Hemorrhoid Fiber Tracker Calculator
Calculate Your Daily Fiber Intake
Track your fiber consumption from whole foods to meet the recommended 25-35g per day for hemorrhoid prevention and relief.
Current Intake
This tool estimates fiber content from whole food sources. For accurate tracking, always check food labels and consult a healthcare professional for personalized advice.
When you feel a dull ache or notice bleeding after a bathroom visit, the first thought is often uncomfortable, but the solution can be as simple as reshaping what’s on your plate.
Key Takeaways
- Increasing dietary fiber reduces straining, a major trigger for hemorrhoids.
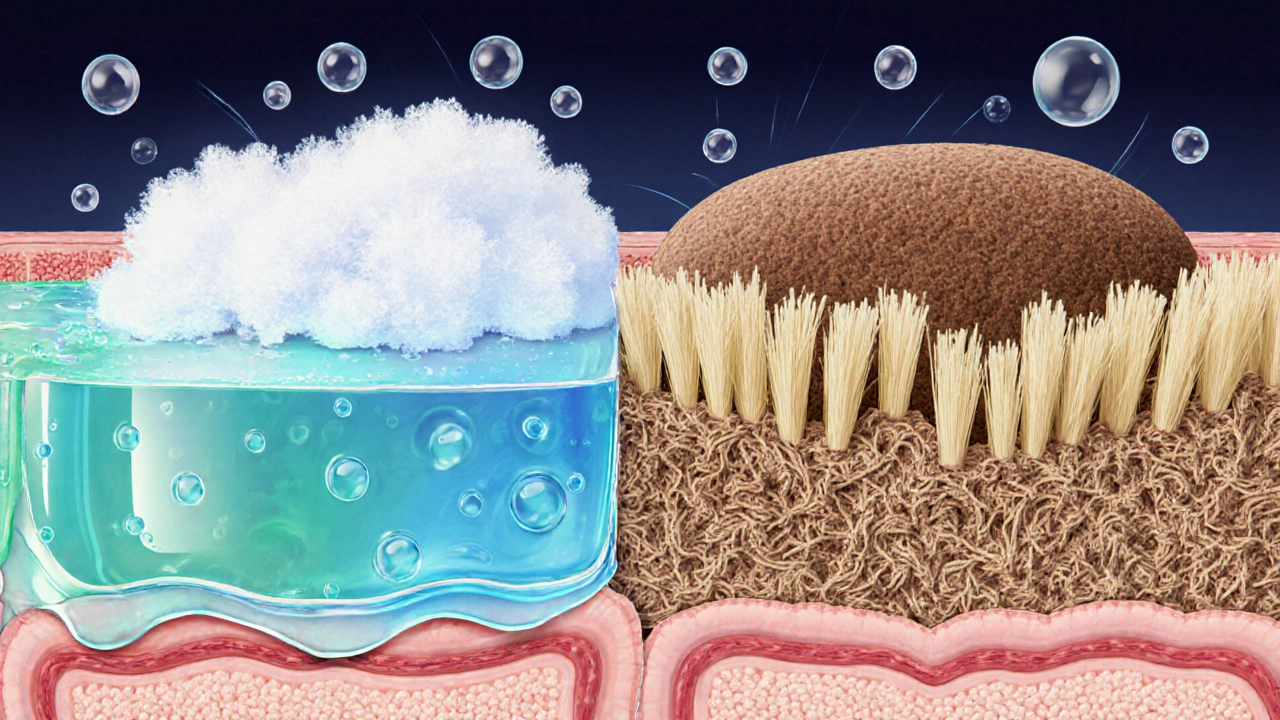
- Soluble and insoluble fibers work together to soften stool and add bulk.
- Whole grains, fruits, vegetables, and legumes are the most effective natural sources.
- A daily goal of 25‑35g of fiber, paired with adequate water, keeps bowel movements regular.
- Gradual changes prevent gas, bloating, and temporary discomfort.
