When older adults receive sedatives or pain meds, their bodies don’t process them the same way they did when they were younger. Their liver slows down, their kidneys filter less, and their brains become more sensitive to drugs. This means a dose that’s safe for a 40-year-old could put an 80-year-old at risk of stopping breathing - quietly, and without warning. Over-sedation isn’t dramatic. It doesn’t always come with slurred speech or falling asleep. Often, it starts with a slow, shallow breath. If you’re caring for an elderly loved one or working in a medical setting, knowing how to catch these early signs can mean the difference between a routine procedure and a life-threatening event.
Why Seniors Are at Higher Risk
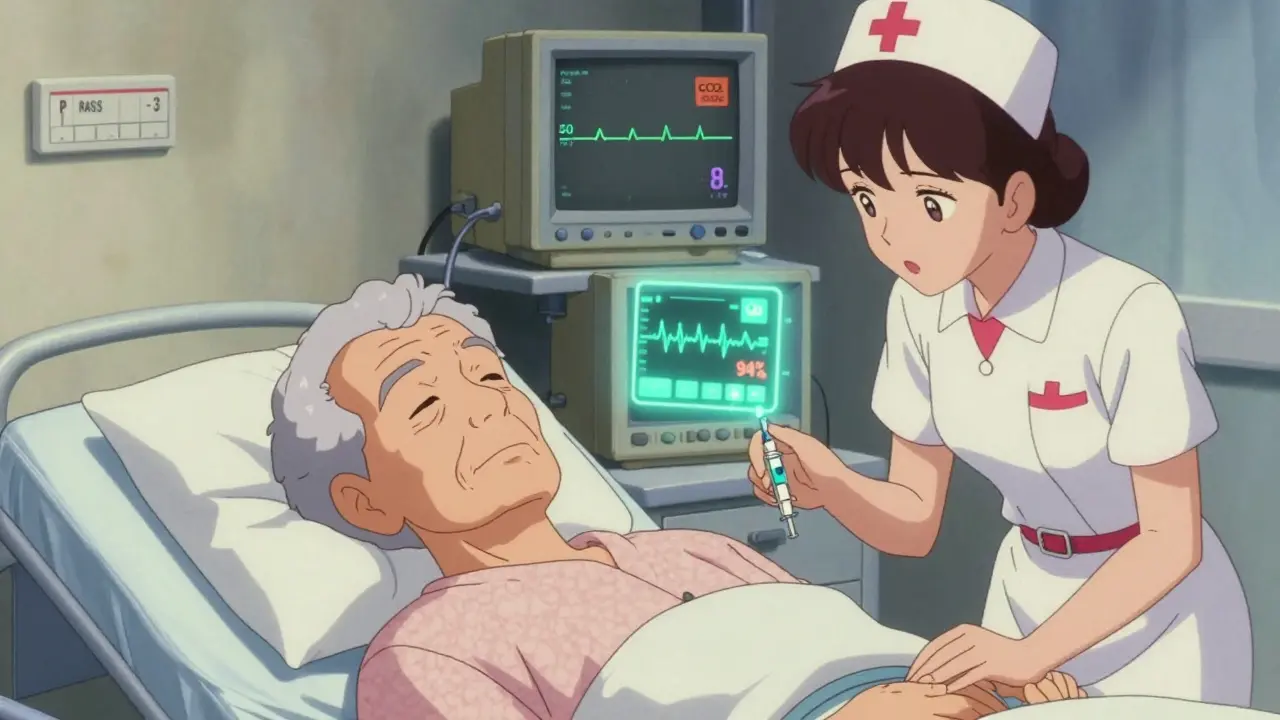
People over 65 are 3.5 times more likely to suffer serious sedation-related problems than younger adults. Why? It’s not just about taking too much medicine. It’s about how their bodies change with age. The liver’s ability to break down drugs drops by 30% to 50% between ages 20 and 80. Kidneys clear medications 0.8 mL per minute less each year after age 40. At the same time, the blood-brain barrier becomes more porous, letting more drug into the brain. Even small doses can have big effects. A 2023 report found that 65% of all respiratory arrests during sedation happen in seniors, even though they make up only about 16% of the population undergoing these procedures.
