When you switch from a brand-name drug to a generic version, most people don’t notice a difference. That’s because generics are required by law to work the same way as the original. But for some, even small changes in how a medicine is made can cause noticeable effects. That’s why monitoring your health after switching to generics isn’t just a good idea-it’s necessary for certain conditions.
Why Some People Notice a Difference
Generics contain the same active ingredient as brand-name drugs, at the same strength and dose. The U.S. Food and Drug Administration (FDA) requires them to be bioequivalent, meaning they deliver the same amount of medicine into your bloodstream within the same time frame. So why do some people feel different? The answer lies in inactive ingredients. These are the fillers, dyes, and binders that hold the pill together or help it dissolve. While they don’t treat your condition, they can affect how quickly the medicine is absorbed. For most people, this doesn’t matter. But for those taking drugs with a narrow therapeutic index-like warfarin, levothyroxine, or seizure medications-even a slight change in absorption can throw off their balance. Take levothyroxine, for example. It’s used to treat hypothyroidism. A 2022 FDA report found that 12% of patients switching to a different generic version reported changes in energy, weight, or heart rate. These weren’t random side effects-they were signs their thyroid hormone levels had shifted. The same pattern shows up with lamotrigine, an antiepileptic drug, where 9% of patients experienced increased seizures after switching.Who Needs to Be Extra Careful
Not everyone needs to monitor closely. But if you’re taking one of these types of medications, pay attention:- Anticoagulants like warfarin (Coumadin) - small changes can increase bleeding risk or cause clots
- Thyroid meds like levothyroxine - even a 5% difference in absorption can affect your metabolism
- Anti-seizure drugs like phenytoin, carbamazepine, or lamotrigine - too little can trigger seizures; too much can cause dizziness or toxicity
- Immunosuppressants like cyclosporine or tacrolimus - used after transplants, these require precise blood levels
- Certain antidepressants like bupropion - some users report mood swings or reduced effectiveness after switching
The American Heart Association and the American Academy of Family Physicians both recommend extra monitoring for these drugs. If you’re on any of them, don’t assume the switch is harmless.
What to Track After the Switch
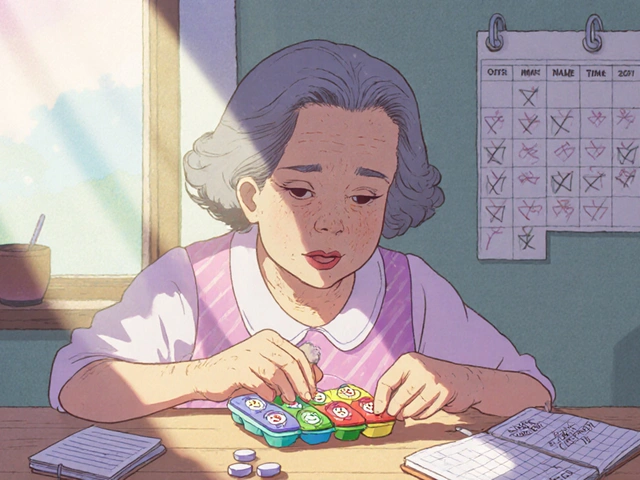
The first 30 days after switching are the most important. Here’s what to watch for:- Symptoms - Are your original symptoms returning? Are new ones showing up? Keep a simple journal: write down how you feel each morning and night.
- Lab values - If you’re on warfarin, check your INR at 7 days and again at 30 days. If you’re on levothyroxine, get your TSH tested at 4-6 weeks. For diabetes, check your HbA1c at 8 weeks.
- Physical signs - Unexplained weight gain or loss, heart palpitations, tremors, fatigue, or mood swings can all signal a problem.
- Medication appearance - Note the shape, color, and imprint on the pill. If your pharmacy switches to a different generic manufacturer, the pill might look different. That’s normal-but if your symptoms change at the same time, it’s worth reporting.
Consumer Reports found that 24% of people who switched to generics started tracking their health more closely. The most common metrics? Blood pressure (38%), blood sugar (29%), and seizure frequency (17%). If you’re on a high-risk drug, do the same.
