Blood Thinner Transition Calculator
Blood Thinner Transition Calculator
Calculate safe transition times between anticoagulants and determine if bridging therapy is required based on current guidelines.
Switching between blood thinners isn’t just about changing pills-it’s a high-stakes balancing act. One wrong step, and you could end up with a stroke, a dangerous bleed, or both. For patients on long-term anticoagulation, surgery or an invasive procedure often means pausing their medication. But stopping blood thinners leaves a dangerous gap where clots can form. That’s where bridging therapy comes in. Yet, more and more evidence shows that bridging might be doing more harm than good. So when should you do it? And when should you avoid it? Let’s cut through the confusion.
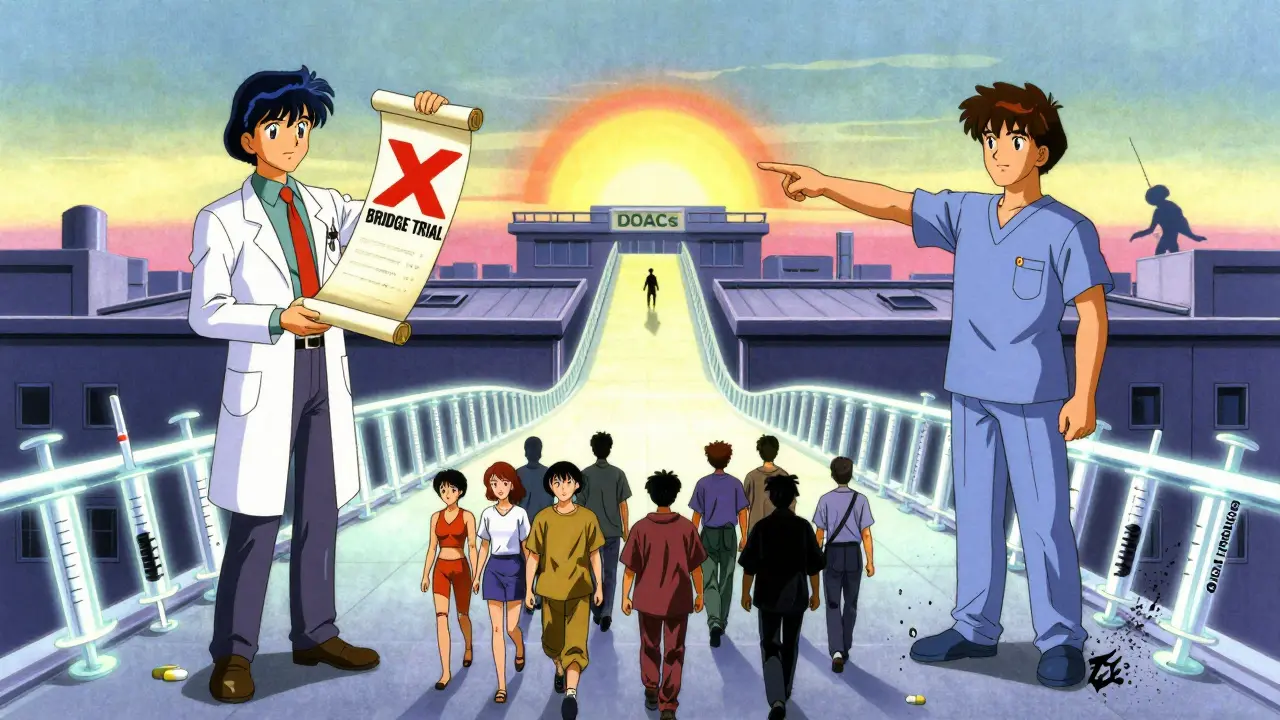
What Exactly Is Bridging Therapy?
Bridging therapy means using a short-acting anticoagulant-like low molecular weight heparin (LMWH) or unfractionated heparin-to cover the time when your main blood thinner is paused. This usually happens before surgery, a dental procedure, or any intervention where bleeding risk is a concern. The idea is simple: keep your blood from clotting during the gap. But the reality? It’s messy, risky, and often unnecessary.
