When you hear the word biosimilar, you might think it’s just like a generic pill-cheaper, same effect, no big deal. But biologics aren’t pills. They’re complex proteins made in living cells, and their biosimilars aren’t exact copies. They’re incredibly close, but not identical. And that tiny difference? It can sometimes trigger your immune system in ways the original drug never did.
Why Your Body Might React Differently
Biologics like Humira or Enbrel are made using living cells-usually Chinese hamster ovary cells. These cells tweak the protein after it’s made, adding sugar molecules (glycans), changing how the protein folds, or adding tiny chemical tags. That’s called post-translational modification. Even small shifts in those changes-like more or less sialic acid, or different galactose patterns-can turn a harmless protein into something your immune system sees as foreign. That’s immunogenicity. It’s not rare. Up to 70% of patients on some monoclonal antibodies develop anti-drug antibodies (ADAs). These aren’t always bad. Some just stick to the drug and clear it faster. But when they block the drug’s active site or cause inflammation, that’s when things get dangerous. Think anaphylaxis with cetuximab, or reduced effectiveness in rheumatoid arthritis patients who suddenly stop responding to their TNF blocker. Biosimilars are built to match the original. But if the manufacturer uses a different cell line, or a different purification process, those sugar tags might look slightly different. One study found that protein aggregates-tiny clumps of misfolded protein-over 5% of the total product increased ADA risk by more than three times. Host cell proteins left behind from manufacturing? More than 100 parts per million? That’s linked to an 87% higher chance of your body attacking the drug.How You’re Treated Matters Just as Much
It’s not just about the drug. It’s about how you get it. Subcutaneous injections-like those for adalimumab or etanercept-carry a 30-50% higher immunogenicity risk than intravenous infusions. Why? Because the drug sits under your skin for hours, slowly leaking into immune-rich tissue. Your dendritic cells have time to grab it, process it, and show it to your T cells. IV delivery? It goes straight into your bloodstream. Less exposure. Less chance for your immune system to notice. Dosing frequency plays a role too. If you’re getting a shot every week, your immune system gets constant reminders. Intermittent dosing? That’s like waving a flag in front of your immune cells every few months. It’s more likely to react. And the longer you’re on the drug? The more likely your immune system will break tolerance. After six months, ADA rates start climbing steadily. Then there’s what else you’re taking. Methotrexate, a common RA drug, cuts ADA formation by 65% for TNF inhibitors. Why? It suppresses the immune cells that make antibodies. Patients on combo therapy rarely develop ADAs. Those on monotherapy? Much higher rates.Your Genetics and Health Play a Part
Not everyone reacts the same. Your genes matter. People with the HLA-DRB1*04:01 allele are nearly five times more likely to develop ADAs against certain biologics. That’s not a guess-it’s backed by multiple studies. If you’re of European descent and have rheumatoid arthritis, your odds of having this gene are higher. That’s one reason why immunogenicity rates vary across populations. Your disease state matters too. Healthy volunteers show low ADA rates. Patients with active rheumatoid arthritis? Their immune systems are already revved up. Studies show they’re 2.3 times more likely to develop ADAs than healthy people given the same drug. Inflammation breaks immune tolerance. It’s like your body is already on high alert-and the drug is just another thing to attack. Even your immune status changes things. If you’re on chemotherapy or have HIV, your ADA rates drop. Why? Because your immune system is too weak to mount a strong response. That’s not a good thing-it just means the drug might stay active longer, but you’re also more vulnerable to infections.