Dietary fiber is a plant‑based carbohydrate that passes through the digestive tract largely unchanged, adding bulk to stool and nurturing beneficial gut bacteria. When fiber intake is low, stools become hard and dry, forcing you to push harder during bowel movements. That extra pressure is what inflames the veins around the rectum, leading to hemorrhoids swollen vascular cushions in the anal canal that can cause pain, itching, and bleeding. By boosting fiber, you give your colon an easier job, lessen straining, and give those veins a chance to heal.
Why Fiber Matters for Hemorrhoid Health
Two main mechanisms protect you:
- Stool bulk: Insoluble fibers absorb water, increasing stool volume and speeding up transit time.
- Stool softness: Soluble fibers dissolve into a gel‑like substance that holds onto water, making each bowel movement smoother.
When both processes happen, you experience fewer episodes of hard, pebble‑like stools that trigger that uncomfortable pressure.
Understanding Soluble vs. Insoluble Fiber
Not all fiber is created equal, and knowing the difference helps you plan a balanced diet.
| Attribute | Soluble Fiber | Insoluble Fiber |
|---|---|---|
| Typical Sources | Oats, barley, beans, apples, citrus fruits | Whole‑grain wheat bran, nuts, seeds, cauliflower, skin of fruits |
| Water Interaction | Forms a viscous gel that slows digestion | Absorbs water, adds bulk without dissolving |
| Effect on Stool | Softens stool, eases passage | Increases stool bulk, speeds transit |
| Key Health Benefits | Helps control blood sugar, lowers LDL cholesterol | Reduces risk of constipation, supports regularity |
For hemorrhoid relief, you want a mix: the gel from soluble fiber softens, while the bulk from insoluble fiber cuts down on the need to strain.
Top Natural Sources of Fiber
Below are the foods that bring the most bang for your buck. Each entry includes a short microdata definition so search engines can understand the topic better.
- Whole grains cereals that retain the bran, germ, and endosperm, such as brown rice, quinoa, and whole‑wheat bread - 3‑5g of fiber per cooked cup.
- Fruits fresh or dried produce like apples, pears, berries, and prunes, especially when the skin is eaten - 2‑4g per medium piece.
- Vegetables non‑starchy varieties such as broccoli, carrots, and leafy greens - 2‑3g per cup cooked.
- Legumes beans, lentils, chickpeas, and peas, packed with both soluble and insoluble fiber - 6‑9g per half‑cup cooked.
- Water intake the fluid that works with fiber to keep stool soft; aim for at least 1.5‑2L per day.
Because fiber expands when it meets water, drinking enough fluid is as important as eating fiber‑rich foods.
How Much Fiber Do You Need?
Guidelines vary by age and sex, but the general target for adults is:
- Women: 25g per day
- Men: 30‑35g per day
If you’re just starting, add 5‑10g a week and monitor how your gut reacts. A simple way to track intake is to keep a food diary for a week and sum the fiber content listed on nutrition labels.
Practical Steps to Build a Fiber‑Friendly Routine
- Start the day with a fiber boost. Choose oatmeal topped with berries and a sprinkle of flaxseed instead of a sugary cereal.
- Swap refined grains for whole‑grain alternatives. Replace white bread with whole‑grain pita or brown rice with quinoa.
- Add a vegetable side to every meal. Roast broccoli, toss a salad, or blend spinach into a smoothie.
- Snack on legumes. Hummus with carrot sticks or a handful of roasted chickpeas keep you full and fiber‑rich.
- Stay hydrated. Sip water throughout the day; a glass with each meal helps the fiber work its magic.
- Consider a gentle supplement. If whole foods aren’t enough, a psyllium husk powder (soluble fiber) mixed into water can add 5g without extra calories.
Remember, sudden large doses of fiber can cause gas and cramping. Increase slowly and give your body time to adjust.