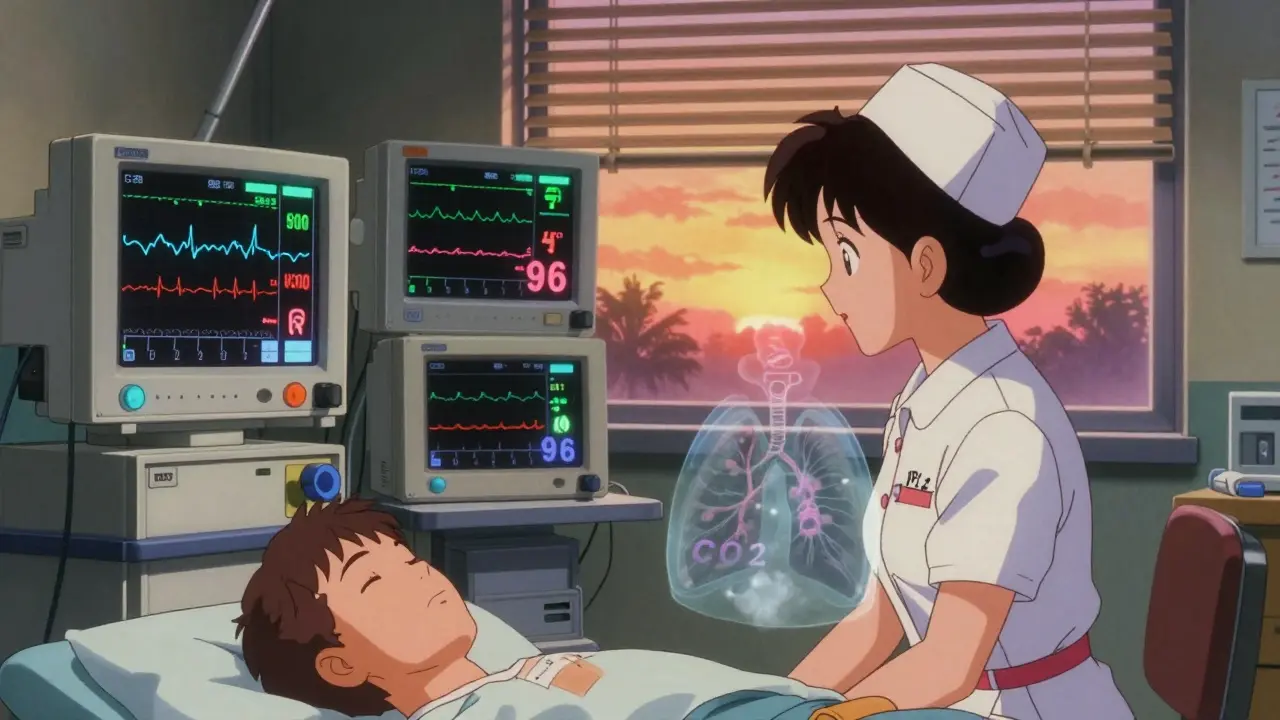
Another hidden danger? Supplemental oxygen. Many seniors get oxygen during procedures because they have COPD or heart issues. But oxygen can mask the real problem - low breathing. A patient might have an SpO2 reading of 96% and look fine, while their carbon dioxide levels are climbing dangerously. Without checking more than just oxygen, you’re flying blind.
The Five Vital Signs You Must Watch
Monitoring isn’t just about one number. It’s about watching five key signs together. Here’s what you need to track - and what numbers mean trouble:
- Pulse Oximetry (SpO2): Keep above 92%. If it drops below 90%, act immediately. But don’t rely on this alone. Oxygen can hide low breathing.
- Respiratory Rate: Normal is 12-20 breaths per minute. Below 8 breaths per minute? That’s a red flag. Seniors often breathe slower when sedated, but 8 or fewer means their body is shutting down.
- End-Tidal CO2 (EtCO2): This measures how much carbon dioxide the patient is exhaling. Normal range is 35-45 mmHg. If it rises above 50, they’re not breathing well enough to clear CO2. If it drops below 30, they may be holding their breath. Capnography - the device that measures this - is the single most important tool for detecting trouble before oxygen levels fall.
- Heart Rate: Should stay between 50 and 100 beats per minute. Below 50 or above 100 can signal stress, low oxygen, or drug toxicity.
- Blood Pressure: Systolic pressure should stay above 90 mmHg. A sudden drop can mean the body is failing to compensate for low breathing.
These numbers matter most when you watch them continuously. Checking every 5 minutes misses 78% of dangerous events, according to a 2019 study. Continuous monitoring catches problems early - often 10 to 15 minutes before a patient turns blue.
The Gold Standard: Multimodal Monitoring
Using just one tool - like a pulse oximeter - is like trying to drive with only your rearview mirror. You need all the windows. The best practice is multimodal monitoring: combining at least three measurements.
Here’s what works:
- Capnography + Pulse Oximetry: This combo is the minimum standard for seniors. Capnography catches breathing problems 92% of the time. Pulse oximetry catches low oxygen. Together, they reduce false alarms and catch silent hypoxia.
