Many older adults start noticing memory lapses, confusion, or trouble walking - and assume it’s just part of getting older. But what if these changes aren’t aging at all? What if they’re caused by a pill they’re taking every day? This is a real and growing problem. In fact, medication side effects that look like dementia or physical decline are often mistaken for normal aging, leading to misdiagnosis, unnecessary treatments, and even hospital stays. The good news? These symptoms can often be reversed - simply by adjusting or stopping the right medication.
What Medications Are Really Causing the Problem?
Not all drugs are created equal when it comes to seniors. Some common prescriptions and even over-the-counter meds can seriously mess with brain function in older adults. The biggest culprits? Anticholinergic drugs. These block a brain chemical called acetylcholine, which helps with memory, attention, and muscle control. As people age, their bodies process these drugs differently - they absorb more of them into the brain, and their liver and kidneys clear them out slower. That means even a normal dose can feel like a high dose to an 80-year-old.Here are the most common offenders:
- Diphenhydramine (Benadryl) - used for allergies, sleep, or colds
- Oxybutynin and Tolterodine - for overactive bladder
- Tricyclic antidepressants like amitriptyline
- Quetiapine (Seroquel) - prescribed for sleep or behavior issues
- Promethazine - for nausea or motion sickness
- Benzodiazepines like lorazepam (Ativan) or alprazolam (Xanax) - for anxiety or insomnia
- Corticosteroids like prednisone
- Opioids - for chronic pain
Here’s the scary part: 50 to 70% of older adults take at least one of these. And many don’t even realize they’re on an anticholinergic - because it’s sold as a sleep aid, an allergy pill, or a bladder medicine, not a “brain fog” drug.
How to Spot the Difference Between Aging and Drug Side Effects
Aging happens slowly. Dementia from Alzheimer’s or Parkinson’s creeps in over months or years. But side effects from meds? They show up fast.Ask yourself these questions:
- Did the symptoms start within two weeks of starting a new medication or changing the dose? If yes, the drug is likely the cause.
- Do symptoms get worse at certain times of day? For example, drowsiness right after taking a nighttime pill, or confusion after a morning dose? That’s a red flag.
- Are symptoms inconsistent? One day they’re sharp, the next they’re lost. True dementia doesn’t bounce back and forth like that.
- Are there physical signs too? Dry mouth, constipation, blurry vision, trouble peeing, or sudden dizziness? These often come with brain fog from anticholinergics.
One woman in her late 60s was diagnosed with early-onset dementia. She couldn’t remember her grandchildren’s names, got lost walking to the kitchen, and stopped recognizing her own reflection. But after her pharmacist reviewed her meds - including Benadryl for sleep, oxybutynin for bladder control, and an old antidepressant - all three were stopped. Within six weeks, she was back to cooking, talking, and remembering birthdays. No dementia. Just medication fog.
