It’s a counterintuitive truth: generic drug prices in the United States are often lower than in Europe-even though Americans pay far more for brand-name drugs. If you’ve ever been shocked by the $4 price tag for generic lisinopril at Walmart, only to hear someone in Germany say they paid €15 for the same pill, you’re not imagining things. The data backs it up. In 2022, the U.S. Department of Health and Human Services found that Americans paid, on average, 33% less for unbranded generics than residents of 33 other OECD countries. Meanwhile, the same report showed the U.S. paid over 4 times more for brand-name drugs than most of Europe.
Why Are Generic Drugs Cheaper in the U.S.?
The answer isn’t about better manufacturing or cheaper labor. It’s about competition-and how broken the system is in Europe.
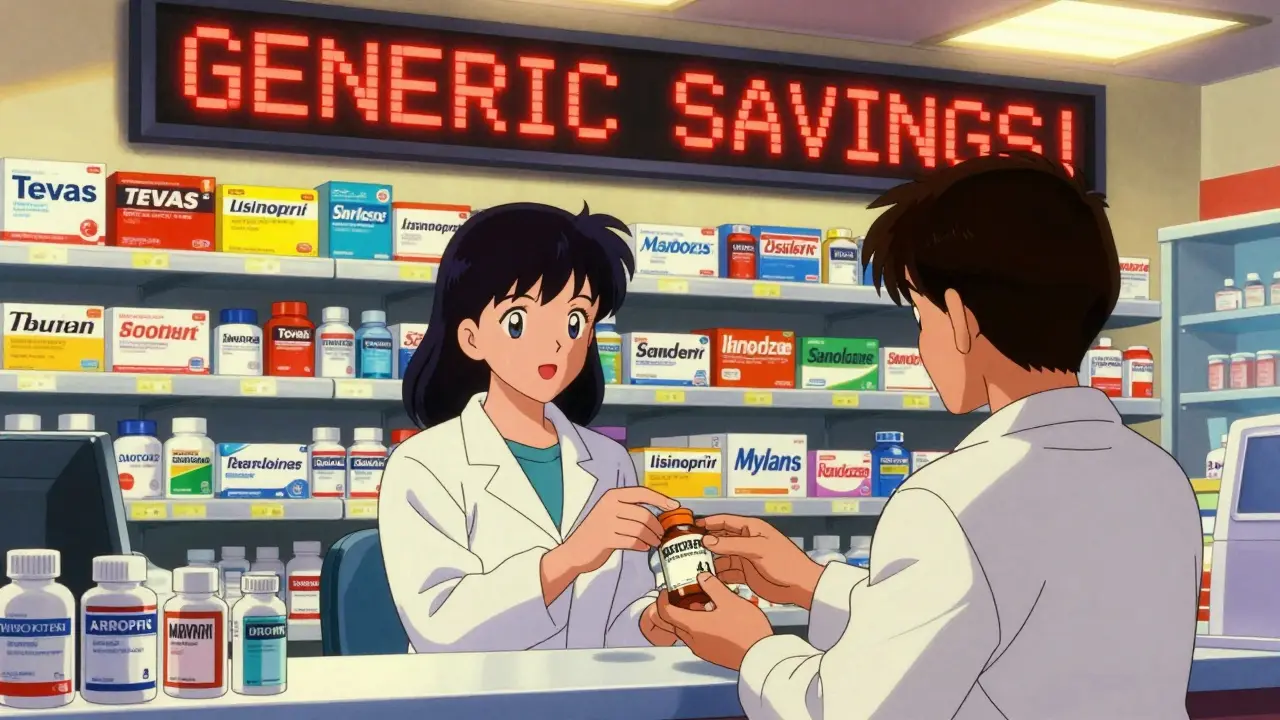
In the U.S., generic drugs make up about 90% of all prescriptions filled. That’s not an accident. Once a patent expires, dozens of companies rush to make the same drug. Teva, Mylan, Sandoz, and others compete fiercely. They don’t just undercut each other-they undercut manufacturing costs. Some generics are sold below cost just to keep shelf space. This creates a race to the bottom, and consumers win.
Pharmacy Benefit Managers (PBMs) amplify this. These middlemen negotiate bulk discounts with drugmakers and pharmacies. They don’t always pass savings to patients, but they do pressure manufacturers to slash prices. The result? A monthly supply of generic metformin can cost $0-$10 with insurance, sometimes even less without it.
Europe doesn’t have this. Generic drug use is only around 41% of prescriptions. Why? Because many countries restrict substitution. In France, a pharmacist can’t swap a brand-name drug for a generic without the doctor’s okay. In Germany, pharmacists can substitute-but the system doesn’t reward them for doing it. There’s no financial incentive to push cheaper options. So, patients get the brand, even when the generic is identical.
