Parkinson's Treatment Selector
Enter Your Information
Recommended Treatment:
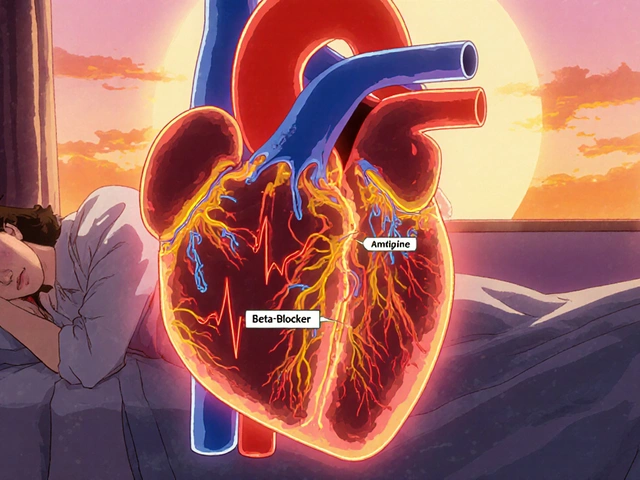
When treating Parkinson’s disease, Sinemet is a fixed‑dose combination of carbidopa and levodopa. It’s been the go‑to therapy for decades because it replenishes dopamine while protecting levodopa from premature breakdown.
Quick Take
- Sinemet remains the most proven levodopa‑based option, but long‑term use can lead to motor fluctuations.
- MAO‑B inhibitors (selegiline, rasagiline) add a mild dopamine boost without needing levodopa.
- Dopamine agonists such as ropinirole and pramipexole work earlier in the disease and may delay levodopa start.
- COMT inhibitors (entacapone, opicapone) extend levodopa’s effect when added to Sinemet.
- Non‑drug options like deep‑brain stimulation are reserved for advanced cases where meds no longer control symptoms.
How Sinemet Works
Carbidopa is a peripheral DOPA decarboxylase inhibitor. By blocking the enzyme outside the brain, it prevents levodopa from turning into dopamine too early, allowing more of the drug to cross the blood‑brain barrier. Levodopa is the metabolic precursor of dopamine. Once inside the brain, levodopa is converted into dopamine, easing the motor symptoms of Parkinson’s disease such as tremor, rigidity, and bradykinesia.
Because both ingredients are combined in a single tablet, dosing is simpler, but the fixed ratio can limit flexibility for patients who need a higher carbidopa‑to‑levodopa balance.
Major Alternatives at a Glance
Below are the most commonly considered alternatives, grouped by their primary mechanism.
Dopamine Agonists
Ropinirole is an oral non‑ergot dopamine agonist. It stimulates D2/D3 receptors directly, providing symptom relief without introducing levodopa. Common side effects include nausea, dizziness, and occasional impulse‑control issues.
Pramipexole is another non‑ergot dopamine agonist with a slightly longer half‑life. It’s often used when patients experience early‑stage symptoms or need to delay levodopa onset. Like ropinirole, it can cause sleep attacks and compulsive behaviors.
Rotigotine delivers dopamine agonist action through a transdermal patch. The patch provides steady plasma levels, which helps reduce “off” periods. Skin irritation is the most frequent complaint.
MAO‑B Inhibitors
Selegiline is a selective mono‑amine oxidase‑B inhibitor. By blocking MAO‑B, it slows the breakdown of endogenous dopamine, offering modest motor improvement. At higher doses it can act as a weak levodopa substitute.
Rasagiline is a newer MAO‑B inhibitor with once‑daily dosing. Clinical trials show it may delay the need for levodopa in early Parkinsonism, and it carries a low risk of hypertensive crisis when used alone.
COMT Inhibitors (Adjuncts to Levodopa)
Entacapone inhibits catechol‑O‑methyltransferase (COMT) in the periphery. Adding it to Sinemet extends levodopa’s half‑life, smoothing out “on” peaks and reducing “off” time. Diarrhea and orange‑colored urine are typical side effects.
Opicapone is a once‑daily COMT inhibitor with a longer duration of action than entacapone. It offers similar benefits with fewer dosing hassles, though it can also cause dyskinesia when levodopa levels become too high.
Other Pharmacologic Options
Safinamide combines reversible MAO‑B inhibition with glutamate modulation. It’s approved as an add‑on for patients already on levodopa, improving motor fluctuations while possibly reducing dyskinesia.
Apomorphine is a potent dopamine agonist used as a rapid‑onset rescue injection. It’s reserved for sudden “off” episodes and requires careful titration because of nausea and hypotension.
Non‑Drug Therapies
Deep Brain Stimulation (DBS) involves surgically implanted electrodes that modulate abnormal brain activity. DBS can dramatically reduce medication‑related side effects and improve motor control in advanced disease, but it carries surgical risks and requires postoperative programming.