- Integrated Pulmonary Index (IPI): This smart algorithm takes capnography, respiratory rate, SpO2, and heart rate, and gives you one number from 1 to 10. Below 7? That’s a warning. A 2021 study of over 1,200 seniors showed IPI predicted trouble 12.7 minutes before oxygen dropped. One nurse on Reddit shared how her 82-year-old patient’s IPI dropped to 5.2 during a colonoscopy - they intervened, and the patient never desaturated.
- Richmond Agitation-Sedation Scale (RASS): This isn’t a machine. It’s a simple way to check how alert someone is. RASS scores range from +4 (agitated) to -5 (unresponsive). A score of -2 or lower means moderate to deep sedation. At -3 or below, you need to stop the procedure and reassess. A 2022 Mayo Clinic study cut oversedation by 41% just by using RASS with capnography.
Some places use BIS (Bispectral Index) monitors, which measure brain activity. They can reduce oversedation by 37%, but they cost over $1,200 per unit and need training. For most settings, capnography and RASS are enough.
What Not to Do
Many mistakes happen because people trust machines too much - or not enough.
- Don’t ignore capnography alarms. In seniors, 38% of capnography alarms are false - because their breathing is irregular. But if you silence them all, you’ll miss the real ones. Always check: Is the patient breathing? Are they moving? Is their skin color changing?
- Don’t rely on intermittent checks. Checking vitals every 5 minutes misses the critical window. Continuous monitoring isn’t optional anymore. The Joint Commission and CMS require it for reimbursement.
- Don’t use adult dosing. A 70-year-old doesn’t need the same dose as a 30-year-old. Use this formula: Age-adjusted dose = standard dose × (1 - 0.005 × (age - 20)). For an 80-year-old, that’s 30% less. Yet, 42% of facilities still use standard adult doses.
- Don’t assume oxygen means safety. A senior on oxygen with SpO2 at 95% can still be in respiratory arrest. Their body is holding its breath. Only capnography shows that.
Practical Tips for Caregivers and Staff
If you’re at home or in a clinic, here’s how to stay ahead:
- Know the signs: Slowed breathing, confusion, unresponsiveness, pale or bluish lips, cold skin.
- Use hydrocolloid dressings: If using electrodes for monitoring, fragile skin can break down. These special bandages reduce skin injury by 67%.
- Train your team: Even nurses with years of experience need 8 hours of training to interpret RASS and capnography correctly. Inter-rater reliability for RASS is 0.87 - meaning if two trained staff check the same patient, they’ll agree 87% of the time.
- Keep a log: Write down vitals every 2 minutes during sedation. Look for trends: Is respiratory rate dropping slowly? Is EtCO2 creeping up? Trends matter more than single numbers.
- Have naloxone ready: If you suspect opioid overdose, have naloxone (Narcan) on hand. It can reverse the effect in minutes.
What’s New in 2026
The field is moving fast. In May 2023, the FDA approved a new system called the Opioid Risk Monitoring System (ORMS). It links IV pain pumps with capnography and pulse oximetry. If the patient’s breathing drops below 8 breaths per minute, the pump stops automatically. In trials, it cut respiratory depression by 58% in seniors.
Next up? AI-powered prediction. Researchers are training algorithms to spot subtle changes in breathing patterns, heart rate, and oxygen levels - predicting trouble 20 minutes before it happens. The goal? To move from reaction to prevention.
But no tool replaces a trained person. The 2023 NCEPOD report says this clearly: "Technology alone cannot compensate for inadequate staffing ratios." One nurse per patient remains the safest standard.
Final Thoughts
Monitoring seniors for over-sedation isn’t about technology. It’s about attention. It’s about knowing that a slow breath, a quiet patient, or a steady SpO2 reading might be the last warning before disaster. Capnography, RASS, and continuous observation aren’t luxuries - they’re the bare minimum. And when you combine them with proper dosing and trained staff, you don’t just prevent overdose. You give seniors the safety they deserve.
What are the first signs of over-sedation in seniors?
The earliest signs are often subtle: slower breathing (fewer than 8 breaths per minute), reduced responsiveness (RASS score of -2 or lower), pale or cool skin, and lack of movement. Unlike younger patients, seniors rarely groan or thrash. They just go quiet. If they stop responding to gentle stimulation - like a touch on the shoulder - it’s time to act.
Can pulse oximetry alone detect over-sedation in seniors?
No. Pulse oximetry measures oxygen in the blood, not breathing effort. Seniors on supplemental oxygen can maintain SpO2 above 94% even while their breathing slows to dangerous levels. This is called "silent hypoxia." Capnography is needed to detect rising carbon dioxide - the true sign of respiratory depression.
Why is capnography so important for elderly patients?
Capnography measures carbon dioxide exhaled, which directly reflects breathing rate and depth. In seniors, it detects respiratory depression 92% of the time - compared to 67% for pulse oximetry alone. It gives a 12- to 14-minute early warning before oxygen drops. For a 75-year-old with COPD, this can be the difference between a safe procedure and a cardiac arrest.
