Picture someone whose sharp mind once rattled off trivia answers or remembered friends’ birthdays with ease—suddenly, those brainy skills start to slip. For many living with manic-depressive disorder, also known as bipolar disorder, this isn’t just frustrating—it’s bewildering. At one point you’re flying high, juggling tasks, ideas, and conversations. Then, almost overnight, you forget why you walked into a room or lose your grip on words mid-conversation. This isn’t laziness, drama, or lack of intelligence. Science shows bipolar disorder twists the brain’s memory and cognitive gears, flipping the switch depending on whether you’re up in a manic state or stuck in a depressive valley. So, why does this happen, and what can you do about it?
What Manic-Depressive Disorder Does to the Brain
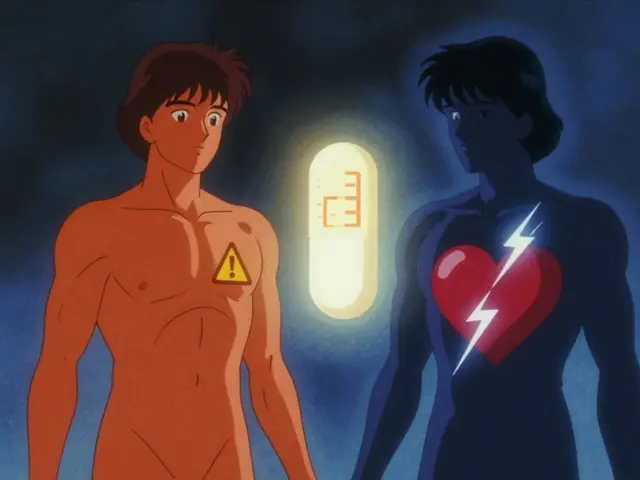
Cut through the stereotypes, and you’ll see that bipolar disorder is tangled deep into how the brain operates. Everything starts with two main periods: mania (or hypomania) and depression. Think of mania as mind on overdrive, ideas buzzing, words tumbling out, energy burning hot. Depression is the opposite, when motivation, energy, and concentration seem to vanish. But here’s the kicker: these ups and downs aren’t just mood swings—they yank around chemicals like dopamine, serotonin, and norepinephrine. Neuroimaging studies show literal shifts. The prefrontal cortex—the part right behind your forehead that runs memory, attention, and decision-making—actually “dims” its activity during depressive episodes. During mania, the brain’s default mode network (the circuit doing mental background checks) runs hot, but not necessarily in a good way. Thoughts race, distractions multiply, and your brain’s “working memory,” or mental scratchpad, easily gets overloaded.
Spotting patterns, the Journal of Affective Disorders reported in 2022 that folks with bipolar disorder have lower scores in cognitive tests during both depressive and manic phases as compared to stable periods. Tasks that involve remembering lists, learning new words, or solving simple puzzles suddenly seem like mountain climbs. But why do these shifts matter? Because they often show up as real-world messes: forgotten appointments, lost items, unfinished projects, or even missing key details in conversations—sometimes adding a layer of guilt or shame.
What about in-between episodes, when moods are “normal”? Studies using MRI scans have found that some people still struggle with memory, attention, and problem-solving even when their mood is stable, a phenomenon called “euthymic cognitive impairment.” And if you think that’s only for people with long-standing illness, research debunks that. Even those newly diagnosed can see these changes. Genetics play a role; it’s estimated that if you have a first-degree relative (like a parent or sibling) with the disorder, your risk jumps as high as 10%. Environmental factors crank up the risk, with childhood trauma, high-stress lives, or major illnesses also chipping away at brain resilience. Real talk: The impact on memory and thinking is baked into the disorder’s roots, not just a side problem.
Memory Loss: It’s More Than Just Forgetfulness
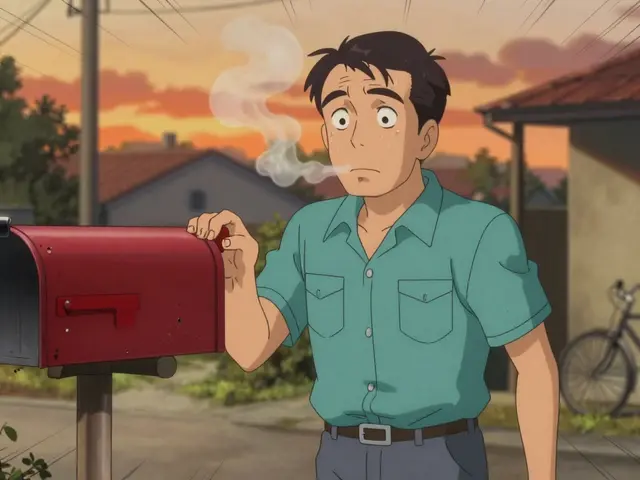
When I talk about “memory loss” in manic-depressive disorder, I don’t just mean classic “I can’t find my keys” moments—although, let’s be honest, those are annoyingly common. The reality goes deeper. Short-term memory, long-term memory, even how you store and pull up facts can all get foggy. During manic states, someone might feel superhuman—thoughts firing left and right, confidence through the roof. But this hype can backfire. Racing thoughts and insomnia mean the brain never really “files away” daily details properly. Imagine reading a book at double speed without turning the page: you catch flashes but miss every plot twist.