Are Biosimilars Really Different? The Evidence
Let’s cut through the noise. Do biosimilars cause more immunogenicity? The data is messy-but mostly reassuring. The NOR-SWITCH trial, which followed 481 patients switching from originator infliximab to its biosimilar CT-P13, saw a small uptick in ADA rates: 8.5% vs. 11.2%. But no one had worse outcomes. No more flares, no more hospitalizations. The same was true in a large 2021 rheumatoid arthritis study of 1,247 patients: 12.3% on the original, 11.8% on the biosimilar. No difference. But then there’s the Danish registry. For adalimumab, Humira had a 18.7% ADA rate. Amgevita, the biosimilar? 23.4%. Statistically significant. But here’s the kicker: patients on both drugs still responded just as well to treatment. No drop in remission rates. No increase in side effects. Real-world Reddit threads tell another story. One patient reported severe injection site reactions after switching from Enbrel to its biosimilar. Another switched from Rituxan to Rixathon and saw zero difference after three years. Both are real. Neither is the whole picture. The American College of Rheumatology surveyed 347 rheumatologists. Two-thirds said immunogenicity concerns are overblown. One in five say they’ve seen real differences in practice. That’s not a contradiction. It’s reality. For most, it’s fine. For a few, it’s not.How Regulators Check for Differences
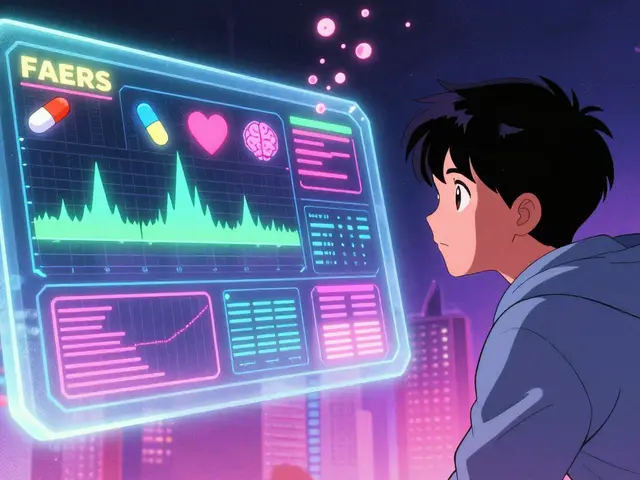
The FDA and EMA don’t just approve biosimilars based on a few lab tests. They demand a full picture. First, analytical studies. Thousands of comparisons: protein structure, glycosylation patterns, charge variants, aggregation levels. Then functional tests: does it bind to the same receptors? Does it trigger the same cell death in cancer cells? Then animal studies. Then human trials. The immunogenicity part? It’s the hardest. You can’t just compare one assay. You need the same test, done the same way, on the same patients. That’s why head-to-head trials are required. If one study uses electrochemiluminescence (ECL) and another uses ELISA, you’re comparing apples to oranges. ECL can detect ADAs in 13% of patients. ELISA? Maybe 5%. That’s not a drug difference-that’s a method difference. Neutralizing antibodies? Those need cell-based assays. They’re less precise-25-30% variation-but they show if the antibody actually blocks the drug’s function. That’s what matters clinically. And formulation? That’s sneaky. Rixathon uses polysorbate 80. Rituxan uses polysorbate 20. One might cause more protein clumping. That’s not a biosimilar flaw-it’s a formulation choice. But regulators now require manufacturers to prove those stabilizers don’t increase immunogenicity risk.
What’s Next? Better Tools, Better Safety
The future is in precision. By 2027, advanced mass spectrometry will be able to map glycosylation patterns at 99.5% accuracy. That means we’ll know if a biosimilar’s sugar tags are truly identical to the original-not just "similar enough." Some labs are already combining proteomics, glycomics, and immunomics. They’re not just looking at the drug. They’re looking at how your immune cells respond to it. At UCSF, clinical trials are using these multi-omics tools to predict who’s at risk before they even start treatment. The goal isn’t to make every biosimilar perfect. It’s to know which ones are safe for which patients. For most people, biosimilars work just fine. For a small group? We’re getting better at spotting who might react-and why.Bottom Line
Biosimilars aren’t generics. They’re not copies. They’re near-identical twins with tiny differences. Those differences can, in rare cases, trigger immune responses that the original drug didn’t. But for the vast majority, they’re just as safe and effective. The key takeaway? Don’t assume all biosimilars are the same. Don’t assume your body will react the same way to every version of the same drug. If you switch and notice new side effects-rash, fatigue, joint pain, or loss of effectiveness-talk to your doctor. It might not be your disease flaring. It might be your immune system reacting to a new version of the drug. The science is evolving. The data is growing. And for now, the evidence says: biosimilars are a win for affordability, and mostly, a win for safety too.Can biosimilars cause more side effects than the original biologic?
Biosimilars are designed to have no clinically meaningful differences in safety or efficacy. Most large studies show side effect rates are nearly identical. But in rare cases, minor manufacturing differences-like glycosylation patterns or protein aggregates-can trigger immune reactions in susceptible individuals. These reactions aren’t more common overall, but they can happen. If you notice new symptoms after switching, report them to your doctor.
Why do some people develop anti-drug antibodies and others don’t?
It’s a mix of biology and environment. Genetics play a big role-certain HLA alleles make you more prone. Your disease state matters too; active inflammation increases risk. How you’re dosed (subcutaneous vs. IV), how often you get the drug, and whether you’re on methotrexate or another immune modulator all affect your odds. Even your gut microbiome may influence immune responses, though that’s still being studied.
Are biosimilars tested for immunogenicity before approval?
