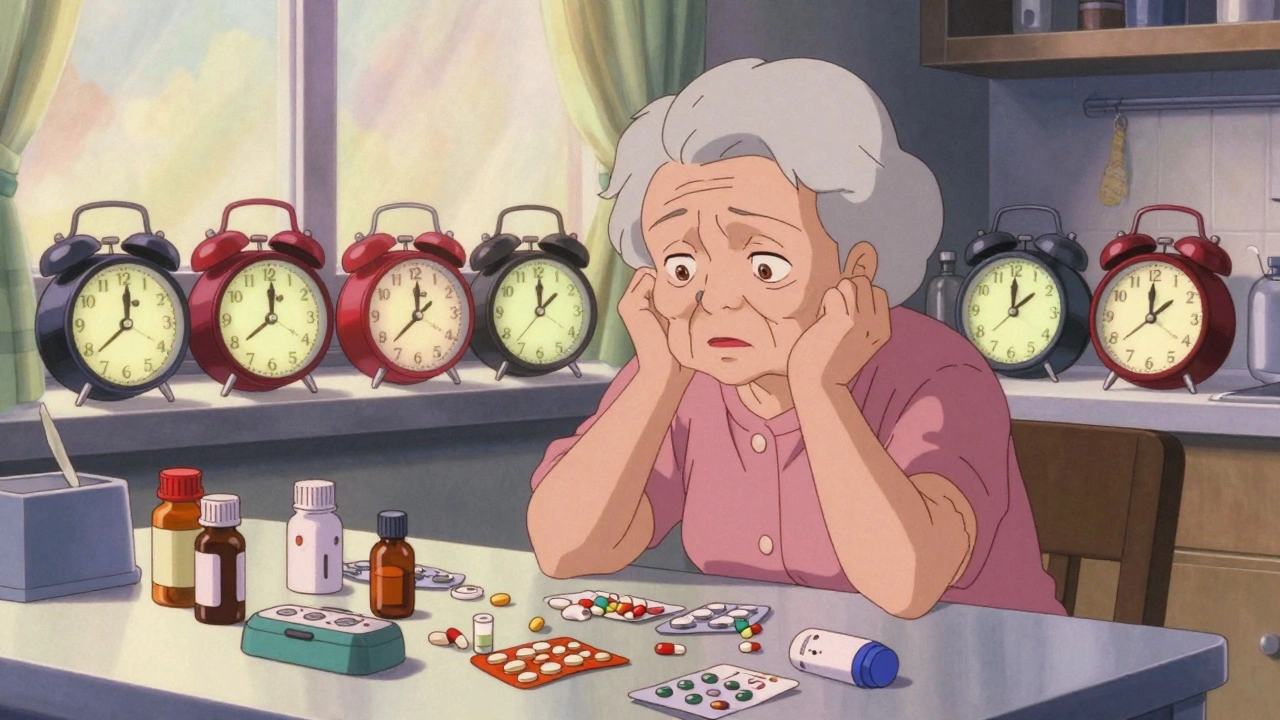
For many older adults, taking medications becomes a daily struggle-not because they forget, but because the regimen is simply too complicated. Imagine waking up at 6 a.m. for a pill, then again at 8 a.m., noon, 3 p.m., 6 p.m., and bedtime. That’s six different times, maybe eight different pills, some with food, some without, some to be swallowed upright, others to be held under the tongue. And if you’re managing diabetes, high blood pressure, arthritis, and heart failure? That’s not just a routine-it’s a full-time job. And it’s one that many seniors can no longer keep up with.
Why Medication Regimens Get So Complicated
It’s not that doctors are being careless. Often, each medication was prescribed for a specific reason, by a different specialist, at a different time. A cardiologist adds a blood thinner. A rheumatologist prescribes a painkiller. A neurologist adds a sleep aid. A primary care doctor throws in a vitamin. No one sits down and asks: How many times a day is this person supposed to take pills? By the time all the prescriptions stack up, an older adult might be handling 10 or more doses daily. Studies show that nearly 40% of adults over 65 in the U.S. take five or more medications regularly. In aged care facilities, it’s often double that.This isn’t just about confusion. It’s about safety. Missed doses, double doses, wrong timing-all lead to hospital visits. A 2020 study found that 83% of simplification efforts improved medication adherence. But here’s the catch: better adherence doesn’t always mean better health. Taking the right pills at the wrong time can still cause harm. That’s why simplification isn’t just about reducing pills-it’s about smart, safe reorganization.
