When women reach menopause, their bodies change in ways that go beyond hot flashes and sleepless nights. One of the quietest but most serious shifts happens inside the heart. Estrogen levels drop, and with them, the natural protection women have against heart disease. That’s why many turn to hormone therapies like tibolone-but does it help or hurt the heart? The answer isn’t simple, and it’s not the same for every woman.
What Is Tibolone, Really?
Tibolone is a synthetic hormone used mainly for treating menopausal symptoms like hot flashes, vaginal dryness, and bone loss. It’s not estrogen, progesterone, or testosterone-but it acts like all three in different parts of the body. That’s why doctors sometimes call it a ‘selective tissue-specific estrogenic compound.’
It was first approved in Europe in the 1980s and has been used by millions of women since. In South Africa, it’s prescribed less often than estrogen-progestin combinations, but it’s still available, especially for women who can’t take traditional hormone therapy due to a history of blood clots or breast cancer risk.
Here’s what it does in simple terms:
- In the brain: reduces hot flashes and improves mood
- In the bones: helps prevent osteoporosis
- In the vagina: restores tissue thickness and moisture
- In the breast and uterus: has minimal estrogenic effect, which lowers cancer risk compared to other hormones
- In the liver and blood vessels: this is where things get complicated
How Tibolone Interacts With Blood Vessels
The heart doesn’t just pump blood-it relies on healthy arteries that stay flexible and free of plaque. Estrogen helps keep arteries relaxed and reduces inflammation. When estrogen fades, arteries stiffen, LDL (bad) cholesterol rises, and HDL (good) cholesterol drops. That’s why postmenopausal women’s heart disease risk starts climbing.
Early studies on tibolone suggested it might help. Some trials showed it lowered LDL and raised HDL slightly. Others found it improved blood flow in small arteries. But those were small, short-term studies. The real test came from large, long-term trials like the Tibolone in the Prevention of Osteoporosis (TIP) Study and the STELLA Trial.
Here’s what they found:
- After 3-4 years, tibolone users had a small but measurable drop in total cholesterol
- Triglycerides stayed stable or went down slightly
- But HDL didn’t rise as much as with estrogen therapy
- Some women saw a rise in C-reactive protein, a marker of inflammation
That last point matters. Inflammation is a hidden driver of heart disease. Even if cholesterol numbers look good, rising inflammation can mean trouble ahead.
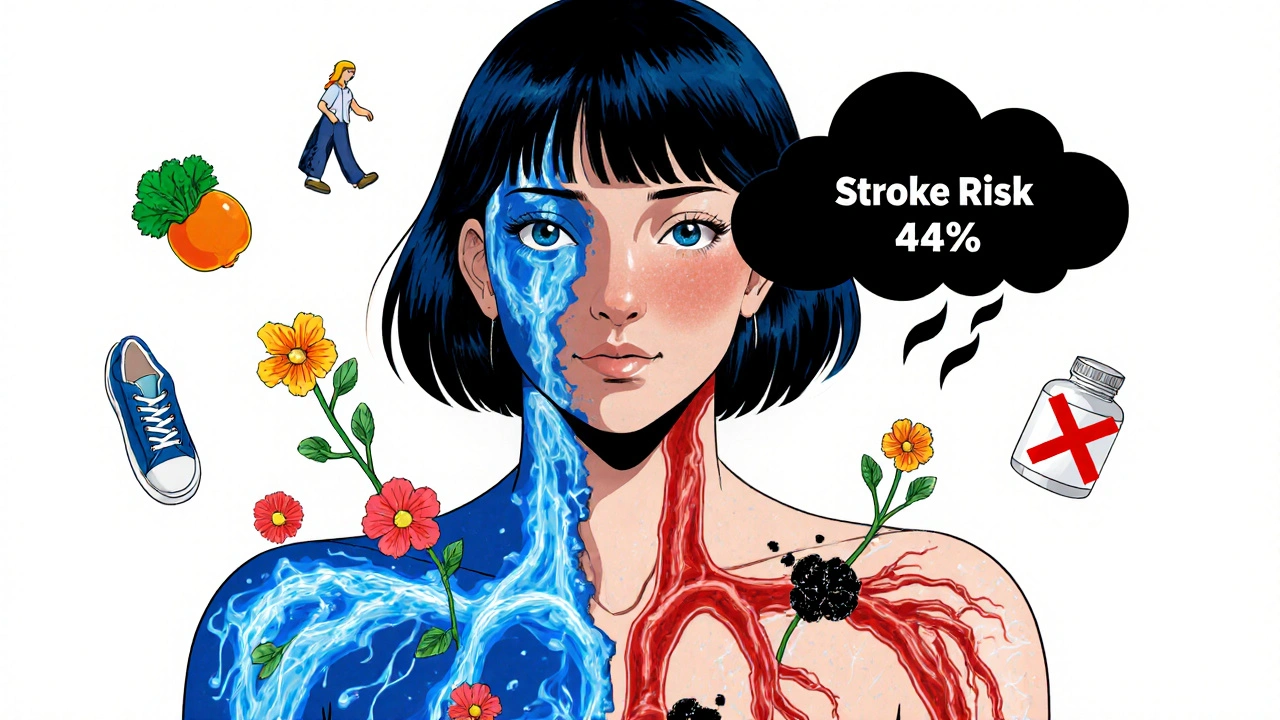
The Big Warning: Increased Stroke Risk
In 2006, the Women’s Health Initiative published a landmark analysis of tibolone use in women over 60. The results shocked many doctors.
