 30 mL per year. That’s a 50% slowdown in damage. Pulmonary rehab isn’t usually recommended yet, but it can help. And yes-getting the flu shot matters. Studies show it cuts your risk of flare-ups by 32%.
One man in Durban, 58, started wheezing after his morning walk. His doctor said, "You’re fine, just get more exercise." He didn’t get tested. Two years later, his FEV1 dropped to 68%. He was now in Stage 2. If he’d had that spirometry test at 58, he could’ve changed the course of his disease.
Stage 2: Moderate COPD
This is where things start to feel real. FEV1 drops to 50-79%. Now, you’re stopping to catch your breath every few minutes on level ground. Eighty-three percent of people here say they can’t walk without pausing. Mucus production increases. You’re more likely to get sick, and when you do, it hits harder.
Treatment changes. You’re no longer just using a rescue inhaler when you need it. You’ll likely start a long-acting bronchodilator-either a LABA or LAMA. These aren’t quick fixes. They work all day to keep your airways open. In the UPLIFT trial, patients on these medications improved their FEV1 by 100-150 mL on average. That’s not just a number. It means you can walk farther, carry groceries, maybe even play with your grandkids without feeling like you’re drowning.
And here’s the surprise: 38% of people classified as "high risk" in the GOLD ABCD system actually have Stage 2 COPD. Their symptoms are worse than their lung numbers suggest. That’s why doctors now use two tools: the COPD Assessment Test (CAT) and the mMRC dyspnea scale. If your CAT score is 10 or higher, or you’re on mMRC level 2 or above, you’re in a higher risk group-even if your FEV1 is still in Stage 2.
One Reddit user, u/BreathlessInSeattle, wrote: "I can’t walk to my mailbox (20 feet) without stopping. My FEV1 is 38%, but my doctor says I’m 'only' Stage 3. So I must be exaggerating." That’s the disconnect. The numbers don’t tell the whole story. Your experience matters. If you’re struggling, you’re not imagining it.
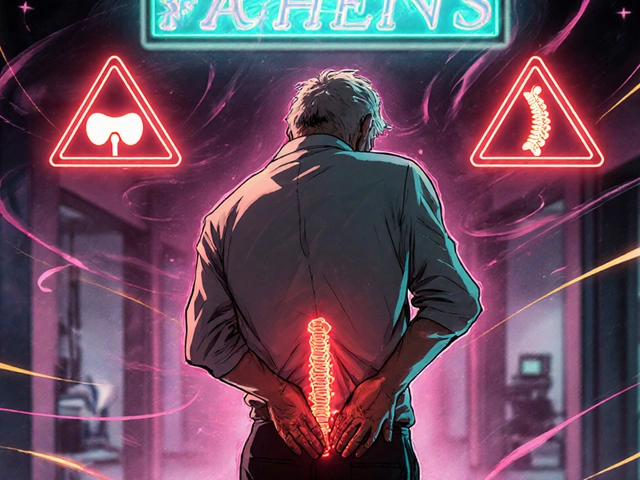
Stage 3: Severe COPD
FEV1 is now between 30% and 49%. This is where daily life changes. Ninety-two percent of people here get winded just putting on clothes or showering. Oxygen levels drop during routine tasks. Many need supplemental oxygen for short periods, even if they don’t need it full-time yet.
Treatment gets more aggressive. You’ll probably be on a combination of two long-acting bronchodilators-LAMA and LABA together. The SUNSET trial showed this combo cuts moderate-to-severe flare-ups by 14% compared to one drug alone. If your blood eosinophil count is above 300 cells/μL, you might also get an inhaled steroid. The WISDOM trial found this reduces flare-ups by 25% in people with that marker.
But here’s what no one talks about enough: your heart. Dr. Don Sin from the University of British Columbia found that 65% of Stage 2 COPD patients already have heart disease. By Stage 3, it’s even worse. COPD isn’t just a lung disease. It’s a whole-body condition. That’s why doctors now check for high blood pressure, irregular heartbeat, and signs of heart failure alongside your lung numbers.
One patient in Cape Town, 67, started using oxygen for 2 hours a day after walking. She didn’t think it was serious until she had a heart attack. Her COPD had been silently straining her heart for years. After adding cardiac rehab to her plan, her hospital visits dropped by 60%.