Yes. Regulators require head-to-head clinical trials comparing immunogenicity between the biosimilar and the reference product. These trials use identical testing methods-same assay, same patient population, same timing. The goal is to prove any differences in anti-drug antibody rates are not clinically meaningful. If the biosimilar shows higher ADA rates, developers must explain why and prove it doesn’t affect safety or effectiveness.
Can I switch back to the original biologic if I have a reaction to a biosimilar?
Yes. If you experience new side effects, loss of effectiveness, or signs of an immune reaction after switching to a biosimilar, your doctor can switch you back. Many patients do so safely. There’s no evidence that switching back increases risk. The key is monitoring: if symptoms appear after a switch, consider immunogenicity as a possible cause.
Do biosimilars have the same long-term safety profile as the original?
Real-world data over 10+ years shows that biosimilars like CT-P13 (infliximab biosimilar) have long-term safety profiles matching the original. No increased risk of infections, cancer, or serious adverse events. For newer biosimilars, data is still accumulating, but regulatory agencies require at least 5 years of post-market surveillance. So far, the trend holds: safety is comparable.




Sean Hwang
13 November, 2025 03:56 AMso i switched to a biosimilar last year and honestly? no difference. my joints still hurt the same, no rashes, no weird fatigue. maybe my body just doesn't care about the sugar tags.
Brittany C
14 November, 2025 00:08 AMThe glycosylation heterogeneity observed in biosimilar manufacturing profiles is not merely a technical artifact-it represents a fundamental deviation in post-translational modification fidelity that can modulate FcγR binding kinetics and dendritic cell uptake efficiency. The clinical implications are non-trivial.
Barry Sanders
14 November, 2025 00:49 AMAnother placebo-driven delusion. If your body reacts to a biosimilar, you're weak. Get over it.
Sean Evans
15 November, 2025 18:20 PMLOL. People still think biosimilars are safe? My cousin got anaphylaxis switching from Humira to Amgevita. They told her it was "just anxiety." 😂
Ryan Anderson
17 November, 2025 05:44 AMJust want to say thank you for writing this. So many people don’t get how complex biologics are. This is the kind of info that actually helps.
gent wood
18 November, 2025 18:59 PMI’ve been on biosimilars for five years now-three different ones-and I’ve never had an issue. But I also take methotrexate, and I stick to IV infusions. Maybe that’s why. It’s not the drug-it’s the combo.
Scarlett Walker
20 November, 2025 16:28 PMMy doc switched me to a biosimilar and I felt like a zombie for two weeks. I went back to the original and boom-back to normal. I didn’t think it was the drug, but now I know. Always listen to your body.
Anjan Patel
21 November, 2025 12:40 PMLet me tell you something-this whole biosimilar thing is a corporate scam. Big Pharma doesn’t want you to know that the "cheap" version might make you sicker. They’re cutting corners and you’re the lab rat.
kshitij pandey
22 November, 2025 01:23 AMAs someone from India where biosimilars are the only option for most, I want to say: yes, they work. Not for everyone, sure-but for thousands of us, they’re a lifeline. Don’t throw them out because of a few scary stories.
Hrudananda Rath
22 November, 2025 08:25 AMOne must contemplate the epistemological dissonance inherent in the regulatory paradigm: the FDA’s insistence on analytical equivalence, while simultaneously acknowledging that immunogenicity is a phenomenological outcome shaped by individualized immune ontologies. This is not science-it is bureaucratic mysticism.
Ashley Durance
22 November, 2025 21:12 PMAnyone who says biosimilars are "just as safe" hasn’t read the real data. The Danish registry alone shows a 25% spike in ADA. And they’re just brushing it off? That’s negligence.
Eleanora Keene
23 November, 2025 11:10 AMHey, I’m not a doctor, but I’ve been tracking my ADA levels since switching. Mine went up a bit, but my symptoms didn’t get worse. So maybe it’s not the end of the world? Just… keep an eye on it.
Chris Ashley
24 November, 2025 07:37 AMbro why are you even worried? just take the cheap one. if it stops working, switch back. it’s not rocket science.
Nathan Hsu
25 November, 2025 20:26 PMLet’s not forget: the original biologic was tested on 5,000 people over 15 years. Biosimilars? Often 300 people over 1 year. That’s not science-it’s a gamble.
Scott Saleska
27 November, 2025 02:58 AMActually, the EMA requires 5 years of post-market surveillance for all biosimilars, and the data from CT-P13 shows no increased risk of serious infections or malignancies. You’re cherry-picking outliers.