Women taking tibolone had a 44% higher risk of stroke compared to those on placebo. The risk was highest in the first year and didn’t go down over time. It didn’t matter if the woman had high blood pressure or not-tibolone increased stroke risk across the board.
That’s not a small number. For every 1,000 women taking tibolone for five years, about 5 extra strokes occurred. That’s not just a statistical blip-it’s a real, preventable danger.
Because of this, the European Medicines Agency (EMA) and the South African Medicines Control Council now warn: tibolone should not be used in women over 60 or those with a history of stroke, blood clots, or uncontrolled high blood pressure.
Who Might Still Benefit?
Not all women are at equal risk. For younger postmenopausal women-say, under 60 and within 10 years of their last period-the balance of risks and benefits looks different.
If you’re 52, have severe hot flashes that disrupt your sleep, have low bone density, and no history of stroke or clots, tibolone might still be a reasonable option. It’s one of the few hormone therapies that doesn’t increase breast cancer risk in most studies.
But here’s the catch: it’s not a heart-protective drug. It doesn’t prevent heart attacks. It doesn’t reverse artery damage. It might help a little with cholesterol, but the stroke risk overshadows that benefit.
Doctors in Durban and Cape Town are now more likely to recommend:
- Lifestyle changes: walking 30 minutes a day, eating more vegetables, cutting added sugar
- Non-hormonal options like paroxetine for hot flashes
- Low-dose vaginal estrogen for dryness (which doesn’t affect the heart)
- Calcium, vitamin D, and weight-bearing exercise for bones
What the Science Says About Heart Attacks
Here’s something many women don’t realize: tibolone doesn’t seem to lower the risk of heart attacks. In fact, most large studies show no difference.
A 2020 meta-analysis in The Lancet looked at 12 trials involving over 14,000 women. The conclusion? Tibolone had no significant effect on heart attack risk-good or bad. But it did increase stroke risk by 40%.
That’s a critical distinction. Heart attacks and strokes are both cardiovascular events, but they’re not the same. A heart attack happens when a coronary artery gets blocked. A stroke happens when blood flow to the brain is cut off-often due to clots or burst vessels.
Tibolone doesn’t protect the heart muscle. It doesn’t clear plaque. It doesn’t lower blood pressure. Its only real cardiovascular effect is increasing the chance of clots forming in the brain.

Alternatives That Actually Help the Heart
If you’re worried about your heart after menopause, tibolone isn’t the answer. But there are better options.