For decades, doctors routinely bridged patients on warfarin. The logic was straightforward: warfarin takes days to leave your system, and its effects linger. So, inject a fast-acting heparin to fill the void. But that changed after the BRIDGE trial in 2015. This landmark study followed over 1,800 patients with atrial fibrillation who stopped warfarin for procedures. Half got heparin bridging. The other half didn’t. The results were shocking: bridging didn’t lower stroke risk at all. But it doubled the chance of major bleeding-from 1% to 2.3%. That’s not a trade-off. That’s a net loss.
Why Warfarin Needs Bridging (Sometimes)
Warfarin is old-school. It works by blocking vitamin K, but its effects are slow to start and slow to fade. It takes 5 to 6 days for warfarin to clear from your system. That’s why you stop it early before surgery. But during those days, your blood’s natural clotting ability is dropping, and you’re vulnerable. That’s the window bridging tries to cover.
Standard timing for warfarin bridging:
- Stop warfarin 5-6 days before the procedure
- Start LMWH (like enoxaparin) 3 days before the procedure
- Stop LMWH 24 hours before surgery
- Restart warfarin 12-24 hours after surgery, often at 15-20% higher dose
This schedule sounds precise, but it’s fragile. INR levels can swing unpredictably. A patient’s kidney function, diet, or even a cold can throw off the timing. And LMWH requires daily injections-often twice a day. Many patients miss doses. Studies show 15-20% non-adherence. That’s not just inconvenient. It’s dangerous.
When Bridging Is Still Necessary
Not everyone needs bridging. In fact, most don’t. Current guidelines from the American Heart Association and American College of Cardiology now restrict bridging to just two high-risk groups:
- Patients with mechanical heart valves in the mitral position-these valves are the most likely to cause clots
- Patients with a recent venous thromboembolism (VTE) within the last 3 months-meaning a blood clot in the leg or lung that’s still fresh
That’s it. If you have atrial fibrillation with a CHA₂DS₂-VASc score of 4 or lower? Skip bridging. If you had a stroke 6 months ago and your valve is in the aortic position? Skip bridging. The data doesn’t support it.
Why these two? Because the risk of clotting without anticoagulation is extreme. A mechanical mitral valve can trigger a stroke in hours if left unprotected. A recent VTE is still unstable. For these rare cases, the bleeding risk from bridging is worth the trade-off. For everyone else? The evidence says: don’t bridge. Just stop warfarin, let it clear, and restart it after the procedure.
DOACs Changed Everything
Direct oral anticoagulants (DOACs)-like apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa)-are now the first choice for 75% of new patients starting anticoagulation in 2023. And here’s the big win: you almost never need to bridge with DOACs.
Why? Because they work differently.
- They kick in within 2-4 hours
- They clear from your system in 12-17 hours (depending on kidney function)
- No INR monitoring needed
That means a simple, clean plan:
- Stop the DOAC 24-48 hours before surgery (longer if kidney function is poor)
- No injections
- Restart 6-24 hours after surgery, once bleeding risk is low
No bridging. No heparin. No daily shots. No cost. No risk of heparin-induced thrombocytopenia (a rare but deadly side effect). This is why DOACs are replacing warfarin so fast. They make anticoagulation simpler-and safer.