The Three Ways to Simplify Medication Regimens
There are three proven strategies used by pharmacists and geriatric specialists to cut through the clutter:- Fixed-dose combinations: Instead of taking two separate pills-one for blood pressure, one for cholesterol-switch to a single pill that contains both. This cuts pill count in half and removes the need to remember two different times.
- Once-daily dosing: Many medications now come in long-acting forms. A blood pressure pill that used to need two doses a day can often be replaced with one that lasts 24 hours. Same goes for some antidepressants, diabetes meds, and even certain antibiotics.
- Combination approach: The most effective method. Reduce both the number of pills and the number of times they’re taken. For example, switching from three daily pills to one once-daily combination tablet.
These aren’t theoretical. A 2020 trial in U.S. community-dwelling seniors found that 41% of medication regimens could be simplified just by adjusting dosing times and switching to once-daily versions. In Australian aged care homes, pharmacists were able to simplify regimens for 58% to 60% of residents using a structured tool called MRS GRACE.
When Simplification Works Best
Not all medications respond the same way. Some classes benefit more than others:- Antiretrovirals (for HIV): Combined simplification (fewer pills + once-daily) boosted adherence by over 70%.
- Insulin: Switching from multiple daily injections to once-daily long-acting insulin improved consistency and reduced errors.
- Antipsychotics: Long-acting injectables or once-daily oral versions cut down on missed doses and improved behavior management in dementia patients.
- Diabetes and hypertension: Surprisingly, simplification didn’t always improve adherence here. Why? Because timing matters. Some blood pressure meds work best at night. Some diabetes drugs need to be taken right before meals. Changing that can backfire.
That’s the tricky part. You can’t just shuffle pills around like a deck of cards. A statin must be taken at night to block cholesterol production. Levothyroxine must be taken on an empty stomach, 30 minutes before breakfast. These aren’t suggestions-they’re biological rules. Simplification must respect them.
The Five-Step Simplification Process
Real simplification isn’t a quick fix. It’s a careful process. Here’s what it looks like in practice:- Get the full picture. Start with a best possible medication history. That means collecting every pill, supplement, and over-the-counter drug the person is taking-even the ones they forget about. Studies show that between 5 and 10 errors exist in every senior’s medication list when compared to what’s actually being taken.
- Check if each drug is still needed. This is called deprescribing. Maybe that sleeping pill was prescribed five years ago and hasn’t been reviewed since. Maybe the painkiller is doing more harm than good. Not every pill is worth keeping.
- Identify simplification opportunities. Look for pills that can be switched to once-daily versions. Look for combinations. Look for drugs that can be taken at the same time as another.
- Match timing to daily life. Can a pill be taken with breakfast instead of 7 a.m. alone? Can a nighttime dose be moved to bedtime after brushing teeth? Aligning doses with routines-like meals, bathing, or visiting nurses-makes it stick.
- Involve the person and their caregiver. One size doesn’t fit all. Some seniors prefer fewer pills, even if they have to take them twice a day. Others want it all in one go, even if it means a slightly bigger pill. Their preferences matter as much as the science.
The MRS GRACE tool, developed in Australia, is built around these five steps. It’s a simple checklist that pharmacists use to guide decisions. In trials, two pharmacists independently simplified the same regimens and agreed on over half the changes. That’s not perfect-but it’s a solid start.
What Gets in the Way
Even when simplification works, it’s not always done. Why?- Time. A full medication review with a pharmacist takes 45 to 60 minutes. Most doctors don’t have that kind of time during a 15-minute visit.
- Training. Only 35% of pharmacy schools teach formal medication simplification techniques. Many prescribers don’t know how to spot opportunities.
- Systems. Electronic health records rarely flag a patient’s pill burden. No alert says: “This patient takes 12 doses a day. Consider simplification.”
- Reimbursement. In most places, pharmacists aren’t paid for doing these reviews. So they don’t do them.
But change is coming. In Australia, 85% of aged care homes now include some form of regimen simplification. In Germany, pharmacists get paid extra for conducting these reviews. In the U.S., Medicare Advantage plans are starting to reward providers who reduce hospital readmissions linked to medication errors.
What Families Can Do Right Now
You don’t need to wait for a doctor’s appointment. Here’s what you can do today:- Make a list. Write down every medication, supplement, and herbal product your loved one takes. Include the dose and time. Don’t assume they remember correctly.