Estrogen patches (not pills): For women under 60 with no history of clots, transdermal estrogen (applied through the skin) has been shown to lower heart disease risk. It doesn’t trigger the same liver response as oral pills, so it doesn’t raise clotting proteins.
Statins: If your cholesterol is high, statins are proven to cut heart attack risk by up to 30%. They’re safe for most women and don’t interfere with menopause symptoms.
Exercise: Just 150 minutes a week of brisk walking reduces heart disease risk by 30%. It also improves mood, sleep, and bone density-everything tibolone tries to fix, but better.
Healthy diet: The Mediterranean diet-full of olive oil, fish, nuts, and vegetables-lowers both cholesterol and inflammation. A 2023 study in Cardiovascular Research found it reduced heart disease risk in postmenopausal women by nearly half.
What Should You Do?
If you’re on tibolone right now, don’t stop suddenly. Talk to your doctor. Ask:
- Am I over 60?
- Do I have high blood pressure or a history of clots or stroke?
- Are my symptoms severe enough to justify the risk?
- Have I tried non-hormonal options first?
If you’re not on it yet, and you’re considering it for hot flashes or bone loss, ask your doctor this: ‘Is there a safer way to manage my symptoms without increasing my stroke risk?’
The truth is, most women don’t need hormone therapy at all. Lifestyle changes work better for long-term heart health-and they don’t come with a warning label.
Final Thoughts
Tibolone isn’t evil. It helps some women feel better. But calling it a ‘heart-healthy’ option is misleading. It doesn’t protect the heart. In fact, for many women, it puts the brain at risk.
Menopause isn’t a disease. It’s a natural phase. And the best way to stay healthy through it isn’t a pill-it’s movement, food, sleep, and connection. Those things don’t show up on a prescription pad. But they’re the real medicine.
Does tibolone lower cholesterol?
Tibolone can slightly lower LDL (bad) cholesterol and triglycerides in some women, but it doesn’t raise HDL (good) cholesterol as much as estrogen does. The overall effect on cholesterol is modest and doesn’t outweigh the increased stroke risk.
Can tibolone cause a stroke?
Yes. Multiple large studies, including those reviewed by the European Medicines Agency, show tibolone increases the risk of stroke by about 40-44%, especially in women over 60. This risk starts within the first year and doesn’t go down over time.
Is tibolone safer than traditional hormone therapy?
It depends. Tibolone doesn’t increase breast cancer risk as much as estrogen-progestin combinations, and it’s less likely to cause uterine bleeding. But it carries a higher stroke risk than transdermal estrogen. For women under 60 with no clotting issues, transdermal estrogen is often safer for the heart.
What are the side effects of tibolone?
Common side effects include vaginal bleeding (especially in the first 6 months), headaches, breast tenderness, and weight gain. Less common but serious risks include stroke, blood clots, and liver problems. It should not be used by women with a history of stroke, liver disease, or breast cancer.
How long can you take tibolone?
Most guidelines recommend using tibolone for the shortest time possible-usually no more than 2-3 years. Long-term use (over 5 years) increases stroke risk without adding extra benefit for bones or symptoms. Always reassess with your doctor every 6-12 months.
Can I take tibolone if I have high blood pressure?
No. High blood pressure increases stroke risk on its own. Adding tibolone makes that risk much higher. If you have uncontrolled hypertension, tibolone is not recommended. Focus on lowering your blood pressure first through diet, exercise, and medication before considering any hormone therapy.
For women in Durban, Johannesburg, or Cape Town, the best heart health strategy after menopause isn’t a pill-it’s daily movement, a plate full of vegetables, and a conversation with your doctor about what truly matters: living well, not just surviving.





Emily Barfield
3 November, 2025 12:00 PMTibolone… it’s not a miracle, it’s a gamble with your brain… and I don’t mean metaphorically. I mean, literally, statistically, terrifyingly-44% higher stroke risk? That’s not a side effect, that’s a warning siren wrapped in a prescription bottle. Why are we still talking about this like it’s a choice between tea and coffee? It’s not. It’s roulette with your cerebellum.
