Escitalopram Risk Assessment Tool for Elderly Patients
Risk Assessment
This tool evaluates key safety concerns when prescribing escitalopram to elderly patients. Enter patient details to receive risk assessment and management recommendations.
Risk Assessment Results
Recommended Actions
Quick Takeaways
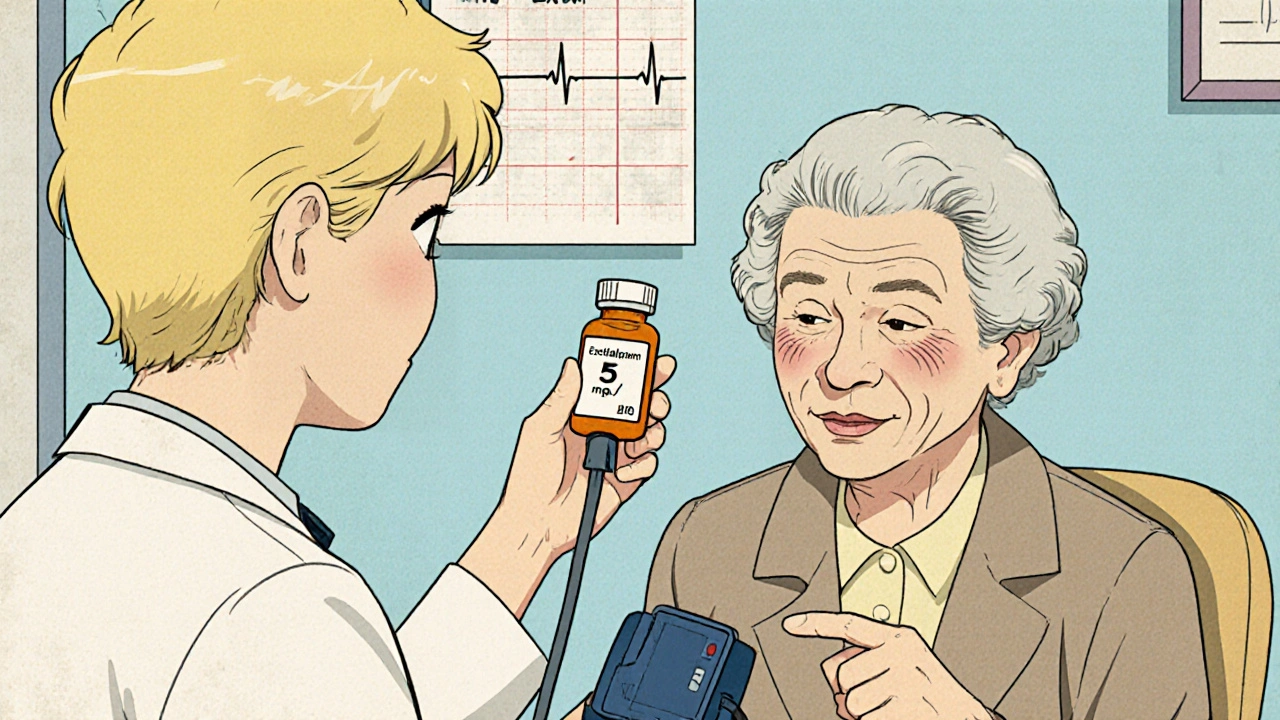
- Start low (5 mg) and increase slowly; monitor blood pressure, sodium, and heart rhythm.
- Watch for hyponatremia, especially in patients on diuretics or with low water intake.
- Check the QT interval on an ECG if the patient has cardiac disease or takes other QT‑prolonging drugs.
- Mind the CYP2C19 pathway - many common meds (e.g., omeprazole) can raise escitalopram levels.
- Re‑evaluate effectiveness after 4-6 weeks; adjust only when side‑effects are under control.
What is Escitalopram?
Escitalopram is a selective serotonin reuptake inhibitor (SSRI) prescribed for depression and generalized anxiety disorder. It works by increasing serotonin availability in the brain, which helps lift mood and reduce worry. In clinical trials, it shows similar efficacy to other SSRIs but with a slightly cleaner side‑effect profile, a reason many clinicians choose it for older adults.
Why Seniors React Differently to SSRIs
Age‑related changes in liver function, body fat composition, and kidney clearance all tweak how drugs behave. The elderly often have reduced activity of the enzyme CYP2C19, the primary pathway that metabolises escitalopram. Lower enzyme activity means the drug stays longer in the bloodstream, raising the risk of toxicity.
Poly‑pharmacy is another reality. A typical 75‑year‑old may be taking antihypertensives, anticoagulants, and a statin, each with the potential to interact with the SSRI. Even over‑the‑counter sleep aids can shift the balance.