How Europe Sets Drug Prices
European countries don’t let the market decide. Governments do.
In Germany, France, and the UK, price regulators set what a drug can cost. They don’t look at what it costs to make. They look at whether it’s worth the price. The UK’s NICE evaluates if a drug offers enough health benefit to justify its cost. If not, it’s denied coverage. Other countries use reference pricing: they look at what other nations pay and set their own price below that.
This keeps brand-name drug prices low-but it also kills competition for generics. Why would a company invest in making a generic if the government will cap the price so low that there’s no profit? The result: fewer manufacturers enter the market. Less competition means higher prices for consumers.
Compare that to the U.S., where the same generic drug can be made by 15 different companies. Even if one shuts down, another steps in. In Europe, if two manufacturers exit a market, the remaining one can raise prices without fear.
The Brand-Name Paradox
Here’s where things get strange. The U.S. pays the most for new, patented drugs. A 2024 Health System Tracker analysis found that Medicare’s negotiated price for Jardiance was $204 per month-nearly four times what it costs in the UK, Germany, or Japan. Stelara? $4,490 in the U.S. versus $2,822 elsewhere.
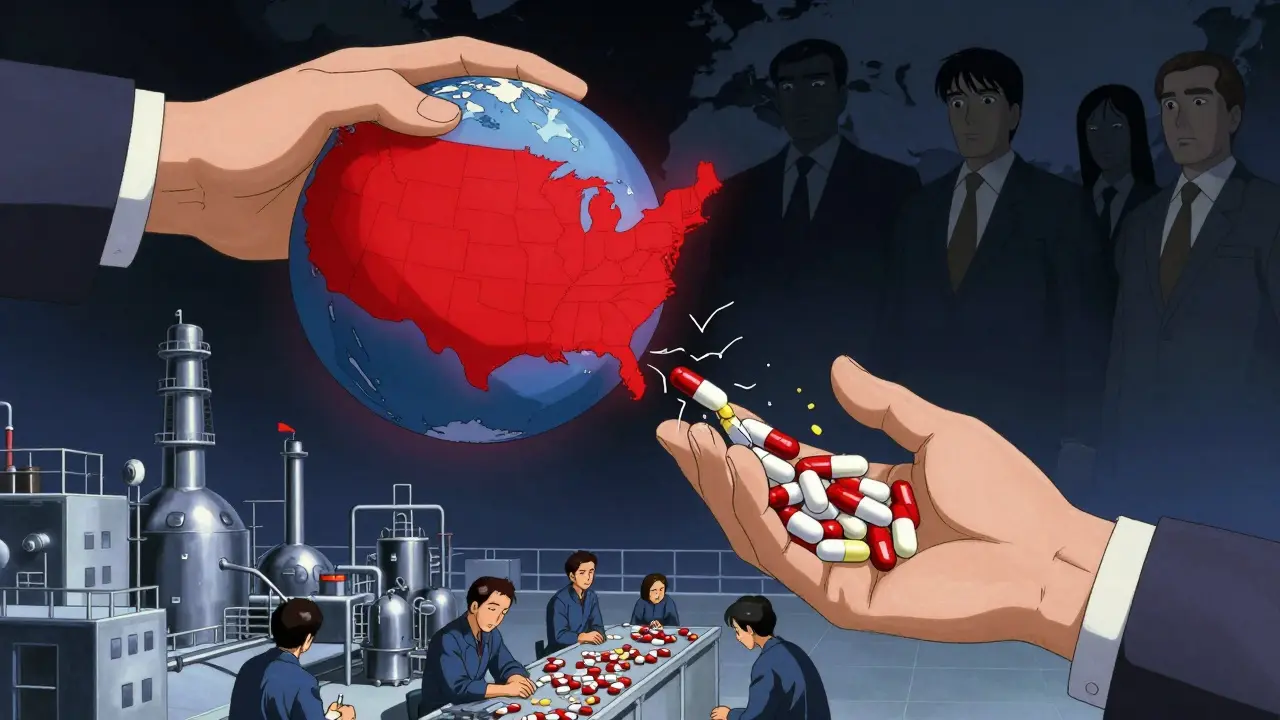
Why? Because the U.S. is the world’s biggest payer for innovation. About two-thirds of global pharmaceutical R&D is funded by American consumers and insurers. Drugmakers know they can charge more here, so they do. Europe, Canada, and Australia benefit from those high prices-they pay less because they negotiate hard, but they still get the drugs developed in the U.S.
That’s why experts call it “free riding.” The U.S. shoulders the cost of discovery. Everyone else gets the benefit. Dana Goldman from the University of Southern California put it plainly: “Europe negotiates prices as low as they can without regard to the cost of innovation.”