How to Verify Your Generic
Not all generics are made the same. Even if two pills have the same active ingredient, they can come from different manufacturers with different formulations. That’s why checking the National Drug Code (NDC) matters. Every pill bottle has an NDC number-usually a 10- or 11-digit code on the label. Write it down when you first get your generic. If you refill and the number changes, that means you got a different brand of generic. It’s not a mistake-it’s just how the system works. But if your symptoms change after that switch, it could be related. The FDA’s Orange Book lists which generics are considered therapeutically equivalent to brand-name drugs. You can look up your drug there to see which versions are approved as interchangeable. But even if a generic is rated “AB,” that doesn’t guarantee you won’t react differently. The system works for populations-not individuals.When to Call Your Doctor
You don’t need to panic if you feel a little off. But here are signs you should reach out:- Your symptoms return or worsen within 2 weeks of switching
- You develop new side effects that weren’t there before
- Your lab results show a significant change (e.g., INR outside target range, TSH up or down by more than 20%)
- You have a seizure, fainting episode, or unusual bleeding
Don’t stop your medication. Don’t switch back without talking to your doctor. Instead, schedule a quick visit. Bring your pill bottle, your symptom log, and your NDC number. Most doctors will run a quick test and decide whether to switch you back or adjust the dose.
Reporting Problems Helps Everyone
If you think your generic isn’t working right, report it. The FDA’s MedWatch program collects reports from patients like you. In 2022, over 1.2 million adverse event reports were filed-but only about 15% involved generics. Most of those were minor. But when someone reports a real issue-like a seizure triggered by a new generic-it helps the FDA spot patterns. If multiple people report the same problem with the same NDC number, the FDA can investigate the manufacturer. That’s how unsafe batches get pulled. You can report online at www.fda.gov/medwatch or call 1-800-FDA-1088. Be specific: include the drug name, NDC number, lot number (found on the bottle), when you started the new version, and what happened. The FDA commits to reviewing serious reports within 30 days.What the Data Really Shows
Let’s be clear: for 9 out of 10 people, switching to generics makes no difference at all. A 2022 study by PatientsLikeMe tracked 42,315 people who switched. 92.7% had no change in symptoms. Only 1.2% needed medical help. On Reddit’s r/Pharmacy, a review of 1,247 user stories found that 78% noticed nothing. 19% saw minor changes-like a different pill shape or a slight stomach upset. Only 3% reported real problems. The bottom line? Generics are safe, effective, and save billions every year. But medicine isn’t one-size-fits-all. For the small group who do react, monitoring is the key to catching issues early.Final Checklist: Your 30-Day Monitoring Plan
Here’s a simple plan to follow after switching:- Day 1 - Note the NDC number and pill appearance. Write down your current symptoms and baseline lab values if applicable.
- Days 2-7 - Track daily symptoms. Are you sleeping better? More tired? Any new aches or mood shifts?
- Day 14 - If you’re on a high-risk drug (warfarin, thyroid, seizure meds), schedule a lab test.
- Day 30 - Review your journal. Compare symptoms to before the switch. If anything’s off, call your doctor.
- Day 90 - Even if you feel fine, check in with your provider. Some changes take longer to show up.
Switching to generics is smart financially and medically-for most people. But if you’re in the small group that’s sensitive to formulation changes, staying alert can prevent serious problems. Don’t ignore your body. Track, report, and speak up. Your health is worth it.
Are generic medications less effective than brand-name drugs?
No, generic medications are required by the FDA to be therapeutically equivalent to brand-name drugs. They must contain the same active ingredient, strength, dosage form, and route of administration. Bioequivalence studies show they deliver the same amount of medicine into the bloodstream at the same rate. Over 90% of prescriptions in the U.S. are generics, and studies confirm they work just as well for most people.
Can switching to a generic cause side effects?
Yes, but rarely. Side effects from generics are usually caused by inactive ingredients-like dyes or fillers-that differ from the brand-name version. These can cause mild issues like stomach upset or headaches in sensitive individuals. Serious side effects are uncommon, but if you notice new or worsening symptoms after switching, track them and talk to your doctor.
Which medications should I be careful about switching to generics?
Be extra cautious with drugs that have a narrow therapeutic index: warfarin, levothyroxine, phenytoin, carbamazepine, lamotrigine, cyclosporine, tacrolimus, and bupropion. These require precise blood levels, and even small changes in absorption can affect how well they work or increase the risk of side effects. Always monitor closely when switching these.
How long should I monitor my health after switching to a generic?
For most people, 30 days is enough. But if you’re on a high-risk medication, monitor for up to 90 days. For drugs like warfarin or levothyroxine, get lab tests at 7-14 days and again at 30 days. Keep a symptom journal during this time. If everything stays stable after 90 days, you’re likely fine.
What should I do if I think my generic isn’t working?
Don’t stop taking it. Instead, write down your symptoms, the pill’s NDC number, and when you switched. Call your doctor and schedule a check-up. They may order a blood test or switch you back temporarily. If you believe the issue is with the medication itself, report it to the FDA via MedWatch. Your report helps protect others.