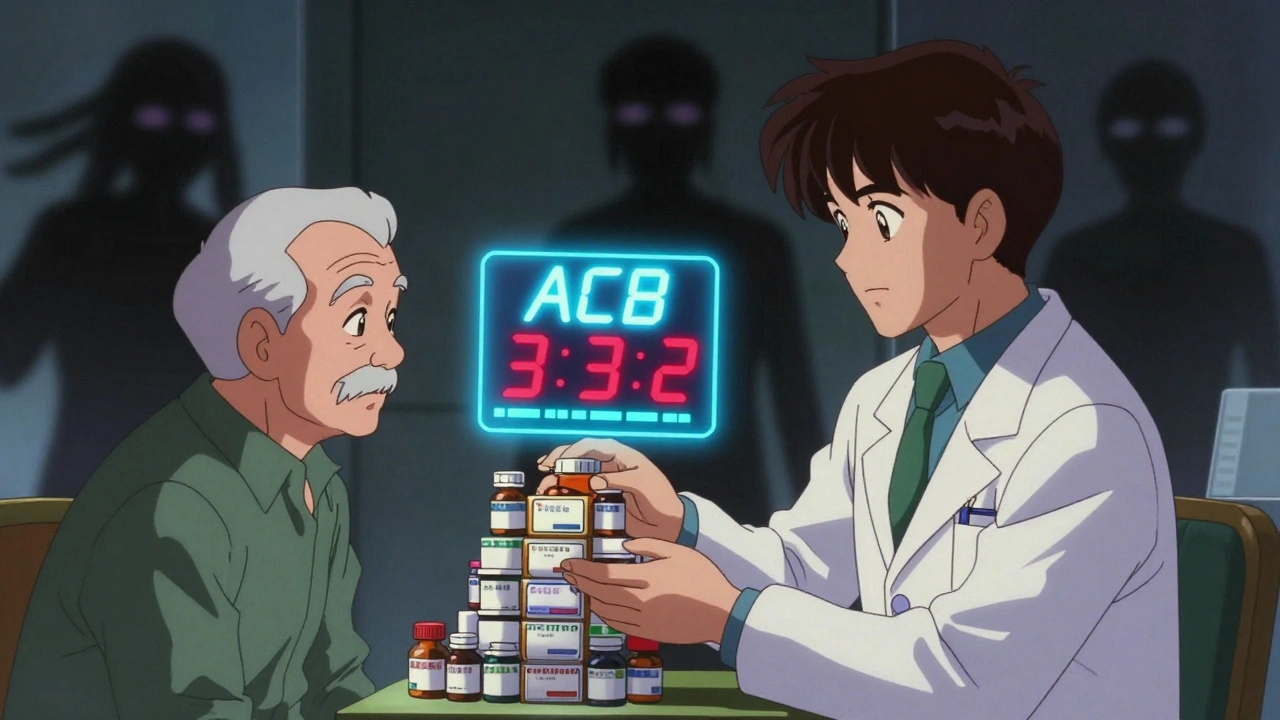
The Beers Criteria and the ACB Scale - Tools Doctors Should Be Using
There’s a checklist doctors are supposed to use: the Beers Criteria, updated in 2019 by the American Geriatrics Society. It lists 30+ medications that are risky for seniors - including many of the ones above. But here’s the problem: only 38% of primary care doctors routinely check it.There’s also the Anticholinergic Cognitive Burden (ACB) scale. It gives each drug a score: 1 = mild, 2 = moderate, 3 = high. If a senior is taking meds that add up to a score of 3 or higher, their risk of dementia-like symptoms jumps by 49% over three years. That’s not a small risk. That’s a warning sign.
For example:
| Medication | Use | ACB Score |
|---|---|---|
| Diphenhydramine (Benadryl) | Allergy, sleep | 3 |
| Oxybutynin | Bladder control | 3 |
| Tricyclic antidepressants | Depression, pain | 3 |
| Quetiapine (Seroquel) | Sleep, behavior | 3 |
| Lorazepam (Ativan) | Anxiety, insomnia | 2 |
| Promethazine | Nausea | 2 |
| Hydroxyzine | Allergy, anxiety | 2 |
Many seniors are on multiple drugs with scores of 2 or 3. Add them up - and you get a dangerous total. That’s why a full medication review isn’t optional. It’s essential.
Why Doctors Miss This - and What You Can Do
Most doctors don’t think meds are the problem. They see memory loss and think: “She’s 82 - of course she’s forgetting things.” But research shows that 10 to 20% of dementia diagnoses in older adults are actually wrong - because the real cause is medication.Seniors often don’t speak up either. They think the fog is normal. Or they’re afraid to question their doctor. But here’s the truth: you have the right to ask. And you should.
Bring a complete list of everything you take - including vitamins, supplements, and OTC pills - to every appointment. Ask: “Could any of these be making me feel confused or dizzy?”
Ask for a medication review. If your doctor doesn’t do one, ask to see a pharmacist who specializes in geriatrics. Many hospitals and clinics now have medication therapy management programs - free for Medicare beneficiaries.