The opposite mood, depression, slows everything down. Sitting in a fog, you might forget entire conversations, birthdays, or tasks you’d swear you handled. Research from King’s College London found, in a study of 248 people, that over 60% reported forgetting appointments and plans when depressed. Some couldn’t remember the last movie they’d seen, let alone plot details. And it isn’t always temporary. Sometimes, after years of cycling between highs and lows, the brain “wears grooves,” making some holes in memory permanent or tougher to patch up. MRI scans have found that people living with bipolar disorder sometimes show smaller hippocampi—the brain’s main memory hub—than folks without it.
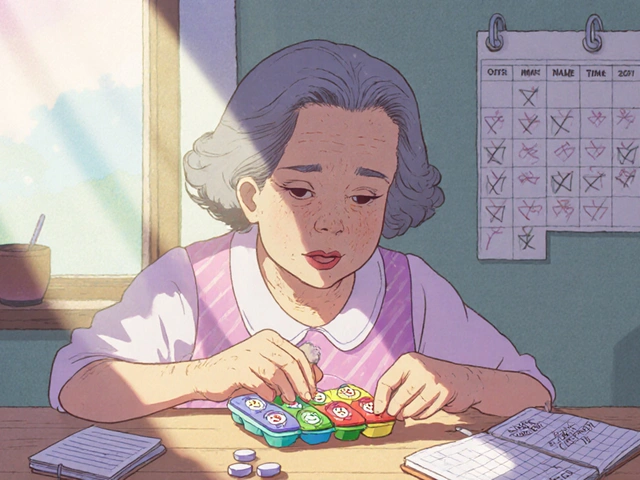
Of course, medication can muddy the picture. Mood stabilizers and antipsychotics, essential for many, sometimes have “memory issues” as rare but real side effects. Forgetting words, losing your train of thought, and feeling slower mentally—these struggles aren’t lacking willpower. They’re a genuine blend of biology, chemistry, and circumstance. Maybe you’ve met someone who seems to blank on shared stories or misplaces important paperwork again and again. If they have bipolar disorder, it’s not sloppiness—it’s the illness scrambling time and details inside their head.

Challenges in Cognitive Function: Focus, Decision, and Processing Speed
It’s easy to chalk up the day-to-day “scatterbrain” moments to distraction or stress, but for many people with manic-depressive disorder, the issue goes way further. One of the biggest complaints? Sustaining attention. You might sit down to work, determined to finish a report or read for pleasure, and suddenly realize half an hour has passed and you’re four sentences in. Even watching a TV show can become a chore—rewinding scenes, re-reading subtitles—because your mind jumps elsewhere. During mania, this gets extreme: grand plans pop up, conversations leap around, and focus is gone. When depression sets in, the world can feel muted; the smallest decision, like what to eat for lunch, drags on and drains mental batteries. Researchers at Stanford found that the average person with bipolar disorder shows a 25% longer time on complex cognitive tasks compared to control groups.
Working memory—the mental scratchpad that holds phone numbers, directions, or multiple tasks in mind—takes a hit regardless of mood. In a 2023 psychological sciences study, participants with bipolar disorder made three times more errors on basic memory games than people without it. Even if you’re sharp in other ways, these little slips can add up throughout the day. Processing speed, another core challenge, slows down in both mania and depression. It’s not just about being “slow”—it’s an actual reduction in how fast the brain sorts and reacts to new info. Imagine driving through dense fog: you see what’s right in front, but miss what's around the bend.
Decision-making also gets tricky. Hyperactivity in manic phases leads to snap decisions, spending sprees, risky behaviors, or sending impulsive texts. Down in depression, the simplest choices bog down amid a swamp of doubt. Cognitive fog can cause major life problems: job slips, relationship clashes, and self-confidence nosedives. My friend once missed her own birthday dinner because she simply lost track of the date—not a crisis, but proof that daily living gets tangled up fast. Teachers, employers, friends, and even partners might not see these invisible battles.