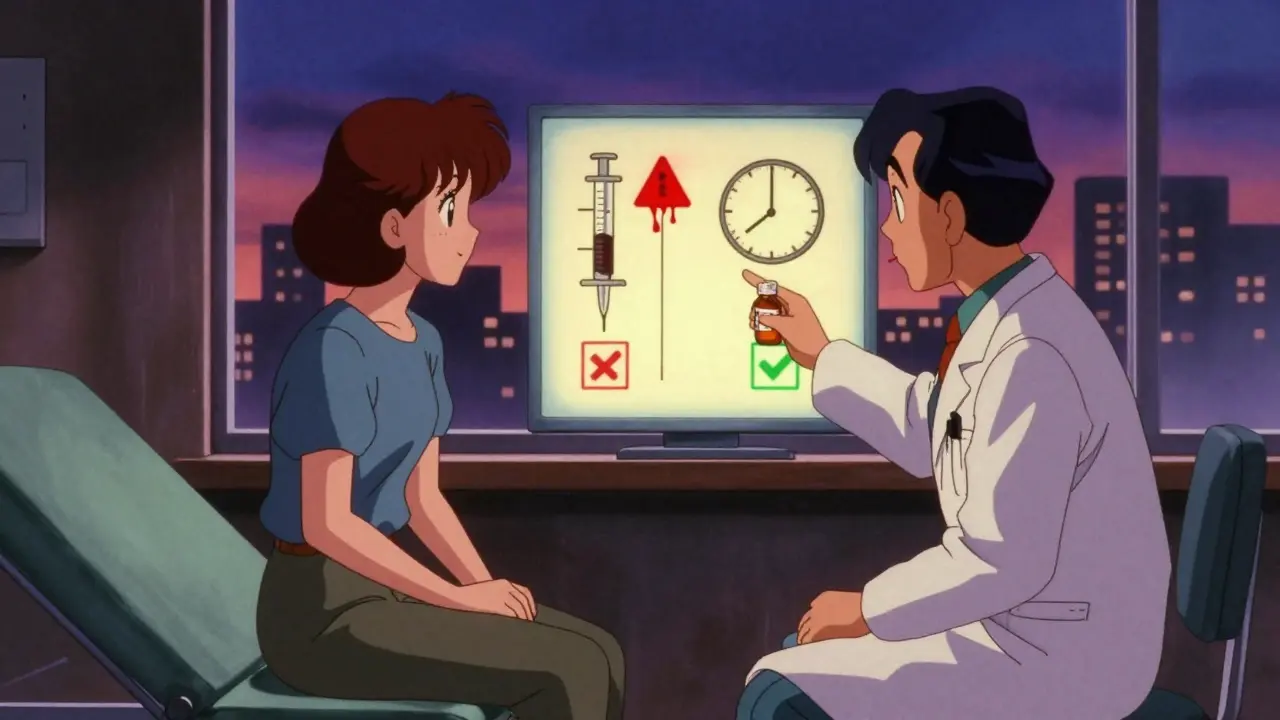
How to Transition Between Blood Thinners
Even if you’re not bridging, switching from one blood thinner to another requires precision. Here’s what actually works:
From DOAC to Warfarin
- Stop the DOAC
- Start warfarin immediately
- Give a loading dose-often 15-20% higher than your previous maintenance dose
- Check INR in 3-4 days
Why the higher dose? Warfarin takes time to build up. Starting with a boost helps avoid the gap where you’re unprotected.
From Warfarin to DOAC
- Stop warfarin when INR drops below 2.0
- Start the DOAC the next day
That’s it. No bridging. No overlap. Just wait for the INR to fall naturally. If you start the DOAC too early while INR is still high, you risk excessive anticoagulation and bleeding.
From DOAC to LMWH (if bridging is unavoidable)
- Stop DOAC
- Wait until the next dose would have been taken
- Start LMWH
- Stop LMWH 24 hours before surgery
This only applies if you’re in a very high-risk group and your doctor insists on bridging. For most people, it’s unnecessary.
The Hidden Costs of Bridging
Bridging isn’t just risky-it’s expensive. A 7-day course of LMWH in the U.S. costs $300-$500 out-of-pocket. Add in clinic visits, lab tests, and nurse instruction for injections. That’s a lot of money for something that, for most people, doesn’t help.
And then there’s the burden. Daily injections are painful. They cause bruising. They disrupt sleep and routines. Many patients refuse them. Some stop mid-course. That’s not just non-adherence-it’s a medical failure waiting to happen.
What Your Doctor Should Be Asking
A good clinician doesn’t default to bridging. They ask:
- What’s your CHA₂DS₂-VASc score? (Is it really ≥5?)
- When was your last clot? Is it still high-risk?