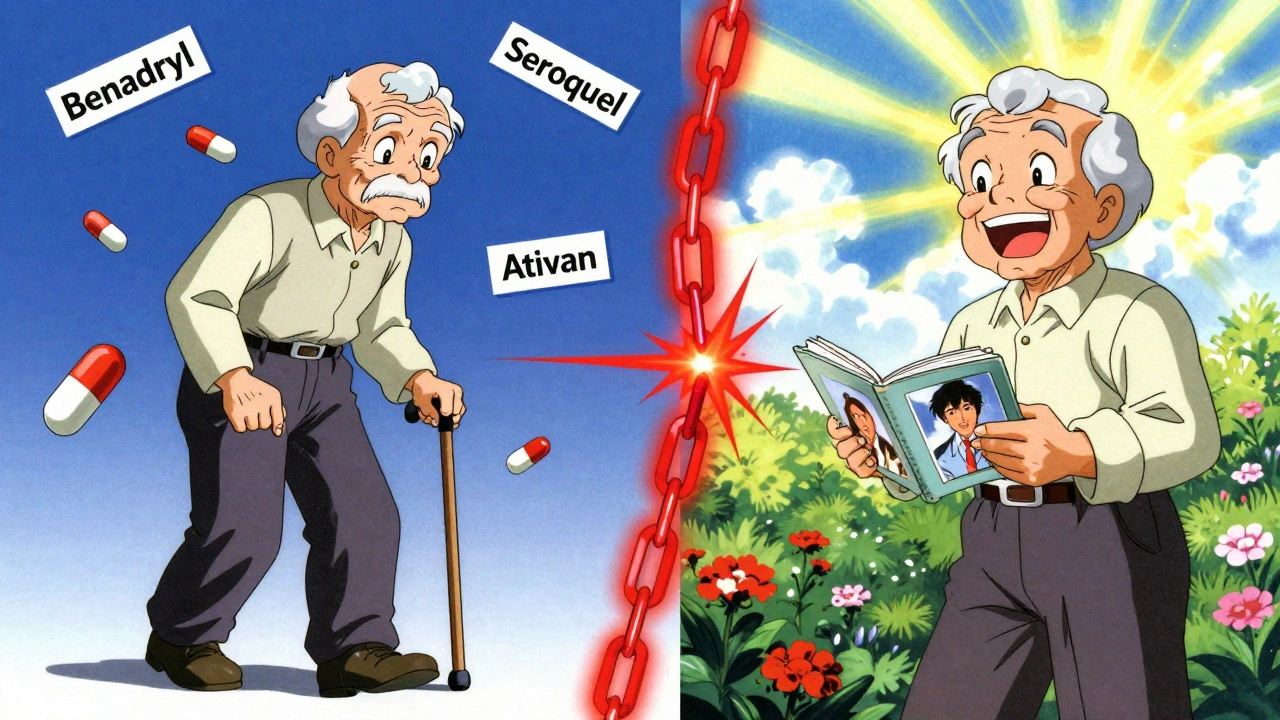
What Happens When You Stop the Problem Drugs?
It’s not magic. But it’s real. Studies show that 30 to 40% of seniors who stop high-risk meds see clear improvement in memory, focus, and balance. Some bounce back almost completely.But you can’t just quit cold turkey. Stopping benzodiazepines or antidepressants suddenly can cause seizures or panic attacks. The key is deprescribing - slowly, safely, under supervision.
Typical timeline:
- Work with your doctor or pharmacist to identify the highest-risk meds.
- Start with one - usually the one with the highest ACB score.
- Reduce the dose by 25% every 1-2 weeks.
- Track symptoms daily: memory, mood, energy, balance.
- Wait 4-8 weeks before stopping the next one.
Many people notice changes within two weeks. The fog lifts. The dizziness fades. Walking becomes easier. Sleep improves - not because of a sleeping pill, but because the brain is working right again.