Want a simple test? Ask someone to count backwards from 100 by sevens or recall a list of five objects after five minutes. For someone with bipolar disorder, these tasks can occasionally feel like scaling a mountain—sometimes fine, sometimes frustratingly impossible. Modern therapies now use “cognitive remediation” exercises—brain games, memory strategies, and lifestyle hacks—to help reclaim some of this lost ground. If you notice consistent forgetfulness or trouble focusing, tracking episodes in a journal can reveal patterns and help structure daily life around your brain’s strongest moments.
The Road Ahead: Practical Tips for Sharpening Memory and Cognition
Tackling memory and thinking issues in manic-depressive disorder isn’t about “trying harder”—it’s about working smarter, respecting your brain’s rhythms, and knowing which tools actually help. First, get real about your patterns. Many folks use mood and memory tracking apps. Simple entries—like, “trouble focusing today” or “forgot morning meds”—can pinpoint what’s happening and steer you away from blame spirals. Sharing these logs with your doctor makes meds and therapy way more effective.
Sleep matters—a lot. Up to 90% of people with bipolar disorder struggle with sleep, and missed sleep boosts the odds of memory slip-ups. Set a bedtime routine: keep it boring, turn down lights, and swap out screens. Even my wife Lina, who doesn’t have bipolar disorder, found winding down with a favorite song and cup of herbal tea adds stability.
Break big tasks into smaller bites. Grab a sticky note or phone reminder for even the smallest chore. When my friend Mark started using voice memos for everything from grocery lists to work deadlines, his daily stress dropped. Calendars—digital or paper—protect against missed appointments.
Don’t skip exercise, even walks. Physical movement increases blood flow to the brain, pumping up new neurons and clearing out brain fog. Science backs this: a UCLA study found moderate exercise three times a week improved memory in people with mood disorders by 17%. And hydration—yes, drinking enough water—directly boosts cognitive speed. Even mild dehydration can slow thinking and worsen confusion, so keep a water bottle on hand.
When concentration or memory blanks hit, don’t fight them; instead, give yourself a five-minute reset. Mindfulness—like focusing on your breath or listening to music—helps your brain reset without guilt. Try “chunking” info: Instead of holding a 10-digit phone number, break it into three small groups. Mnemonics, visual cues, and association tricks can all give you more recall power, even on tough days.
If medication seems to fog your mind, bring it up with your psychiatrist. There are alternatives and dose adjustments, and doctors can balance your mental stability with sharp thinking. And connect with others. Peer support groups are treasure troves of real-life memory hacks and offer proof that you’re not alone fighting the invisible cognitive battles.
Finally, don’t underestimate the simple tools: sticky notes, alarms, voice assistants, and checklists—these aren’t crutches, they’re cognitive lifelines. With the right mix of lifestyle tweaks, practical tricks, and medical support, the synapses can regain some spring. And hey, give yourself the grace to laugh at the occasional mental hiccup. Labels like “scatterbrained” or “flighty” miss the mark—what’s happening is as real and scientific as a broken bone, even if you can’t see it. If you spot memory and cognitive shifts affecting someone with manic-depressive disorder, patience and understanding are the best support you can offer. So, go gentle on your mind, lean on good science, and keep experimenting—your best brain days aren’t behind you.




ka modesto
14 June, 2025 10:26 AMLove this breakdown. I’ve seen this in my sister-she’ll be on fire with ideas during hypomania, then forget her own phone number during a depressive episode. It’s not laziness. It’s neurobiology. The part about the hippocampus shrinking over time? Scary but real. I started using Google Keep for everything after reading this. Life changed.
Also, the sleep advice? 100%. Her worst memory lapses always follow all-nighters. Now we treat sleep like oxygen.
Holly Lowe
15 June, 2025 01:54 AMOMG YES. I used to think I was just ‘spacey’ until my psychiatrist slapped me with a cognitive assessment and said, ‘Your brain’s doing the cha-cha between lava and ice.’ 🥶🔥
Now I have a ‘brain fog survival kit’: sticky notes on my mirror, voice memos for grocery lists, and a playlist called ‘Neuro-Nirvana’ that resets me when I’m lost. Also-hydration. I drink a liter before 10am now. My brain thanks me.
PS: If you’re medicated and feeling like your thoughts are wrapped in bubble wrap? Talk to your doc. There’s a sweet spot.
Tressie Mitchell
16 June, 2025 21:10 PMThis is a well-researched article, but let’s be honest-bipolar disorder is overmedicalized. People used to just live with mood swings. Now we’re turning normal human variability into a clinical diagnosis with MRI scans and cognitive remediation. Who benefits? Pharma, mostly.