Side‑by‑Side Comparison
| Therapy | Primary Mechanism | Typical Form | Usual Max Daily Dose | Common Side Effects | Main Advantage | Key Limitation |
|---|---|---|---|---|---|---|
| Sinemet (Carbidopa/Levodopa) | Dopamine precursor + peripheral decarboxylase inhibition | Oral tablet | Up to 4,000mg levodopa per day (in divided doses) | Nausea, orthostatic hypotension, dyskinesia | Most potent symptomatic relief | Motor fluctuations & dyskinesia with long‑term use |
| Ropinirole | Dopamine D2/D3 agonist | Oral tablet | 24mg per day | Somnolence, impulse‑control issues, nausea | Delays need for levodopa | Less robust symptom control in advanced disease |
| Pramipexole | Dopamine D2/D3 agonist | Oral tablet | 4.5mg per day | Edema, hallucinations, compulsive behaviors | Long half‑life, smooth symptom coverage | Potential psychiatric side effects |
| Rasagiline | Selective MAO‑B inhibitor | Oral tablet | 1mg per day | Headache, dizziness | Once‑daily dosing, low dietary restrictions | Modest efficacy when used alone |
| Entacapone | Peripheral COMT inhibitor (add‑on) | Oral tablet | 200mg with each levodopa dose | Diarrhea, orange urine | Extends levodopa “on” time | Increases risk of dyskinesia |
| Opicapone | Long‑acting COMT inhibitor (add‑on) | Oral tablet | 50mg once daily | Dyskinesia, constipation | Once‑daily dosing simplifies regimen | Similar dyskinesia risk as entacapone |
| Deep Brain Stimulation (DBS) | Electrical modulation of subthalamic nucleus or GPi | Surgical implantation | Not applicable | Infection, hardware malfunction | Reduces medication burden, improves motor fluctuations | Invasive, requires ongoing device management |
How to Choose the Right Option for You
Think of the decision as a checklist rather than a single factor. Ask yourself:
- What stage of Parkinson’s am I in? Early stages often benefit from dopamine agonists or MAO‑B inhibitors, while later stages usually require levodopa‑based therapy.
- How sensitive am I to side effects? If nausea or impulsive‑control issues are a concern, a lower‑dose agonist or a patch may be preferable.
- Do I need simplicity? Once‑daily dosing (e.g., opicapone, rasagiline) reduces pill burden, which matters for busy lives.
- Am I planning surgery? If DBS is on the horizon, some clinicians aim to keep levodopa doses modest to avoid severe dyskinesia that can complicate programming.
- What are my financial constraints? Generic carbidopa/levodopa is inexpensive, whereas newer agents or DBS can be significantly costlier.
Bring this list to your neurologist. A shared‑decision conversation ensures the chosen regimen matches your lifestyle, disease progression, and budget.
Practical Tips & Common Pitfalls
- Start low, go slow. When adding a dopamine agonist, begin with the smallest dose to gauge tolerance.
- Watch for “off” periods. If you notice the medication wears off before the next dose, discuss adding a COMT inhibitor.
- Mind diet with MAO‑B inhibitors. At therapeutic doses, they rarely interact with tyramine‑rich foods, but high doses can still cause headaches.
- Monitor for impulse‑control disorders. Gambling, binge eating, or hypersexuality can emerge with agonists; report any changes early.
- Keep a symptom diary. Logging on/off times, side effects, and activity levels helps your doctor fine‑tune the regimen.
Frequently Asked Questions
Is Sinemet still the best first‑line drug for Parkinson’s?
For most patients, yes. Levodopa provides the strongest symptom relief, and carbidopa reduces peripheral side effects. However, doctors may start with a dopamine agonist in younger patients to postpone levodopa‑related dyskinesia.
Can I mix Sinemet with a dopamine agonist?
Yes, many clinicians combine a low dose of levodopa with a dopamine agonist to smooth out motor fluctuations while keeping overall levodopa exposure low.
What’s the difference between entacapone and opicapone?
Both block COMT, but opicapone lasts longer and is taken once daily, whereas entacapone must be taken with each levodopa dose. Opicapone’s longer action can improve adherence.
Are MAO‑B inhibitors safe to use with Sinemet?
They can be combined, but the total dopamine boost may increase the risk of dyskinesia. Dosage adjustments are usually needed.
When should I consider deep‑brain stimulation?
DBS is typically recommended after several years of medication when “off” periods become frequent or dyskinesia limits daily activities. A multidisciplinary evaluation determines candidacy.






Sondra Johnson
30 September, 2025 12:24 PMOkay but let’s be real - Sinemet is the OG for a reason. I’ve been on it for 8 years and it’s the only thing that lets me hold a coffee cup without my hand turning into a claw. The dyskinesia? Yeah, it’s a beast. But I’d rather dance with the devil than sit in an ‘off’ state watching my own body betray me.