- Do you have a mechanical mitral valve?
- What’s your kidney function? (DOACs depend on this)
- Can you handle daily injections?
- Have you ever had heparin-induced thrombocytopenia?
If the answer to most of these is "no," then bridging is not the answer. Stopping and restarting without bridging is safer.
The New Standard: Less Is More
The old way-bridge everyone-was based on fear. Fear of stroke. Fear of lawsuits. Fear of doing nothing. But the data now tells a different story: in most cases, doing nothing is the safest thing.
The American College of Cardiology’s "Primum Non Nocere" principle-"first, do no harm"-should guide every decision. Bridging adds risk without benefit for 85% of patients. That’s not care. That’s over-treatment.
Today’s best practice? For patients on warfarin:
- Stop it 5-6 days before surgery
- Don’t bridge unless you have a mechanical mitral valve or a recent VTE
- Restart it 12-24 hours after surgery
For patients on DOACs? Even simpler:
- Stop it 24-48 hours before
- Restart it 6-24 hours after
- Never bridge
And if you’re still on warfarin? Talk to your doctor about switching to a DOAC. It’s not just easier. It’s safer. And it eliminates the whole bridging dilemma.
What If You’re Already on Bridging?
If you’re currently being bridged and you’re not in one of the two high-risk groups, ask:
- Why am I on heparin?
- What’s the evidence for this?
- Can I just stop warfarin and restart it?
Many patients are still on outdated protocols because no one questioned them. Don’t be afraid to push back. Your life isn’t a default setting.
Final Thought: Don’t Let Fear Drive Your Care
Blood thinners are powerful. But they’re not magic. You don’t need to be protected 24/7. You need to be protected smartly. The days of blanket bridging are over. The evidence is clear. For most people, the safest path is the simplest one: pause, wait, restart. No injections. No extra cost. No extra risk.
Is bridging therapy still recommended for everyone on warfarin?
No. Bridging is no longer recommended for most patients. Current guidelines restrict it to only two groups: those with mechanical heart valves in the mitral position and those with a recent blood clot (within the last 3 months). For everyone else-including most people with atrial fibrillation-bridging increases bleeding risk without reducing stroke risk. Stopping warfarin and restarting it after the procedure is safer.
Do I need to bridge if I’m on Eliquis or Xarelto?
No. Direct oral anticoagulants (DOACs) like apixaban (Eliquis) and rivaroxaban (Xarelto) don’t require bridging. They work quickly and leave your system fast-usually within 12 to 24 hours. The standard plan is to stop the DOAC 24-48 hours before surgery and restart it 6-24 hours after, depending on bleeding risk. No injections, no heparin, no extra cost.
How long should I stop warfarin before surgery?
Stop warfarin 5 to 6 days before surgery. This allows your INR to fall below the therapeutic range (usually under 2.0). If you’re in a high-risk group and bridging is needed, low molecular weight heparin (LMWH) is started 3 days before surgery and stopped 24 hours before the procedure. Always confirm your INR level before stopping warfarin.
What’s the risk of bleeding with bridging therapy?
The BRIDGE trial found that bridging increased the risk of major bleeding from 1.0% to 2.3% compared to no bridging. That’s more than double. The added risk comes from injections, overlapping anticoagulation, and the difficulty of timing doses around surgery. For most patients, this risk outweighs any small benefit in preventing clots.
Can I switch from warfarin to a DOAC to avoid bridging?
Yes. Switching from warfarin to a DOAC like apixaban or rivaroxaban is often a good option to avoid bridging altogether. The transition is straightforward: stop warfarin when your INR is below 2.0, then start the DOAC the next day. DOACs don’t require bridging, have fewer dietary restrictions, and don’t need regular blood tests. Most new patients are now prescribed DOACs because they’re safer and simpler.





Suzette Smith
12 February, 2026 05:43 AMI get that bridging is outdated, but what about the guy who had a stroke last year and swears he 'felt the clot coming' when they stopped his warfarin? I'm not saying we should bridge everyone, but maybe the data doesn't capture the ones who panic and demand it. I've seen patients cry because they 'don't trust' the new guidelines. Fear isn't always irrational. Sometimes it's just lived experience.