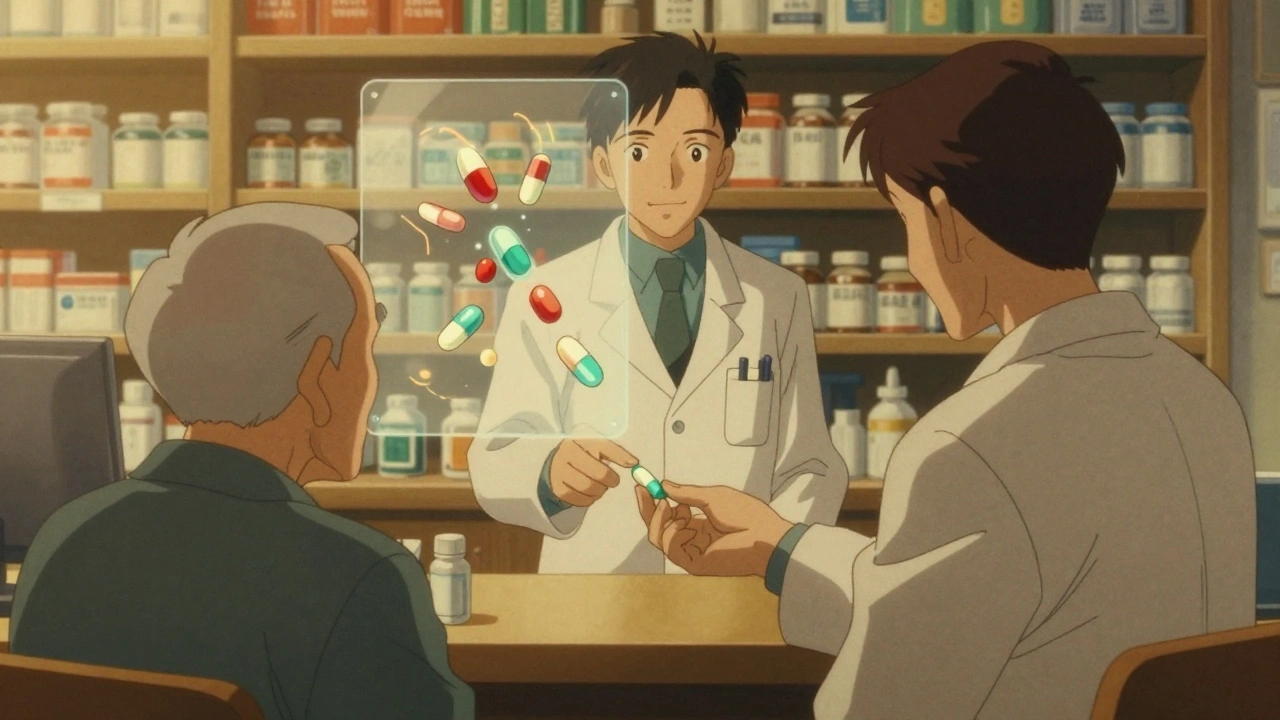
- Bring it to the pharmacy. Ask the pharmacist: “Can any of these be simplified?” Pharmacists are trained to spot this stuff. They see hundreds of regimens a week.
- Ask about generics and combinations. Is there a combo pill for blood pressure and cholesterol? Is there a once-daily version of this antidepressant?
- Watch for signs of confusion. Are pills piling up in a drawer? Are doses skipped? Are they saying, “I don’t know what this one is for”? These are red flags.
- Use a pill organizer. Not as a fix-but as a tool to see the pattern. If they need seven different pills at 8 a.m., that’s a sign the regimen is too heavy.
One woman in Durban, 78, was taking 11 pills a day. Her daughter noticed she was forgetting doses and feeling dizzy. They took her list to the pharmacist. Within two weeks, she was down to six pills-four of them once-daily combinations. Her dizziness went away. Her adherence jumped from 60% to 95%. She didn’t need more medicine. She needed less clutter.
The Bigger Picture
The global population over 65 will double by 2050. That means more people, more medications, more complexity. We can’t keep prescribing like we’re treating one condition at a time. We need to treat the whole person. Simplification isn’t about cutting corners. It’s about cutting through the noise so that medicine works for the person, not the other way around.When a senior can take their pills without stress, without confusion, without fear of making a mistake-they regain control. And that’s not just better health. It’s better life.
Can I just stop a medication if it seems unnecessary?
No. Never stop or change a medication without talking to a doctor or pharmacist. Some drugs, like blood pressure or seizure medications, can cause serious withdrawal effects if stopped suddenly. Even if a pill seems harmless-like a vitamin or herbal supplement-it could interact with other drugs. Always review with a professional first.
Are combination pills safe?
Yes, if they’re prescribed properly. Combination pills are made by pharmaceutical companies to match approved dosages. They’re tested for safety and effectiveness just like single drugs. The main risk is if the doses don’t match what the patient needs-for example, if one component is too strong or too weak. That’s why a pharmacist should always review them before switching.