Chelsey Gonzales
30 September, 2025 13:04 PMim so tired of people actin like sinemet is the only option… i tried ropinirole and it was like a miracle for my tremors. no dyskinesia, no nausea, just… calm. why do docs always push the big guns first??
MaKayla Ryan
1 October, 2025 03:02 AMUgh. Another one of those ‘alternatives are just as good’ posts. Newsflash: if you’re not on levodopa, you’re not treating Parkinson’s - you’re just pretending to manage it. This isn’t yoga. This is neurology. Get real.
Kelly Yanke Deltener
2 October, 2025 13:02 PMI just want someone to tell me why my insurance won’t cover opicapone but will pay for 10 different generic SSRIs? I’m not even mad, I’m just… heartbroken. Like, I’m dying slowly and they’re arguing over a $3 copay.
Sarah Khan
4 October, 2025 11:13 AMThe real question isn’t which drug works best - it’s which version of yourself you’re willing to become to keep moving. Levodopa gives you motion but steals your dignity in waves. Agonists give you peace but whisper madness in your ear. COMT inhibitors stretch the moment, but never the meaning. And DBS? That’s not medicine - that’s installing a remote control on your nervous system. We’re not choosing treatments. We’re choosing who we become when the tremors stop.
Kelly Library Nook
6 October, 2025 01:12 AMThe data presented here lacks proper statistical normalization across patient cohorts. The efficacy metrics for dopamine agonists are conflated with early-stage bias. Furthermore, the omission of longitudinal dyskinesia incidence curves renders the comparison statistically invalid. This is not clinical guidance - it’s marketing fluff dressed as medical advice.
Crystal Markowski
7 October, 2025 21:47 PMIf you’re just starting out, don’t rush into Sinemet. I waited two years before going on it, and I’m so glad I did. My motor symptoms are still manageable, and I haven’t had a single episode of impulse control issues. You’ve got time - use it to learn, to track, to talk to others who’ve been there. You’re not behind. You’re preparing.
Charity Peters
8 October, 2025 06:47 AMI use the rotigotine patch. It’s messy but it works. No more counting pills. Just slap it on and forget about it. My husband says I smell like a pharmacy now, but I don’t care.
Faye Woesthuis
8 October, 2025 13:37 PMIf you’re not on Sinemet, you’re not serious about fighting this disease. End of story.
raja gopal
10 October, 2025 05:15 AMMy father in India started on rasagiline because Sinemet was too expensive. He’s 72, walks with a cane, but still plants tomatoes every spring. Medicine isn’t just pills - it’s dignity. Thank you for writing this. It gives hope to people who can’t afford the ‘best’.
Samantha Stonebraker
10 October, 2025 08:28 AMThere’s something sacred about the way the patch sticks to your skin - like a quiet promise that today, your body will still listen to you. I used to hate the idea of being tethered to a device, but now? It’s my little armor. And yes, I sometimes cry when I peel it off at night. Not from pain. From gratitude.
Kevin Mustelier
10 October, 2025 17:39 PMDBS is basically like putting a Tesla autopilot on your brain. Cool? Sure. But who’s gonna fix it when it glitches? 😅 Also, anyone else notice the author didn’t mention amantadine? Like… come on.
Keith Avery
10 October, 2025 22:20 PMLet’s be honest - this entire post is just a glorified pharmaceutical ad. You missed the fact that levodopa accelerates neurodegeneration long-term. You ignored the role of gut microbiome in dopamine metabolism. And you completely omitted the benefits of high-dose CoQ10 and ketogenic diets. This isn’t medicine - it’s corporate propaganda.
Luke Webster
11 October, 2025 03:00 AMI’m from Nigeria originally, moved to the US for treatment. Back home, we used to make herbal teas from moringa and ginger - not a cure, but it eased the stiffness. Here, I’m on Sinemet and opicapone. I don’t see it as ‘Western vs traditional’ - I see it as ‘what keeps me alive today’. We all deserve access to whatever works, no matter the label.
Natalie Sofer
12 October, 2025 18:18 PMjust a quick note - if you're on entacapone and your pee turns orange, dont panic. it's totally normal. i thought i was dying the first time it happened. my mom called 911. we all live and learn. 😅
Tiffany Fox
13 October, 2025 05:12 AMTrack your on/off times. Seriously. Even just a note on your phone. It makes your neurologist’s job 10x easier - and you’ll feel heard. I did this for 6 months and we finally fixed my dosing. It changed everything.
Orion Rentals
13 October, 2025 19:03 PMThank you for the comprehensive overview. I particularly appreciate the structured comparison table and the emphasis on patient-centered decision-making. As a clinician, I find that the most effective outcomes occur when patients are equipped with clear, evidence-based options rather than being steered toward the most profitable or convenient therapy. The inclusion of non-pharmacological considerations - including financial constraints and lifestyle - is not merely thoughtful, it is essential to ethical neurologic care. I will be sharing this with my patients.