What Happens When Prices Go Too Low?
The U.S. generic market isn’t perfect. Sometimes, it works too well.
When competition drives prices below what it costs to produce a drug, manufacturers quit. In 2021, a generic version of a common heart medication disappeared because no one could make it profitably. Then, one company bought up the remaining production capacity-and raised the price 1,000% overnight.
This isn’t rare. The FDA reports that generic drug shortages have more than doubled since 2015. Most are caused by low prices, not supply chain issues. When profit margins vanish, companies leave. And when only one or two are left, they control the market.
Europe doesn’t have this problem-because prices never drop that low. But it has another: limited access. If no one makes a generic because the price is too low, patients in Europe still pay more for the brand. In the U.S., they might get it for free-or not at all.
What’s Changing in 2025?
The Inflation Reduction Act is the biggest shift in U.S. drug pricing in decades. For the first time, Medicare can negotiate prices for a handful of expensive brand-name drugs. The first 10 drugs selected include Jardiance, Stelara, and others. Their negotiated prices are still higher than in Europe-but they’re down 25-40% from what they were.
That’s putting pressure on drugmakers. If Medicare can force down prices on top-selling drugs, why can’t private insurers? Some PBMs are already following suit.
Meanwhile, Europe is watching. The European Commission’s 2025 pharmaceutical strategy admits that current pricing models may threaten access to new drugs. If U.S. prices fall, companies might raise prices elsewhere to make up the difference. That’s what Alexander Natz of EUCOPE warned about: if the U.S. caps prices, manufacturers will hike them in Germany or France.
And then there’s the political threat. Former President Trump’s proposed “most favored nation” rule would force the U.S. to pay the same price as the lowest-paying OECD country. If enacted, it could slash U.S. brand-name drug costs-but at the cost of global R&D funding.
What This Means for You
If you’re in the U.S. and take generics: you’re getting a deal. Most are dirt cheap. Use your pharmacy’s $4 list. Ask for generics. Switch when you can.
If you’re in Europe and frustrated by high prices: you’re not alone. But you’re also not paying for innovation. The U.S. system is messy, unfair, and sometimes broken-but it’s the engine that keeps new drugs coming.
For global health, this isn’t sustainable. The U.S. can’t keep paying 4 times more for brand-name drugs forever. Europe can’t keep paying so little forever either. Somewhere in between, there’s a balance. But right now, the system works like this: Americans pay less for old drugs, and way more for new ones. Everyone else pays less for everything.
It’s not fair. But it’s how it is.
Why are generic drugs cheaper in the U.S. than in Europe?
The U.S. has a highly competitive generic market with dozens of manufacturers, aggressive pricing by Pharmacy Benefit Managers (PBMs), and automatic generic substitution at pharmacies. In contrast, European countries use government price controls, restrict pharmacist substitution, and limit competition-leading to higher prices for the same generic drugs.
Do Americans really pay less for generic drugs?
Yes. According to the U.S. Department of Health and Human Services’ 2022 analysis, U.S. generic drug prices were 67% of the average in 33 OECD countries. For example, a month’s supply of generic lisinopril costs about $4 in the U.S. but €15 in Germany. This is due to volume-based discounts and fierce competition among manufacturers.
Why do U.S. brand-name drugs cost so much more than in Europe?
The U.S. doesn’t regulate brand-name drug prices. Drugmakers set high prices because they know insurers and patients will pay them. This high revenue funds about two-thirds of global pharmaceutical research. European countries negotiate prices based on cost-effectiveness and use reference pricing to keep costs low, often paying less than half of U.S. prices for the same drugs.
Can the U.S. lower brand-name drug prices without hurting innovation?
It’s possible, but risky. The Inflation Reduction Act’s Medicare negotiation program is testing this by lowering prices for 10 drugs. Early results show savings without halting new drug development. But if U.S. prices fall too far, manufacturers may raise prices in Europe or cut R&D spending. Experts warn that global innovation depends on U.S. spending-so any drastic cuts could slow new drug approvals worldwide.
Are generic drug shortages a problem in the U.S.?
Yes. When competition drives prices below manufacturing costs, companies stop making the drug. Between 2015 and 2024, generic shortages more than doubled. The FDA reports that low profitability-not raw material shortages-is the main cause. Once a market consolidates, the remaining supplier can raise prices dramatically, creating cycles of scarcity and spikes.
Should Europe copy the U.S. generic pricing model?
Not exactly. The U.S. model works because of its size, private insurance system, and PBM power-things Europe doesn’t have. But Europe could improve by allowing more pharmacist substitution, encouraging generic competition, and reducing bureaucratic barriers. The goal shouldn’t be to copy the U.S.-but to create a system that ensures both affordability and steady supply without sacrificing innovation.