And calling forgetfulness a ‘symptom’? That’s just pathologizing forgetfulness. I forget where I put my keys too. Does that mean I have a disorder? No. It means I’m human.
Cindy Burgess
17 June, 2025 13:02 PMWhile the scientific content is technically accurate, the tone of this piece is dangerously sentimental. The use of phrases like ‘your best brain days aren’t behind you’ is emotionally manipulative and lacks clinical rigor. There is no ‘reclaiming’ cognition in bipolar disorder-only management. The author’s anecdotal framing risks minimizing the chronic, degenerative nature of the illness.
Furthermore, the recommendation to use voice memos as a ‘cognitive lifeline’ is patronizing. If one’s executive function is impaired, why assume they can consistently operate a smartphone interface?
dayana rincon
18 June, 2025 14:55 PMme: *forgets my own name*
my brain: *still remembers the lyrics to every 2007 pop song* 🤡
also i wrote ‘buy milk’ on my hand and then washed it off. thanks, bipolar. 🙃
Samantha Stonebraker
20 June, 2025 06:09 AMWhat struck me most is how the article frames cognitive impairment not as a failure, but as a rhythm-a biological tide. That’s revolutionary.
I used to beat myself up for missing deadlines. Now I track my energy like weather patterns. Some days, my brain is a sunny meadow. Others, it’s a foggy forest. I don’t fight the fog. I carry a lantern.
And yes-hydration. I used to think it was a myth. Then I drank a liter of water after a depressive episode and actually remembered my mom’s birthday. She cried. I cried. We ate ice cream.
There’s dignity in adaptation. Not perfection. Just presence.
raja gopal
21 June, 2025 20:05 PMAs someone from India who’s seen both traditional healing and modern psychiatry, I can say this: the West over-medicalizes, but also over-helps. In my village, people just say, ‘He’s having a storm inside.’ They don’t call it bipolar. They bring him tea, sit with him, don’t push.
But I also know the meds saved my cousin’s life. So maybe the truth is both: science gives us tools, but compassion gives us space to use them.
Also-walking barefoot on grass helps. My grandmother swore by it. Science now says grounding reduces cortisol. She was right.
Crystal Markowski
23 June, 2025 19:47 PMThank you for writing this with such clarity and compassion. I work as a therapist specializing in mood disorders, and I see daily how cognitive fog isolates people-even from those who love them.
One of my clients started using color-coded calendars: red for depressive days, green for stable, yellow for hypomanic. She began labeling her memory lapses as ‘brain weather,’ not failures. That small shift reduced her shame by 80%.
Also-please, if you’re on lithium: get your thyroid checked. Hypothyroidism mimics brain fog, and it’s easily corrected. Don’t assume it’s the bipolar. Rule out the treatable first.
Charity Peters
24 June, 2025 02:57 AMmy brain is like a browser with 50 tabs open and half of them are frozen. sometimes i just close it all and nap.
also i forgot my dog’s name for three days. he didn’t care. he still licked my face.
Sondra Johnson
25 June, 2025 23:27 PMY’all are missing the point. This isn’t just about memory. It’s about the invisible labor of surviving your own mind.
I used to hide my sticky notes. Now I post them on my fridge like art. ‘DID I PAY THE ELECTRIC BILL?’ ‘DON’T TEXT EX.’ ‘YOU ARE NOT A FAILURE FOR FORGETTING.’
My therapist says, ‘Your brain is not broken-it’s been through a war.’ And you know what? I’m still standing. And I’m still here. And I’m still trying.
That’s not weakness. That’s courage with a foggy lens.
Chelsey Gonzales
27 June, 2025 14:57 PMok but like… i just wrote ‘buy eggs’ on my hand and then i forgot i wrote it and i bought 12 cartons. also i called my boss ‘mom’ by accident. my brain is a glitchy phone.
but i found out that if i hum my fav song while walking, i remember where i’m going. weird? yes. works? yes. 🙌
MaKayla Ryan
28 June, 2025 16:38 PMStop coddling people with mental illness. This isn’t a poetry slam. You’re not ‘courageous’ for forgetting your keys. You’re irresponsible. Get a pill organizer. Set alarms. Stop making excuses. America is falling apart because we treat weakness like wisdom.
My cousin had bipolar. He got a job. He kept it. He didn’t whine about brain fog. He just did it.
Stop making it a trauma story. It’s a choice to be functional.