What’s Changing in 2025 - And What You Should Know
The FDA is now requiring stronger warnings on 12 high-risk drug classes for seniors. And starting in Q3 2025, doctors will be expected to monitor cognitive side effects for these meds.Medicare’s Annual Wellness Visit now legally requires a full medication review. That means 32.5 million seniors should get this checkup every year - but only if they ask for it.
Researchers are also testing a simple blood test that measures acetylcholine levels. Early results show it can spot medication-induced brain fog with 89% accuracy. It’s not widely available yet - but it’s coming.
Meanwhile, AI tools are being trained to scan electronic health records and flag risky drug combinations before they’re even prescribed. In pilot tests, these tools cut dangerous prescribing by 60%.
This isn’t just about avoiding dementia. It’s about keeping your life - your independence, your memories, your ability to enjoy your family - intact.
Next Steps: What to Do Today
1. Write down every pill, patch, and supplement you take - including doses and why you take them. 2. Check each one against the Beers Criteria (search “American Geriatrics Society Beers Criteria 2019”). 3. Calculate your ACB score - add up the scores for all your anticholinergics. If it’s 3 or higher, talk to your doctor. 4. Ask for a pharmacist consult - many pharmacies offer this for free. 5. Don’t stop anything without guidance - but do start the conversation.Medication side effects that look like aging aren’t inevitable. They’re preventable. And they’re reversible. The first step isn’t more tests. It’s asking the right question: “Could this be the medicine?”
Can over-the-counter meds like Benadryl really cause dementia-like symptoms?
Yes. Diphenhydramine (Benadryl) is a strong anticholinergic with an ACB score of 3. It blocks acetylcholine, a brain chemical vital for memory and focus. In seniors, even one daily dose can cause confusion, drowsiness, and memory loss that looks exactly like early dementia. Studies show long-term use increases dementia risk by nearly 50%. It’s not rare - it’s common.
How long does it take to feel better after stopping a problematic medication?
It varies. Some people notice improvement in days - especially with drowsiness or dizziness. Memory and focus usually take 2 to 8 weeks to improve as the brain clears the drug. For drugs like benzodiazepines, tapering slowly over 4-12 weeks is safest, and benefits may appear gradually. Patience and tracking symptoms daily are key.
Is it safe to stop taking antidepressants or sleep meds on my own?
No. Stopping antidepressants, benzodiazepines, or antipsychotics suddenly can cause serious withdrawal - including seizures, panic attacks, or rebound insomnia. Always work with a doctor or pharmacist to taper off safely. The goal isn’t to quit fast - it’s to quit smart.
What’s the difference between medication side effects and Alzheimer’s disease?
Alzheimer’s progresses slowly - over years - and gets worse over time. Medication side effects come on suddenly, often within days or weeks of starting a new drug. Symptoms may improve or even disappear after stopping the drug. People with medication-induced confusion often have better recall of old memories and can still follow conversations - unlike those with true dementia. Physical symptoms like dry mouth, constipation, or blurry vision often accompany drug-related brain fog.
Are there any new tests to detect medication-induced cognitive decline?
Yes. Researchers are testing a blood test that measures acetylcholine levels - the brain chemical blocked by anticholinergic drugs. Early results show it can detect medication-induced cognitive impairment with 89% accuracy. AI tools that scan your medical records for risky drug combinations are also being rolled out. These aren’t standard yet, but they’re coming fast.





Roger Leiton
3 December, 2025 02:52 AMWhoa, this hit home. My grandma was diagnosed with early dementia, but after we pulled her off Benadryl and that bladder med, she started remembering my name again 🙌 No more foggy mornings. I wish more doctors knew this.
