When a doctor prescribes a generic medication, they expect it to work just like the brand-name version. But越来越多的临床医生开始怀疑:这些便宜药,真的安全吗?
Why clinicians are asking hard questions
It’s not about distrust in generics themselves. Generic drugs have saved the U.S. healthcare system over $300 billion in the last decade. But when a patient on a generic blood thinner starts having unexplained bruising, or someone on a generic antidepressant suddenly feels worse after a refill-clinicians notice. And they’re starting to connect the dots.
A 2023 study from Ohio State University looked at over 1.2 million adverse event reports in the FDA’s database. The results were startling: generic drugs made in India had a 54% higher rate of severe side effects-including hospitalizations, disability, and death-than identical generics made in the U.S. This wasn’t random. The difference showed up most clearly in older, low-cost drugs where profit margins are razor-thin.
“As drugs get cheaper and cheaper and the competition gets more intense to hold down costs,” said lead researcher Dr. Robert S. Gray, “you start to see operations and supply chain issues that can compromise drug quality.”
How a pill gets made-and where things go wrong
Think of a generic pill like a car built from parts shipped from five different countries. The active ingredient might come from a factory in Hyderabad. The filler powder from a plant in Shanghai. The coating from a facility in Poland. The packaging from a warehouse in Mexico. Only one company’s name appears on the box. The rest? Invisible.
The FDA requires generics to prove they’re “bioequivalent”-meaning they deliver the same amount of active ingredient at the same speed as the brand version. But that’s just the starting point. What happens during manufacturing? How stable is the compound over time? Are the machines calibrated? Are workers trained? Are quality checks done hourly-or just before an inspection?
Here’s the catch: the FDA can show up unannounced at U.S. plants. But for overseas facilities? They schedule inspections months in advance. That gives manufacturers time to clean up, fix broken equipment, or even hide records. One former FDA inspector told me, “It’s like showing up to a restaurant only after they’ve scrubbed the kitchen and hired new staff.”
Older generics are the weakest link
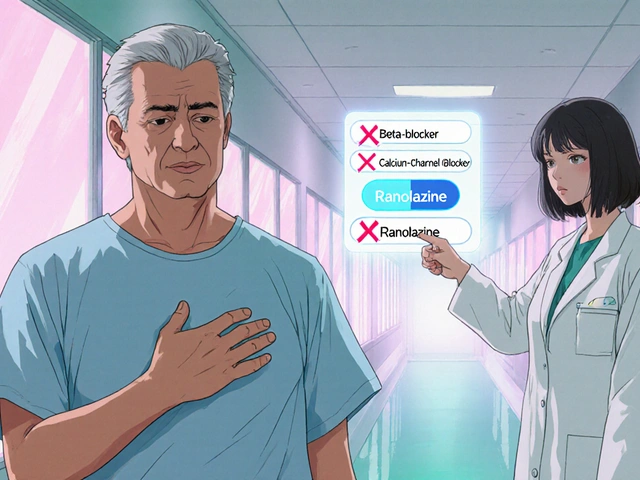
Not all generics are created equal. The biggest problems show up in older drugs-things like metformin, lisinopril, or warfarin. These are cheap, widely used, and have been on the market for decades. No one’s making big profits off them anymore. So manufacturers cut corners.
Duke-Margolis Center researchers found that outdated equipment, poor quality control, and lack of skilled labor are the top reasons for drug shortages-and almost all of them involve older generics made overseas. A single faulty batch can shut down production for weeks. Patients miss doses. Cancer treatments get delayed. Blood pressure meds run out.
And it’s not just about effectiveness. Some studies have found inconsistent dissolution rates-meaning the drug doesn’t break down the same way in the body. One pharmacist in Atlanta told me about a patient who switched from a U.S.-made generic levothyroxine to an Indian-made version and suddenly developed heart palpitations. Her TSH levels jumped 40%. She went back to the U.S. version-and her numbers stabilized within two weeks.

The FDA says it’s all fine. But is it?
The FDA insists the U.S. drug supply is among the safest in the world. They point to their 1,300+ inspectors and strict approval standards. They say bioequivalence equals safety. But that’s like saying two cars with the same engine will perform the same-ignoring the quality of the brakes, the tires, or the wiring.
What the FDA doesn’t track publicly is where each drug is made. You can’t look up a pill’s origin like you can a smartphone. A 2023 study found that only 14% of active pharmaceutical ingredients (APIs) come from U.S. labs. Over half are made in India and China. And those countries don’t always follow the same standards.