Common Pitfalls and How to Avoid Them
- Too much fiber, too little water. The fiber will just sit in the colon, making constipation worse. Pair every fiber boost with at least 250ml of water.
- Relying on processed “high‑fiber” snacks. Many contain added sugars or unhealthy fats that counteract the benefits. Stick to natural sources.
- Skipping regular bowel habits. Even with fiber, ignoring the urge can lead to harder stools later. Respond to natural signals promptly.
- Over‑supplementing. Excessive psyllium can cause blockage if not taken with enough fluid. Follow label instructions carefully.
When to Seek Professional Help
If bleeding persists after two weeks of a high‑fiber diet, or if you notice a lump that doesn’t shrink, schedule a visit with a gastroenterologist. Some hemorrhoids require medical procedures, but most cases improve dramatically with dietary changes.
Frequently Asked Questions
How quickly can I expect relief after increasing fiber?
Most people notice softer stools within 2‑3 days, but visible reduction in hemorrhoid swelling often takes 1‑2 weeks of consistent fiber intake and proper hydration.
Can I get enough fiber on a low‑carb diet?
Yes-focus on low‑carb, high‑fiber foods like leafy greens, avocado, nuts, seeds, and fiber supplements such as psyllium or inulin.
Is it safe to use fiber supplements while taking medication?
Generally, yes, but take the supplement at least two hours apart from medicines like anticoagulants or certain antibiotics, as fiber can affect absorption.
What if I experience gas after adding more fiber?
Gas is a typical adjustment sign. Reduce the portion size, increase slowly, and include a probiotic‑rich food like yogurt to help balance gut bacteria.
Do I need to track fiber if I eat a balanced diet?
If you’re regularly consuming whole grains, fruits, vegetables, and legumes, you’re likely meeting the recommendation. A quick weekly check can confirm you stay within the 25‑35g range.





Mike Creighton
14 October, 2025 15:53 PMIn the quiet chambers of our gut, fiber stands as the steadfast sentinel, warding off the insidious siege of hemorrhoids.
When we honor the ancient covenant of whole grains, legumes, and crisp vegetables, we grant our colon the smooth passage it craves.
Like a river carving stone, gradual increase in fiber softens stool, diminishing the straining that fuels inflammation.
Thus, the humble apple or a handful of flax becomes a heroic ally in the battle for comfort.
Remember, patience is the true companion of progress.
Desiree Young
18 October, 2025 03:13 AMBoost fiber fast and stop the pain.
Vivek Koul
21 October, 2025 14:33 PMIt is well documented that dietary fiber increases stool bulk and reduces transit time. This effect minimizes anal pressure and consequently lowers the risk of hemorrhoidal development. Moreover, soluble fiber modulates gut microbiota which can further alleviate inflammation.
Frank Reed
25 October, 2025 01:53 AMHey folks, just wanted to say that adding a bowl of oatmeal or some beans to your breakfast can really help keep things smooth down there. I’ve tried it myself and felt way less pressure when I hit the bathroom. Keep it up and don’t forget to drink water!
Bailee Swenson
28 October, 2025 12:13 PMFiber is the cure you’ve been ignoring 😂🚀. Start loading up on veggies and watch those hemorrhoids disappear.
tony ferreres
31 October, 2025 23:33 PMThe journey from ignorance to awareness is paved with humble kernels of oat and lentil 🌱. Let the fiber be your compass toward a painless tomorrow.
Kaustubh Panat
4 November, 2025 10:53 AMOne must contemplate the metaphysical significance of cellulose in the sustenance of our corporeal vessel. The aristocratic selection of artisanal whole‑grain breads bestows both elegance and therapeutic benefit. Therefore, the discerning palate should never forsake fiber.
Arjun Premnath
7 November, 2025 22:13 PMIncluding a colorful salad at lunch not only brightens your plate but also fortifies your digestive tract. Consistent fiber intake gently guides stool through the colon, reducing strain. Embrace this simple habit for lasting relief.