Stage 4: Very Severe COPD
FEV1 is below 30%. This stage is life-altering. Eighty-nine percent of people here need oxygen for more than 15 hours a day. Simple tasks become impossible. Walking across the room? Exhausting. Eating a meal? Takes two hours. Many stop leaving the house.
Long-term oxygen therapy isn’t optional. The NOTT trial showed that if you use oxygen 15+ hours a day, your one-year survival rate jumps from 73% to 90%. That’s not a small difference. It’s the difference between being in bed all day and being able to sit outside with your family.
Non-invasive ventilation (NIV) is another tool. It’s not a ventilator with a tube down your throat. It’s a mask that helps you breathe better while you sleep. Studies show it cuts hospital readmissions by 28%. For many, it means staying out of the ER during flare-ups.
But the hidden crisis? Cost. The American Lung Association found that 52% of Stage 4 patients pay $287 a month out-of-pocket for oxygen equipment-even with Medicare. In places like South Africa, where public health systems are stretched thin, many just go without. That’s not just expensive. It’s deadly.
Why Early Detection Is Everything
Only 12.3% of people over 40 who smoke get spirometry tested when they have symptoms. That’s a massive gap. And here’s the kicker: 42% of primary care doctors misread spirometry results because they weren’t trained properly.
AI is starting to help. At Massachusetts General Hospital, AI-assisted spirometry cut staging errors by 35%. But technology won’t fix the problem if people don’t get tested.
Dr. MeiLan Han says most patients delay diagnosis by 5.2 years. They think their breathlessness is normal. But if you catch COPD in Stage 1 or 2, you can slow progression by half. That’s not a guess. That’s from clinical trials.
What You Can Do Right Now
- If you smoke, quit. Today. No delay. Your lungs will thank you.
- If you’re over 40 and have a cough, wheeze, or get winded easily, ask for a spirometry test. Don’t wait for your doctor to bring it up.
- Get the flu shot every year. It’s not just for kids.
- If you’re diagnosed, join a pulmonary rehab program. It’s not gym class. It’s structured breathing and exercise that helps you live better.
- Track your symptoms. Use a notebook or app. Write down when you get short of breath, how often you cough, and how much mucus you produce.
COPD doesn’t have to be a death sentence. But it won’t fix itself. And it won’t wait.
Can COPD be reversed?
No, the lung damage from COPD can’t be reversed. But you can stop it from getting worse. Quitting smoking, taking prescribed medications, doing pulmonary rehab, and avoiding triggers like smoke and pollution can keep your lung function stable for years-even decades. Many people with Stage 1 or 2 COPD never progress to severe stages if they act early.
How do I know if I have COPD and not just asthma?
Asthma usually starts in childhood and comes and goes. COPD builds slowly over time, especially in people over 40 with a smoking history. The key test is spirometry with a bronchodilator. In asthma, lung function improves significantly after the inhaler. In COPD, improvement is much smaller or nonexistent. A doctor can tell the difference with the right test.
Is COPD only caused by smoking?
Most cases are, but not all. Long-term exposure to secondhand smoke, dust, fumes, or air pollution can also cause COPD. In some parts of the world, burning wood or coal for cooking is a major cause. Even if you never smoked, if you’ve been around these things for years, you could still have COPD.
Do I need oxygen if I’m diagnosed with COPD?
Not everyone. Oxygen is only needed if your blood oxygen levels are low, which usually happens in Stage 3 or 4. Your doctor will check this with a simple test called pulse oximetry or an arterial blood gas test. If your levels are normal at rest and during activity, you don’t need oxygen-even if you’re in Stage 4. Using oxygen when you don’t need it won’t help and can be dangerous.
Can I still live a normal life with COPD?
Yes, if you manage it well. Many people with Stage 1 and 2 COPD live full lives-working, traveling, spending time with family. Even in Stage 3 and 4, with the right treatment, oxygen, and rehab, people stay active and independent. It’s not about the stage. It’s about what you do next. Quitting smoking, staying active, and following your treatment plan can make a huge difference.
What Comes Next
The future of COPD care is moving beyond just FEV1 numbers. Blood tests for biomarkers like fibrinogen are being studied to predict how fast your lungs decline. New drugs are targeting inflammation pathways specific to COPD. And AI is helping doctors read spirometry more accurately.
But none of that matters if you don’t get tested. If you’ve been ignoring your breathlessness, thinking it’s just age or laziness-it’s not. Your lungs are telling you something. Listen before it’s too late.