Some experts argue the FDA’s current model is outdated. “We’re still using 1980s thinking for a 2020s supply chain,” said a pharmacist in Minneapolis who works in hospital procurement. “If we want safety, we need transparency. Patients and providers deserve to know where their meds come from.”
What’s being done-and what’s not
There’s a quiet revolution happening in drug manufacturing: advanced manufacturing technologies (AMTs). These include continuous production lines, real-time sensors, and AI-driven quality control. These systems catch problems before a batch leaves the plant. And here’s the kicker: over 80% of drugs made with AMTs are produced in the U.S.
So why aren’t more companies switching? Cost. Upgrading a factory costs millions. For a generic drug that sells for $3 a month, that’s not a smart investment. But for companies making high-volume, low-margin drugs, the risk of recalls, lawsuits, or patient harm is even higher.
Some hospitals are starting to push back. A few health systems now require suppliers to disclose the country of origin for high-risk generics. One oncology center in Chicago stopped using a particular generic version of a chemotherapy drug after three patients had severe reactions. They switched back to the brand-and the reactions stopped.
Is there a solution?
There’s no single fix. But the best path forward combines three things: transparency, domestic production, and smarter regulation.
First, make manufacturing location public. Let prescribers and patients see where a drug is made-not just the brand name on the bottle. That alone would create market pressure. If two identical generics are on the shelf, but one says “Made in USA” and the other says “Made in India,” people will choose the safer option.
Second, bring more manufacturing home. The University of Wisconsin School of Pharmacy says it clearly: “If we have more generic manufacturing happening domestically, we would ideally have fewer quality concerns, fewer shortages, and a more resilient supply chain.”
Third, change how the FDA inspects. No more advance notice for overseas plants. Random, unannounced checks. Like they do here. And if a facility fails? Ban its products-not just for a few months, but permanently.
It’s not about rejecting generics. It’s about demanding better. We don’t accept shoddy brakes on a car. Why accept them in medicine?”
What clinicians can do today
You don’t need to wait for policy changes to protect your patients. Here’s what you can do right now:
- Ask pharmacists where the generic was made. Many can tell you the manufacturer or country of origin.
- Track reactions. If a patient has a new side effect after switching generics, consider the source.
- Choose U.S.-made generics when available-especially for narrow-therapeutic-index drugs like warfarin, levothyroxine, or seizure meds.
- Report adverse events to the FDA’s MedWatch program. One report might seem small. A hundred? That’s a pattern.
- Advocate for transparency at your hospital or clinic. Push for procurement policies that prioritize quality over lowest price.
Generic drugs aren’t the enemy. Poor manufacturing practices are. And clinicians are the last line of defense.
Are generic drugs less effective than brand-name drugs?
No, not inherently. Generic drugs are required by law to have the same active ingredient, strength, and dosage form as the brand version. They must also prove bioequivalence-meaning they work the same way in the body. But effectiveness can be compromised if the manufacturing process is flawed. Poor quality control, outdated equipment, or inconsistent ingredients can lead to variations in how the drug is absorbed or how stable it is over time. This is why some patients report different side effects or reduced effectiveness after switching to a different generic batch.
Why are most generic drugs made overseas?
It’s about cost. Labor, land, and regulatory compliance are significantly cheaper in countries like India and China. After patents expire, generic manufacturers compete fiercely on price. To stay profitable, many companies outsource production to low-cost facilities-even if it means sacrificing quality control. The U.S. has seen a dramatic decline in domestic API production, falling from over 50% in the 1990s to just 14% today. Globalization made sense financially, but it created a fragile supply chain.
Does the FDA inspect foreign drug factories?
Yes-but not the same way they inspect U.S. factories. For domestic plants, FDA inspections are unannounced. For foreign facilities, inspections are scheduled months in advance. This gives manufacturers time to clean up, fix issues, or hide problems. Experts argue this creates a loophole. A 2023 study found that overseas facilities are more likely to have serious violations than U.S. ones, and the gap is growing. The FDA admits it lacks the resources to inspect every facility annually, especially overseas.
Can I tell if my generic drug is made in the U.S.?
Not easily. Drug labels don’t show where the medicine was manufactured. You might see the name of the distributor or brand, but not the actual factory location. Some pharmacies can tell you the manufacturer if you ask. Online databases like Drugs.com sometimes list the maker, but not always the country. The best way to know is to contact your pharmacist directly and ask: “Where was this generic made?” If they don’t know, it’s a red flag.