Key Safety Concerns in the Elderly
Three safety signals dominate the conversation:
- Hyponatremia - Low sodium can cause confusion, falls, and seizures. SSRIs, including escitalopram, increase antidiuretic hormone release, which can dilute sodium levels, especially in patients on thiazide diuretics.
- QT prolongation - Certain SSRIs can lengthen the heart’s electrical recovery period. In seniors with existing cardiac disease, a prolonged QT interval raises the chance of a dangerous arrhythmia called torsades de pointes.
- Drug interactions - The CYP2C19 pathway overlaps with many common medications (e.g., omeprazole, clopidogrel, certain anti‑arrhythmics). Interactions can either spike escitalopram levels or diminish its effect.
Managing Hyponatremia Risk
Before starting escitalopram, obtain a baseline serum sodium. Re‑check after two weeks and again after six weeks. If sodium drops below 130 mmol/L, consider reducing the dose or switching to an SSRI with a lower reported hyponatremia rate, such as sertraline.
Encourage patients to maintain adequate fluid intake but avoid excessive water consumption, which can worsen dilutional hyponatremia.
QT Prolongation: When to Order an ECG
If the patient has a history of myocardial infarction, heart failure, or is on other QT‑prolonging drugs (e.g., certain antibiotics, anti‑emetics), obtain a baseline ECG. Look for a corrected QT (QTc) over 450 ms. If the baseline is borderline, repeat the ECG after reaching the target dose.
Should the QTc exceed 500 ms, stop escitalopram and switch to an alternative antidepressant with minimal cardiac effects.
Drug‑Interaction Checklist
Use this quick list every time you prescribe or adjust escitalopram in an older adult:
- Anticoagulants (warfarin, apixaban) - monitor INR or factor Xa levels.
- Antiplatelet agents (clopidogrel) - beware of reduced antiplatelet activity via CYP2C19 inhibition.
- Proton‑pump inhibitors (omeprazole, esomeprazole) - can raise escitalopram plasma concentrations.
- Tricyclic antidepressants - increase the risk of serotonin syndrome.
- Antipsychotics (quetiapine, ziprasidone) - additive QT prolongation.
When any of these are present, consider starting at 5 mg daily and extending the titration interval to three weeks.
Dosage and Titration for Seniors
Guidelines suggest a starting dose of 5 mg once daily, especially for patients over 65 or those with hepatic impairment. After two weeks, assess tolerability and increase to 10 mg if needed. The maximum recommended dose in older adults is usually 20 mg, but many clinicians never exceed 10 mg because the therapeutic response often plateaus.
Always counsel patients to take the pill at the same time each day, preferably in the morning to avoid nighttime insomnia, a common SSRI side‑effect.
Choosing the Right SSRI: A Quick Comparison
| Feature | Escitalopram | Sertraline | Citalopram |
|---|---|---|---|
| Typical starting dose | 5 mg daily | 25 mg daily | 10 mg daily |
| Half‑life | ≈27 hours | ≈26 hours | ≈35 hours |
| Metabolism pathway | CYP2C19, CYP3A4 | CYP2D6, CYP3A4 | CYP2C19 |
| Risk of hyponatremia | Moderate | Low | High |
| QT prolongation | Low‑moderate | Low | High (dose‑dependent) |
| Common drug interactions | CYP2C19 inhibitors | SSRIs, antiplatelets | CYP2C19 inhibitors |
When cardiac risk or hyponatremia is a concern, sertraline often emerges as the safer choice because of its low impact on sodium balance and QT interval.
Monitoring Plan After Initiation
Set up the following schedule:
- Week 1: Verify dose, ask about nausea or insomnia.
- Week 2: Check serum sodium and blood pressure.
- Week 4: Repeat ECG if any cardiac history, evaluate mood improvement.
- Month 2 and beyond: Continue sodium checks every 3 months, adjust dose based on response and side‑effects.
Document any adverse events in the electronic health record, linking them to the medication start date to aid future prescribing decisions.
When to Discontinue or Switch
If the patient develops:
- Severe hyponatremia (Na < 125 mmol/L) - stop immediately, correct electrolytes, and consider an alternative SSRI.
- QTc > 500 ms - discontinue; switch to sertraline or venlafaxine, which have a lower cardiac profile.
- Serotonin syndrome (agitation, hyperreflexia, fever) - emergent care, stop all serotonergic agents.
- Unremitting gastrointestinal upset after 2 weeks - lower dose or try a non‑SSRI antidepressant.
Practical Tips for Clinicians
- Use a medication reconciliation worksheet at each visit; seniors often forget over‑the‑counter supplements.
- Educate caregivers about early signs of low sodium (headache, confusion) and when to call.