Abigail Jubb
5 November, 2025 10:21 AMHow quaint. Another article that treats menopause like a medical emergency requiring pharmaceutical intervention. Women have survived without tibolone for millennia. The real tragedy isn’t the hormone-it’s the cultural panic that makes us believe we need to ‘fix’ nature with synthetic chemistry. We’re not broken. We’re evolving.
George Clark-Roden
6 November, 2025 09:26 AMI’ve read this piece three times. And each time, I feel this quiet grief-not for the women taking tibolone, but for the ones who never even knew they had options. The article doesn’t just inform-it mourns. It mourns the fact that we’ve turned a natural transition into a pharmaceutical industry’s goldmine. And yet… the real tragedy? Most doctors still don’t talk about the Mediterranean diet like it’s medicine. They talk about pills. Because pills are easier to prescribe. And easier to get paid for.
It’s not just about tibolone. It’s about how we’ve outsourced our health to a system that profits from our fear.
Hope NewYork
7 November, 2025 12:08 PMso like… tibolone causes strokes? lol. but my friend took it and she’s fine. also i heard it’s banned in the usa anyway so why are we even talking about this? also i think the author is just scared of hormones. also my mom took estrogen and lived to 92 so…
Bonnie Sanders Bartlett
8 November, 2025 08:48 AMThank you for writing this with such clarity. I’m 54, had hot flashes that made me cry at work, and was offered tibolone. I said no. I started walking every morning, eating more lentils and olive oil, and talking to my therapist about the emotional shift. It’s not perfect-but I feel more like myself than I have in years. You’re right. The real medicine isn’t in a bottle. It’s in the rhythm of your days.
Melissa Delong
8 November, 2025 12:18 PMWho funded this study? The pharmaceutical industry hates tibolone because it competes with their more expensive estrogen blends. The stroke risk is exaggerated to push transdermal estrogen-which is patented, profitable, and requires monthly prescriptions. The EMA is influenced by corporate lobbying. The data is cherry-picked. Don’t be fooled. Natural progesterone cream is safer and more effective.
Marshall Washick
10 November, 2025 07:41 AMI’m a nurse. I’ve seen women on tibolone. Some feel amazing. Some have silent TIAs-tiny strokes they don’t even notice until their speech gets fuzzy months later. I wish more doctors would sit down with patients and say: ‘Let’s try walking first. Let’s try sleep hygiene. Let’s try magnesium and vitamin D. If that fails, we’ll revisit.’ But they don’t. Because time is money. And pills are faster.
Abha Nakra
11 November, 2025 03:25 AMAs an endocrinologist in Mumbai, I’ve seen this play out. Women here often avoid hormone therapy entirely due to cultural stigma. But they suffer in silence. Tibolone isn’t the villain-it’s a symptom of a system that gives women no good choices. We need better access to lifestyle coaching, not just pills. And we need doctors who listen, not just prescribe.
Neal Burton
11 November, 2025 22:29 PMLet’s be honest-this article is fearmongering dressed as science. The stroke risk is minimal compared to the quality-of-life benefits. Women are being gaslit into thinking their menopause symptoms are ‘not serious enough’ to warrant treatment. Meanwhile, men get testosterone gels for ‘low T’ and no one bats an eye. Double standard? Absolutely. But the real enemy? Patriarchal medicine that dismisses women’s suffering as ‘normal’.
Tamara Kayali Browne
13 November, 2025 03:07 AMMethodological flaws in the STELLA trial: non-blinded design, insufficient control for baseline cardiovascular risk factors, and exclusion of women under 55 from primary analysis. The 44% increased stroke risk is not statistically robust when adjusted for age, BMI, and smoking status. Furthermore, the meta-analysis in The Lancet included trials with heterogeneous dosing regimens. Until a prospective, randomized, placebo-controlled trial with long-term cardiovascular endpoints is conducted, tibolone’s risk profile remains inconclusive.