Mira Adam
27 November, 2025 17:05 PMLet’s be real - if your body starts acting up after a generic switch, it’s not ‘in your head.’ It’s pharmacology, not placebo. The FDA’s ‘bioequivalent’ label is a statistical average, not a guarantee for your individual physiology. You’re not paranoid - you’re paying attention. And that’s more than most people do.
Jonah Thunderbolt
28 November, 2025 11:10 AMWow. Just… wow. 🤯 I switched to generic levothyroxine last month and suddenly I was weeping uncontrollably at dog videos 🐶😭 - turns out my TSH spiked 47% 📈. My endo said ‘it’s probably stress.’ I said ‘no, the pill changed.’ She sighed and ordered a new lab. 💅💊 #PharmaIsNotMagic
Rebecca Price
29 November, 2025 07:57 AMIt’s heartening to see someone articulate this so clearly. For those of us managing chronic conditions, the transition to generics isn’t just a cost-saving measure - it’s a clinical experiment we didn’t consent to. Tracking symptoms, NDC codes, and lab values isn’t ‘overthinking’ - it’s self-advocacy. And frankly, it’s a responsibility we shouldn’t have to shoulder alone.
shawn monroe
29 November, 2025 21:58 PMAs a clinical pharmacist with 18 years in med management, let me break this down: NARROW THERAPEUTIC INDEX = NO ROOM FOR ERROR. Warfarin? One 0.5mg shift = stroke or hemorrhage. Levothyroxine? 5% absorption difference = TSH off the charts. Lamotrigine? Seizure recurrence risk jumps 3x. These aren’t ‘maybe’ cases - they’re red-flag scenarios. If you’re on one of these, your pharmacy is NOT your friend. Track everything. Document everything. And if the pill looks different? CALL YOUR DOCTOR. NOW.
marie HUREL
1 December, 2025 09:03 AMI switched my dad to generic cyclosporine after his transplant. He didn’t say anything for two weeks - then he started forgetting his own birthday. We got his levels checked - trough was 30% below target. We switched back. He’s fine now. I’m just glad we caught it. Maybe it’s rare, but when it happens? It’s life-changing.
Lauren Zableckis
1 December, 2025 20:23 PMI’ve been on generic lamotrigine for five years. No issues. But I know someone who had seizures after a bottle change. So I always check the NDC now. Better safe than sorry.
Asha Jijen
3 December, 2025 13:42 PMgeneric is cheap so why care? i take whatever pharmacy give me. if i feel bad i just drink more chai
Edward Batchelder
3 December, 2025 23:51 PMThis is exactly the kind of information we need more of. So many people assume ‘same active ingredient = same result’ - but our bodies aren’t lab rats. We’re complex, unique, and deserve better than a one-size-fits-all approach. Thank you for writing this. Please keep raising awareness - your voice matters.
reshmi mahi
5 December, 2025 13:17 PMUSA thinks it owns medicine lol. In India we use generics since 1970s and no one dies. You people overthink everything. Just take the pill and stop crying
laura lauraa
6 December, 2025 14:15 PMLet me be clear: the FDA’s ‘AB’ rating is a corporate fiction designed to justify cost-cutting at the expense of vulnerable populations. When a patient reports a change in seizure frequency or INR instability, it’s not anecdotal - it’s systemic failure. And yet, the pharmaceutical-industrial complex continues to weaponize bioequivalence data to silence dissent. This isn’t about ‘individual variation’ - it’s about regulatory capture. And until we hold manufacturers accountable for batch-specific variability, patients will continue to suffer in silence.
Gayle Jenkins
8 December, 2025 09:44 AMMy sister has been on warfarin for 12 years. She switched generics once - her INR went from 2.4 to 4.8 in 72 hours. She almost bled out. Now she refuses to take anything but the same NDC. I’m so glad she kept a log. If you’re on a high-risk med, don’t wait for a crisis - be proactive. Track. Test. Advocate. You’re your own best health guardian.
Kaleigh Scroger
9 December, 2025 18:45 PMFor those asking why this matters - here’s the clinical reality: bioequivalence is defined as 80-125% AUC and Cmax range. That’s a 45% window. For a drug like levothyroxine where the therapeutic window is 10-15 mIU/L, a 10% shift in absorption can push you from euthyroid to subclinical hypothyroidism. That’s not ‘maybe’ - that’s a documented endocrine disruption. And yes, it happens. I’ve seen it. I’ve documented it. And I’ve had patients cry because their doctor told them it was ‘all in their head.’ It’s not. It’s pharmacokinetics. And we need to treat it like the medical issue it is.