- Leverage pharmacy alerts for CYP2C19 interactions; many community pharmacies now flag high‑risk combos.
- Consider a brief deprescribing trial after 6 months if mood remains stable - less medication often means fewer falls.
Frequently Asked Questions
Can escitalopram cause falls in older adults?
Yes. The drug can lead to dizziness, orthostatic hypotension, or hyponatremia, each of which raises fall risk. Monitoring blood pressure and sodium, and starting at a low dose, helps reduce this danger.
Is it safe to combine escitalopram with a proton‑pump inhibitor?
PPIs like omeprazole inhibit CYP2C19, which can raise escitalopram levels. If a PPI is necessary, keep escitalopram at the lowest effective dose and monitor for increased side‑effects.
How long does it take for escitalopram to work in seniors?
Most patients notice mood improvement after 4-6 weeks, but physical side‑effects may appear within the first two weeks. Patience and regular follow‑up are key.
Should I order an ECG for every elderly patient on escitalopram?
Only if the patient has cardiac disease, a history of arrhythmia, or is taking other QT‑prolonging drugs. For low‑risk patients, a baseline ECG is optional.
What is the best alternative if escitalopram is not tolerated?
Sertraline is often the go‑to alternative because it has a lower hyponatremia rate and minimal QT impact. Venlafaxine is another option, though it belongs to a different drug class (SNRI).





Angela Koulouris
21 October, 2025 12:43 PMYour thorough breakdown gives clinicians a solid roadmap; the incremental dosing visual feels like a safety net for seniors.
Xavier Lusky
2 November, 2025 17:13 PMWhat they hide is the pharma push behind every "low start" recommendation, steering us toward perpetual prescriptions.
Ashok Kumar
14 November, 2025 22:43 PMI get why you’d worry-nothing like a sodium dip to ruin a good day, right? The guidelines sound sensible, but the reality is often messier.
eric smith
27 November, 2025 04:12 AMLet me break it down for you: you don’t need to reinvent the wheel, just follow the standard titration charts-obviously.
Jake Hayes
9 December, 2025 09:42 AMYour suggestion is naïve and dangerous.
parbat parbatzapada
21 December, 2025 15:12 PMThey dont tell u that every time you sip water they are logging your electrolytes to sell data.
Chirag Muthoo
2 January, 2026 20:41 PMIt is commendable that clinicians maintain vigilance; early detection of hyponatremia can dramatically improve outcomes.
Harry Bhullar
15 January, 2026 02:11 AMWhen you start an SSRI in an octogenarian, the pharmacokinetic landscape shifts dramatically, and every milligram counts.
First, the hepatic CYP2C19 activity often declines, which means the drug’s half‑life can stretch beyond the quoted 27 hours.
Second, the volume of distribution increases because of higher body fat, so plasma concentrations linger.
Third, concomitant medications like omeprazole act as competitive inhibitors, pushing escitalopram levels upward.
Because of these factors, a 5 mg initiation is not just a guideline but a safety imperative.
Within two weeks you should obtain a sodium panel, because dilutional hyponatremia is a stealthy cause of confusion and falls.
If the sodium drops below 130 mmol/L, consider either a dose reduction or a switch to sertraline, which has a more favorable hyponatremia profile.
Parallel to labs, an ECG should be ordered if the patient has any history of myocardial infarction, heart failure, or is on another QT‑prolonging agent.
A baseline QTc over 450 ms warrants a repeat after reaching the target dose; exceeding 500 ms is a clear stop signal.
Drug‑interaction checklists are indispensable; beyond PPIs, you must watch out for anticoagulants, antiplatelet agents, and certain anti‑arrhythmics.
Warfarin, for example, may require INR monitoring adjustments because escitalopram can potentiate its effect.
Clopidogrel’s antiplatelet activity can be blunted through CYP2C19 inhibition, raising thrombotic risk.
From a clinical workflow perspective, integrate pharmacy alerts and a medication reconciliation worksheet at each visit.
Educating caregivers about early hyponatremia signs-headache, mild disorientation-can preempt emergency department visits.
Finally, after six months of stable mood response, a structured deprescribing trial may reduce fall risk without sacrificing therapeutic benefit.
All these steps together form a proactive, layered safety net that transforms a simple prescription into a comprehensive geriatric care plan.
Dana Yonce
27 January, 2026 07:41 AMI love how the monitoring schedule lays everything out clearly 😊.
Lolita Gaela
8 February, 2026 13:10 PMThe utilization of a QTc threshold integrates electrophysiological risk stratification, while serial serum sodium assessments operationalize a proactive electrolyte management algorithm-key components of a geriatric pharmacovigilance framework.