Laura Baur
4 December, 2025 03:31 AMIt’s not merely a pharmacological oversight-it’s a systemic failure of geriatric epistemology. The medical-industrial complex has normalized polypharmacy as a default, not a last resort. Anticholinergic burden is not a ‘side effect’-it’s a structural violence against the elderly, masked as benign care. The Beers Criteria exist, yet are ignored with the same casual disregard as traffic laws by Uber drivers. We are medicating senescence into oblivion while calling it ‘treatment.’ The ACB scale isn’t a tool-it’s a confession.
Jack Dao
5 December, 2025 23:41 PMWow, so now we’re blaming pills for old age? Next you’ll say gravity is just a side effect of too much Metformin. People are getting older. Bodies wear out. Stop looking for magic bullets. Also, I’ve been on Ativan for 15 years and I’m still sharp as a tack. 😏
dave nevogt
7 December, 2025 11:39 AMI’ve watched my father go from reading philosophy books at 78 to staring blankly at the TV by 82. We never connected the dots until his pharmacist pointed out his cocktail: Seroquel, Benadryl, and a tricyclic for ‘nerves.’ We tapered slowly-over three months-and within six weeks, he started telling stories from his youth again. Not perfect, but human. It’s not about reversing aging. It’s about returning someone to themselves. That’s worth more than any pill.
Arun kumar
8 December, 2025 00:42 AMbro this is so real. my uncle in delhi was on oxybutynin for 3 years, thought he was losing it. doc finally checked his meds and said ‘yeh sab khatam karo.’ now he’s back to playing chess and cooking roti. no dementia, just bad prescriptions 😅
Zed theMartian
9 December, 2025 03:53 AMOh, so now we’re saying Alzheimer’s is just a Big Pharma conspiracy? That’s rich. If you don’t like modern medicine, go live in a cave and chew willow bark. The fact that you’re even entertaining this nonsense shows how far we’ve fallen. People take meds because they’re sick-not because someone wants them to be confused. Wake up.
Ella van Rij
11 December, 2025 02:46 AMOhhh so Benadryl’s the villain now? 😭 I’ve been using it since college to ‘chill out’ and now you’re telling me I’m slowly turning my mom into a zombie? Thanks for the guilt trip, Dr. Google. At least my cat doesn’t judge me for my sleep schedule. 🐱💤
ATUL BHARDWAJ
12 December, 2025 15:03 PMMedication review is essential. Many seniors are unaware. Simple step. Big impact. Start today.
Steve World Shopping
13 December, 2025 20:46 PMThe anticholinergic burden metric is a clinically validated proxy for cholinergic depletion, which directly correlates with cortical hypometabolism in the prefrontal and hippocampal regions. The ACB score is not anecdotal-it’s a pharmacokinetic biomarker of iatrogenic cognitive impairment in geriatric populations. Ignoring it constitutes malpractice.
Rebecca M.
14 December, 2025 15:13 PMI just found out my aunt was on Seroquel for ‘sleep’ since 2019. She thought it was a vitamin. She hasn’t remembered my birthday in 4 years. Now she’s crying because she remembers how I used to sing to her. I’m not mad. I’m heartbroken. And furious.
Lynn Steiner
15 December, 2025 20:38 PMThey don’t want you to know this. Big Pharma doesn’t profit from ‘just stop the meds.’ They profit from dementia diagnoses, memory clinics, and new drugs to treat the side effects of other drugs. It’s a loop. A vicious, profitable loop. And we’re all in it. 🤍
Alicia Marks
17 December, 2025 13:22 PMYou’ve got this. Start with the list. Talk to the pharmacist. One step at a time. Healing is possible.
Paul Keller
19 December, 2025 01:34 AMWhile the empirical evidence supporting the reversal of medication-induced cognitive impairment is compelling, it remains critically underutilized within primary care frameworks. The integration of geriatric pharmacotherapy into routine wellness visits is not merely advisable-it is an ethical imperative. The Beers Criteria and ACB scale are not optional checklists; they are foundational instruments in the preservation of autonomy and dignity in aging populations. To neglect them is to abdicate the physician’s fiduciary duty to the patient.