How should medication doses be adjusted for seniors?
Use the formula: Adjusted dose = standard dose × (1 - 0.005 × (age - 20)). For example, a 70-year-old should receive 75% of the standard adult dose. Studies show that 42% of facilities still use full adult doses, putting seniors at unnecessary risk. Always start low and go slow.
What should I do if I suspect an overdose in a senior?
Stop all sedatives immediately. Call for help. Check airway and breathing. If breathing is shallow or absent, start rescue breathing. Administer naloxone (Narcan) if opioids are involved - it can reverse the effect within minutes. Continue monitoring even after they wake up - effects can rebound. Always document the event and review the dosing and monitoring protocol.





Brad Ralph
13 February, 2026 09:34 AMSo basically, if your grandma’s breathing slower than a sloth on vacation, you’re doing it right? 😅
christian jon
14 February, 2026 15:42 PMI can’t believe we’re still debating this! Capnography isn’t a luxury-it’s a moral imperative! If your facility isn’t using it, you’re basically playing Russian roulette with your elderly relatives! 🚨💔 And don’t even get me started on the fact that 42% of hospitals are still using adult doses-this isn’t medicine, it’s negligence dressed in scrubs!
Suzette Smith
14 February, 2026 23:54 PMHonestly? I think capnography is overrated. My dad’s been on oxygen for 10 years and he’s fine. Maybe we’re just overmedicalizing aging?
Autumn Frankart
16 February, 2026 22:53 PMYou know who benefits from all this monitoring? The companies selling the devices. Capnography? RASS? IPI? All part of a $30B healthcare industrial complex designed to keep seniors hooked to machines while the real issue-understaffing and profit-driven care-is ignored. They don’t want you to notice the nurse-to-patient ratio is 1:8. They want you to think it’s about the tech.
Skilken Awe
17 February, 2026 23:04 PMYou people are so naive. Pulse oximetry? Capnography? Please. The real issue is that pharmaceutical companies have been pushing opioids on seniors since the 90s under the guise of 'pain management.' The FDA approved ORMS? That’s just the next step in the corporate lock-in. Wake up. This isn’t medicine-it’s a supply chain.
Carla McKinney
19 February, 2026 03:16 AMThe formula for age-adjusted dosing is mathematically sound, but it assumes linear pharmacokinetics, which is flawed. In reality, hepatic metabolism isn’t linear-it’s exponential, especially in frail elderly. Also, RASS has poor inter-rater reliability in dementia patients. You’re not addressing confounders. This entire framework is built on shaky evidence.
Ojus Save
20 February, 2026 00:33 AMi think capnography is cool but i dont think every old person needs it. my uncle just sits there naps and its fine. maybe we just need more tea and less machines??
Jack Havard
21 February, 2026 17:31 PMAll this monitoring? It’s just a distraction. The real problem is that we’ve turned caregiving into a checklist. You don’t need a machine to notice someone’s not breathing. You need to look them in the eye. And if you’re too busy to do that, maybe you shouldn’t be in charge.
Luke Trouten
22 February, 2026 17:05 PMThere’s a quiet dignity in how we’ve come to treat aging. We’ve replaced human presence with algorithms and monitors. But the truth is, no device can replace the weight of a hand on a shoulder, or the pause before a breath. The most vital sign isn’t on the screen-it’s in the silence between heartbeats, and whether someone still feels seen.
Gabriella Adams
23 February, 2026 03:38 AMI’ve worked in geriatrics for 18 years. Let me tell you: the single most effective tool is not capnography or RASS-it’s presence. A nurse who stays 10 minutes longer. A family member who asks, 'How are you feeling right now?' That’s what prevents disaster. The tech helps-but it doesn’t replace the human who shows up.
Vamsi Krishna
23 February, 2026 14:55 PMYou ever notice how every time someone mentions naloxone, the conversation instantly turns into a morality play? We’re not talking about addiction here-we’re talking about accidental overdose in a hospital. But no, let’s just blame the opioids. The real villain? The fact that we don’t train staff to recognize the difference between sedation and stupor. We’re medicating the symptoms and ignoring the system.
Steve DESTIVELLE
24 February, 2026 23:02 PMThe entire premise of this post is built on a flawed assumption-that aging is a medical problem to be solved rather than a natural process to be honored. We have reduced the dignity of the elderly to a set of vital signs to be optimized. We measure their breaths like a machine measures engine RPM. But what happens when the machine fails? What happens when the nurse is distracted? What happens when the elderly person is simply tired of being monitored? We forget they are human beings-not data points. The real crisis is not over-sedation-it is the erosion of compassion in care.