Alyssa Williams
14 February, 2026 02:15 AMHonestly? I switched from warfarin to Eliquis last year and my life changed. No more weekly blood draws. No more bruised belly from shots. No more wondering if my broccoli intake is gonna kill me. I was skeptical at first but now I’m like - why did we ever do it the hard way? DOACs are the future and anyone still pushing bridging for AFib is just stuck in 2012.
Sonja Stoces
15 February, 2026 11:31 AMThe BRIDGE trial? LOL. You think that’s the whole story? What about the 2022 meta-analysis from the Lancet that showed bridging still has a 0.7% reduction in stroke in high-risk AFib patients with prior TIA? You’re cherry-picking. And don’t even get me started on how DOACs are a pharmaceutical cash cow. They cost 10x more. Who benefits? Not you. Not your insurance. Definitely not the hospital.
Also - 'no bridging' sounds nice until you’re the one with a mechanical mitral valve and your INR drops to 0.9 because you forgot your pill. Then you’re the one begging for heparin.
Also also - I’m a nurse. I’ve seen 3 strokes from 'no bridging' in the last 6 months. Just saying.
Luke Trouten
16 February, 2026 11:03 AMThere’s a quiet tension here between safety and autonomy. The guidelines say 'don’t bridge' - but what if the patient doesn’t feel safe? Medicine isn’t just data. It’s trust. And sometimes, the act of bridging - even if statistically unnecessary - restores psychological safety. Is that worth something? Maybe we’re too quick to call fear 'irrational.' Maybe we need to ask: not 'is this evidence-based?' but 'is this human-based?'
Kristin Jarecki
16 February, 2026 20:03 PMThe clinical recommendations presented here are aligned with the 2023 AHA/ACC/HRS Guideline for the Management of Atrial Fibrillation. The restriction of bridging therapy to patients with mechanical mitral valves or recent venous thromboembolism within the past three months is supported by Class I evidence. Furthermore, the avoidance of bridging in patients on direct oral anticoagulants is classified as a Class I recommendation with Level A evidence. Clinicians are advised to individualize decisions based on thrombotic and hemorrhagic risk stratification tools, including CHA₂DS₂-VASc and HAS-BLED scores. Documentation of shared decision-making is strongly encouraged.
Jonathan Noe
16 February, 2026 22:23 PMBro, I work in a clinic. I’ve seen 40 patients switch from warfarin to DOACs in the last 6 months. Guess what? Not one of them went back. Not one. They all say the same thing: 'I didn’t realize how much I hated the shots and the blood tests.' And the best part? No one’s had a stroke. No one. Meanwhile, the guy who got bridged last month? He had a hematoma the size of a grapefruit from the heparin. So yeah - DOACs win. Every time. Stop overcomplicating it.
Jim Johnson
16 February, 2026 22:33 PMI had to bridge twice. Both times I was terrified. I didn’t sleep. I kept checking my INR. I was getting injections at 2am. My arm was black and blue. I thought I was saving myself from a stroke. But now I know - I was just scared. After I switched to Eliquis, I stopped worrying. I just take my pill. No shots. No blood tests. No panic. I wish someone had told me earlier that I didn’t need to suffer like that. You’re not weak for wanting to avoid injections. You’re smart.
Skilken Awe
17 February, 2026 16:18 PMOh wow. Another feel-good post about DOACs. Let me guess - you’re either a pharma rep or a patient who got a free sample. Bridging isn’t about fear. It’s about pharmacokinetics. You think a 72-year-old with CrCl 35 and a history of DVT can just 'stop and restart' a DOAC? You don’t get it. The guidelines are for textbook cases. Real life? We’re managing 7 comorbidities, 12 meds, and a patient who can’t afford the DOAC. So yeah - sometimes we bridge. Because we’re not playing with data. We’re playing with lives. And you? You’re just typing from your couch.