Johnny X-Ray
11 November, 2025 09:33 AMLet the crunch of fresh carrots echo the triumph of a life unburdened by pain 😎.
Every bite is a step toward liberation.
tabatha rohn
14 November, 2025 20:53 PMStop making excuses and start eating fiber already 😠.
Your comfort is in your hands.
Mark Rohde
18 November, 2025 08:13 AMFiber? Just another fad marketed to the masses.
Yet the data shows a clear reduction in anal pressure when intake hits 30g.
Ignore the hype and trust the numbers.
Rajan Desai
21 November, 2025 19:33 PMWhat specific fiber sources provide the highest soluble content?
Legumes and oats rank among the top.
S O'Donnell
25 November, 2025 06:53 AMIt is an incontrovertible truth that the modern diet, replete with processed carbohydrates and deficient in adequate dietary fibre, stands as a principal contributor to the prevalence of haemorrhoidal disease. A conscientious increment of fibre consumption, commencing at a modest five grams per week and progressing judiciously, can effectuate a palpable amelioration in stool consistency. The mechanistic basis for this improvement lies in the osmotic activity of soluble fibre, which retains water within the intestinal lumen, thereby softening the faecal mass. Concurrently, insoluble fibre augments bulk, stimulating peristaltic activity and diminishing the duration of colonic transit. Empirical investigations have demonstrated that individuals who achieve a daily intake of approximately thirty grams of total fibre experience a statistically significant reduction in haemorrhoidal symptoms. Moreover, the incorporation of diverse fibre sources, encompassing legumes, whole grains, fruits, and vegetables, ensures a balanced profile of soluble and insoluble constituents. It is advisable to accompany increased fibre intake with adequate hydration, as the hydrophilic nature of fibre necessitates sufficient aqueous availability to function optimally. In the absence of appropriate fluid consumption, the opposite effect-constipation and exacerbated straining-may ensue, nullifying the intended benefit. Clinicians frequently recommend a gradual escalation of fibre rather than an abrupt surge, precisely to mitigate gastrointestinal discomfort such as bloating and flatulence. Patients are also counseled to monitor their response to specific foods, as individual tolerances to particular fibre types can vary considerably. In certain instances, the utilisation of fibre supplements, for example psyllium husk, may be warranted to achieve target intake levels when dietary sources fall short. Nonetheless, whole‑food sources remain the gold standard, offering additional phytonutrients and a lower risk of adverse reactions. It must be underscored that fibre alone is not a panacea; rectal hygiene practices, avoidance of prolonged sitting, and regular physical activity constitute integral components of haemorrhoid management. Patients are encouraged to adopt a holistic approach, wherein dietary modification operates synergistically with lifestyle adjustments to optimise outcomes. Ultimately, the steadfast commitment to a fibre‑rich regimen, coupled with conscientious self‑care, can substantially diminish the incidence and severity of haemorrhoidal episodes.
Sangeeta Birdi
28 November, 2025 18:13 PMGreat summary! 😊 Remember to sip water throughout the day to let that fibre work its magic.
Chelsea Caterer
2 December, 2025 05:33 AMFiber heals the body, mind follows.
Helen Crowe
5 December, 2025 16:53 PMIntegrating soluble β‑glucan from oats synergizes with the mucosal barrier, enhancing sphincter resilience. Leverage this nutraceutical edge to preempt venous engorgement. Stay pumped, stay regular!
Adam Dicker
9 December, 2025 04:13 AMRise up, load that salad, and crush the pain once and for all!
Victory belongs to the fiber‑fed.
Molly Beardall
12 December, 2025 15:33 PMThe elite know that only premium whole‑grain breads can truly defeat hemorrhoids.
Commoners settle for less, and suffer.
Elijah Mbachu
16 December, 2025 02:53 AMJust start small, maybe a banana or some beans, and keep drinking water.
U wont regret it.