What if my loved one can’t swallow pills anymore?
There are alternatives. Many medications come in liquid, dissolvable, or patch forms. Some can be crushed or mixed with food-but not all. Always check with a pharmacist. For example, extended-release pills should never be crushed. A pharmacist can help find a formulation that works with swallowing difficulties.
Does simplification mean fewer doctor visits?
Not necessarily. In fact, simplification often requires more upfront visits-to review meds, adjust doses, and monitor results. But once the regimen is streamlined, follow-ups become easier and less frequent. The goal is to reduce long-term visits caused by hospitalizations from medication errors.
How do I know if simplification worked?
Look for signs: Are pills being taken consistently? Is the person feeling less confused or overwhelmed? Are there fewer missed doses? Ask them directly: “Do you feel like your meds are easier to manage now?” Also, track refills-if they’re running out too fast or never running out, that’s a clue. And always follow up with the pharmacist or doctor after 4-6 weeks to check how things are going.






Elizabeth Crutchfield
4 December, 2025 08:16 AMi swear my grandma takes like 15 pills a day and she still forgets half of them... she just throws them in a bowl and hopes for the best. it's scary.
Michael Feldstein
5 December, 2025 18:51 PMthis is so true. my dad was on 11 meds until his pharmacist sat down with us and cut it to 5. one of them was a vitamin he'd been taking for 12 years for no reason. turned out his doctor prescribed it in 2011 and nobody ever checked.
Ashley Elliott
6 December, 2025 04:30 AMi've seen this play out in my job as a home health aide. seniors aren't lazy or forgetful-they're overwhelmed. the system is designed for single diseases, not people with 5 chronic conditions. we need to treat the whole person, not just the lab values.
Karl Barrett
6 December, 2025 16:08 PMThe pharmacokinetic and pharmacodynamic interplay of polypharmacy in geriatric populations is a non-trivial clinical challenge. The cognitive load imposed by fragmented regimens exceeds executive function thresholds in over 60% of adults over 75, per the JAMA Geriatrics meta-analysis of 2022. We must transition from disease-centric prescribing to person-centered pharmacotherapy.
George Graham
7 December, 2025 21:20 PMmy mom used to cry because she didn't understand why she needed so many pills. she'd say, 'I just want to feel okay, not take a pharmacy with me to breakfast.' it took a pharmacist coming to the house to realize half her meds weren't even helping anymore.
Augusta Barlow
8 December, 2025 23:06 PMyou know who's really behind this? Big Pharma. They don't want you to take one pill. They want you to take three separate ones so you keep buying. And don't get me started on how they lobby to block combo pills. The FDA is in their pocket. I read a whistleblower report once-
Jenny Rogers
10 December, 2025 16:21 PMIt is imperative to underscore that the simplification of medication regimens, while ostensibly benevolent, may inadvertently compromise therapeutic efficacy if not executed with rigorous clinical oversight. The conflation of convenience with clinical appropriateness represents a perilous epistemological error in medical ethics.
Heidi Thomas
12 December, 2025 03:15 AMstop pretending this is hard. if your grandpa can't keep track of pills, hire someone. or put him in a facility. stop blaming the system. people have been taking meds for 50 years. it's not rocket science.
Libby Rees
13 December, 2025 08:01 AMMy aunt took a pill organizer and started matching her doses to her TV schedule. Breakfast with the news, lunch with her soap opera, dinner with the weather. It worked. Sometimes the simplest solutions are the ones no one thinks to try.
Dematteo Lasonya
14 December, 2025 07:16 AMi love how you mentioned the MRS GRACE tool. i work with seniors in rural areas and we use it every week. it's not fancy but it works. the best part? the pharmacists actually listen. they don't just nod and move on.
Gareth Storer
15 December, 2025 17:52 PMAh yes, because nothing says 'care' like turning a 12-pill routine into a 6-pill routine. Next you'll tell me we should just give them a lollipop and call it a day. How quaint.
Shofner Lehto
16 December, 2025 11:28 AMthe real win here is when families get involved. my sister and i started helping our dad with his meds. we didn't fix everything-but we noticed he hadn't taken his blood pressure pill in three days. that led to a doctor visit. turned out his BP was sky-high. we saved him from a stroke.
val kendra
17 December, 2025 06:44 AMi'm a nurse and i can tell you-this isn't just about pills. it's about dignity. when someone can take their meds without panic, without help, without shame-that’s when they start living again. not surviving. Living.