How does the U.S. generic market affect global drug supply?
The U.S. is the largest market for generic drugs, so manufacturers prioritize it. If a company can make a profit selling to the U.S., it can afford to supply smaller markets. When U.S. prices drop too low, production shifts overseas or stops entirely-causing global shortages. So, U.S. pricing decisions directly impact whether a generic drug is available in Canada, Australia, or even parts of Europe.



Kevin Narvaes
20 January, 2026 20:38 PMso like... america pays less for generics but more for brand names? wow. that makes total sense. also why does my heart med cost $3 but in europe they pay like 15 bucks? someone explain this to my grandma. she thinks we're all getting ripped off. lol
Sangeeta Isaac
21 January, 2026 23:45 PMthe u.s. generic market is basically a bloodsport where companies sell pills below cost just to stay on the shelf. it’s chaotic, it’s wild, and honestly? kinda beautiful. we got a $4 lisinopril while europeans are stuck paying €15 because their system’s too polite to let competition happen. also pbms are sketchy but they’re the reason my metformin is free. 🤷♀️
Alex Carletti Gouvea
23 January, 2026 17:54 PMlet me get this straight-americans are the suckers paying for all the world’s drug research, while europeans sit back and get cheap generics? that’s not free riding, that’s theft. we build the future and they steal the blueprint. if you want cheap drugs, go make your own damn pills. we’re not your pharmacy.
Philip Williams
25 January, 2026 08:21 AMThe structural differences between U.S. and European pharmaceutical markets are profound. The U.S. operates under a decentralized, market-driven model that incentivizes competition among manufacturers, while European systems rely on centralized price controls that suppress entry. This results in lower generic prices in the U.S., but at the cost of systemic vulnerability to supply chain collapse when margins vanish. The trade-off is not merely economic-it is public health.
Ben McKibbin
26 January, 2026 00:53 AMthis whole system is a mess, but not in the way people think. yeah, we get cheap generics because we have 15 companies fighting over pennies-but that’s why drugs disappear when no one can profit. europe’s system is rigid, sure, but at least you don’t wake up one day and your blood pressure med costs $200 because one company owns the factory. we need a middle ground: competition that doesn’t kill supply.
Melanie Pearson
26 January, 2026 02:17 AMthe fact that americans are subsidizing global pharmaceutical innovation through exorbitant brand-name prices is not a feature-it is a national disgrace. we are the world’s financial punching bag, and our government refuses to acknowledge it. if you think this is sustainable, you’re delusional. this isn’t capitalism. it’s feudalism with pill bottles.
Jerry Rodrigues
27 January, 2026 22:08 PMi just buy my generics at walmart for $4 and don't think about it much. but yeah the whole thing is wild. europe pays more for the same thing? weird. but also... i guess i'm lucky?
Uju Megafu
28 January, 2026 15:41 PMthis is why africa gets left behind. america eats the innovation costs, europe gets cheap drugs, and the rest of the world? they get nothing. you think your $4 pill is a win? what about the people in Lagos who can’t get ANY generic because the factories moved to the U.S. market? you’re not saving money-you’re stealing from the global poor. #GlobalHealthJustice
Jarrod Flesch
28 January, 2026 20:51 PMmate, i live in australia and we pay like $10 for generics here. we’re kinda stuck in the middle. we get some of the innovation from the U.S. but our government negotiates like europe. still, i’ve seen shortages too-my dad’s thyroid med vanished for 6 months. it’s not just a u.s. problem. we’re all connected. 🤝
Kelly McRainey Moore
30 January, 2026 16:45 PMmy pharmacist gives me the generic every time and i’m so grateful. honestly i didn’t even know there was a system behind it. i just know i’m not paying $200 for blood pressure pills. 🙏
Stephen Rock
1 February, 2026 02:51 AMthe u.s. is the world’s drug lab. we fund it. europe plays the victim. and now they want to copy our system? nah. they got it easy. we got the pain. they got the price tags. if they want cheaper drugs, they can build their own pharma industry. until then, shut up and pay your taxes
Amber Lane
1 February, 2026 19:17 PMthe real story isn’t prices. it’s access. if a drug disappears in the U.S., it vanishes globally. if it’s capped in Europe, it never gets made. we need both competition and stability. not one or the other.
Gerard Jordan
2 February, 2026 09:03 AMthis is why i love my job. i help people get their meds for $4 and they don’t even know the history behind it. 🌍💊 it’s wild that one country’s chaos helps the world. but yeah, the shortages? real. we need better rules. not just more yelling.