Kelly Yanke Deltener
29 June, 2025 04:21 AMEvery time I see one of these ‘bipolar is beautiful’ posts, I want to vomit. You think this is a journey? It’s a life sentence. Your brain is a broken machine, and no amount of sticky notes or herbal tea fixes a neurochemical warzone.
And don’t get me started on the ‘you’re not alone’ platitudes. I’m alone. I’m always alone. Because no one gets it. No one can.
So yeah. I forget things. I lose jobs. I lose friends. I lose time. And you? You just scroll past this like it’s a TikTok.
Thanks for the performative empathy. It’s not helping.
Kelly Library Nook
30 June, 2025 21:07 PMWhile the author cites peer-reviewed literature, the article lacks methodological critique. The 2022 Journal of Affective Disorders study referenced had a small sample size (n=124) and failed to control for comorbid anxiety. The MRI data on hippocampal volume reduction is correlational, not causal. Furthermore, the claim that ‘even newly diagnosed individuals show impairment’ is overstated-longitudinal data suggests baseline cognition varies widely.
Additionally, the recommendation to use voice assistants assumes digital literacy and access, which are not universal. The article, while well-intentioned, risks reinforcing ableist assumptions by framing neurodivergence as a problem to be ‘fixed’ with productivity hacks.
Kevin Mustelier
30 June, 2025 21:14 PMAh yes, the classic ‘bipolar brain fog’ narrative. I’ve read this exact piece in three different magazines. It’s the same story, same metaphors, same ‘you’re not lazy, you’re neurodivergent’ mantra.
But here’s the philosophical question: if your memory and cognition are unstable, who is the ‘you’ that’s being described? Are you the manic version? The depressive version? The euthymic one?
Maybe the real problem isn’t the disorder-it’s the illusion of a stable self. We’re all just temporary collections of neurotransmitters. But hey, keep your sticky notes. They’re cute.
Keith Avery
1 July, 2025 05:47 AMActually, this article is dangerously misleading. The hippocampus shrinkage data is from cross-sectional studies, not longitudinal. There’s no proof bipolar causes atrophy-it could be medication, substance use, or even poverty. And the ‘cognitive remediation’ studies? Mostly funded by pharma.
Also, why are we assuming that memory loss is inherently bad? Maybe the brain is pruning what it doesn’t need. Maybe forgetting is a feature, not a bug.
And let’s not forget: the ‘memory loss’ in bipolar is often selective. People remember trauma, insults, and old grudges perfectly. Just not the grocery list. Interesting, isn’t it?
Luke Webster
1 July, 2025 16:12 PMI’m from the U.S., but my father is from Ghana. He used to say, ‘The mind is a drum. Sometimes it beats fast. Sometimes slow. But the rhythm is still there.’
He never called it bipolar. He just made sure I ate well, slept, and didn’t sit alone too long. When I was depressed, he’d sit with me in silence. When I was manic, he’d say, ‘Write it down. I’ll listen later.’
Science is great. But sometimes, the oldest wisdom is the most healing.
And yes-I still use sticky notes. But I also still sit in silence with people who need it. Both matter.
Simran Mishra
2 July, 2025 19:15 PMI’ve lived with this for 17 years. I used to write journals in manic phases-pages and pages of brilliant, chaotic thoughts. Then, in depression, I’d find them and feel like a fraud. Who wrote this? It wasn’t me. It was the storm.
Now I keep digital backups of everything I write. I don’t trust my mind to remember what it created. I’ve lost entire novels, poems, even love letters I wrote to myself.
And the worst part? When I’m stable, I still can’t recall the emotional texture of those manic highs. It’s like I’ve been erased from my own history. I have the words, but not the feeling.
So I don’t chase memory anymore. I chase presence. I hold my dog. I smell coffee. I breathe. And I let the rest drift.
It’s not healing. It’s survival.
And that’s enough.
Faye Woesthuis
3 July, 2025 21:17 PMStop glorifying dysfunction. This isn’t a TED Talk. This is a medical condition with real consequences. People lose jobs, families, homes because of this. No amount of ‘brain fog’ poetry changes that.
If you forget your meds, you’re responsible. If you miss work, you’re responsible. Stop hiding behind neuroscience.
Get. Help. Stay. Stable.
ka modesto
5 July, 2025 00:48 AMThanks for the perspective, @5026. I get where you’re coming from. But here’s the thing: when my sister missed her own daughter’s recital because she forgot the date, it wasn’t laziness. It was her brain’s circuit breaker tripping. We didn’t yell. We got a shared calendar. We set three alarms. We cried together.
Responsibility doesn’t mean punishment. It means support. And sometimes, support looks like sticky notes, not shame.