Should I avoid generic drugs altogether?
No. Generic drugs are safe and effective for most people. Millions rely on them every day. But you should be informed. For high-risk medications-like blood thinners, thyroid drugs, epilepsy meds, or chemotherapy-consider asking for the U.S.-made version if it’s available. Don’t assume all generics are equal. If you notice a change in how you feel after switching generics, talk to your doctor. Your body might be telling you something the label won’t.





Iona Jane
17 January, 2026 03:26 AMThis is why I don't trust anything anymore
Jami Reynolds
19 January, 2026 02:34 AMThe FDA is complicit. They've been bought off by Big Pharma and foreign manufacturers. The entire regulatory framework is a charade. Unannounced inspections? Ha. They schedule them during monsoon season in Hyderabad so the plant can 'temporarily' shut down. The data is manipulated. The reports are buried. This isn't negligence-it's systemic corruption.
And don't tell me about bioequivalence. That's a mathematical fiction. Two drugs can have the same active ingredient concentration and still behave differently in vivo due to excipients, crystalline structure, or coating degradation. The FDA doesn't test for that. They don't want to. It's cheaper to ignore it.
Remember the 2018 valsartan recall? Contaminated with NDMA? That was from a Chinese plant. The FDA knew for months. They waited until the drug was in 20 million prescriptions before acting. Why? Because the cost of recalling it would've broken insurers. Patients don't matter. Profits do.
And now they want us to believe that 'U.S.-made' is the solution? Please. Even American plants outsource their APIs. The 'Made in USA' label is a marketing lie. It's like buying a Tesla and thinking the battery was made in Texas.
The only real solution is nationalizing pharmaceutical manufacturing. Take the industry out of private hands. Put it under public oversight. Fund it like the military. Because right now, your life is being auctioned off to the lowest bidder.
Diane Hendriks
19 January, 2026 13:20 PMLet’s be clear: this isn’t about generics. It’s about sovereignty. We outsourced the very foundation of public health to nations with no accountability, no transparency, and no moral compass. We traded our security for a few dollars on a prescription. That’s not capitalism-it’s national suicide.
The U.S. used to produce 50% of its active pharmaceutical ingredients. Now it’s 14%. Where did the rest go? To countries where labor is cheap, regulations are a suggestion, and inspectors are paid in chai and bribes.
And yet we still let pharmacists swap pills without disclosure. No informed consent. No labeling. No right to know. This violates the most basic tenets of medical ethics. If you wouldn’t eat food made in a factory with no health code inspections, why take medicine from one?
It’s time to stop pretending this is a healthcare issue. It’s a national security crisis. Our soldiers, our veterans, our children-they’re being dosed with unverified, untraceable chemicals. And the FDA? They’re the janitors cleaning up after the arsonists.
Sohan Jindal
19 January, 2026 23:11 PMThey're selling poison and calling it medicine. I don't care if it's cheap. I don't care if it's 'bioequivalent.' If I take a pill and my body starts acting weird, it's not me-it's the junk they put in it. And the government lets it happen because they're scared of the cost. Well guess what? The cost is people dying. And that's not a number. That's my mom. That's my neighbor. That's my kid.
Why don't we just make the stuff here? We have the tech. We have the brains. We have the land. We're just lazy. And greedy. And we let China and India run our medicine like it's some cheap Walmart brand.
Stop the outsourcing. Make it here. Pay the workers. Pay the inspectors. Pay the price. Because your life isn't a spreadsheet.
Frank Geurts
21 January, 2026 04:33 AMAs a global health professional with over two decades of field experience across five continents, I must emphasize the profound structural imbalances inherent in the current pharmaceutical supply chain. The commodification of life-saving therapeutics has led to a tragic erosion of quality assurance protocols, particularly in jurisdictions with under-resourced regulatory oversight.
It is imperative that we reframe this discourse not as a nationalist outcry, but as a universal human rights imperative: the right to safe, traceable, and efficacious medication. The FDA’s inspectional disparities-while legally defensible-are ethically indefensible. A patient in rural Ohio deserves the same assurance of drug integrity as a patient in Boston or Berlin.
Moreover, the adoption of advanced manufacturing technologies, while cost-prohibitive for low-margin generics, must be incentivized through public-private partnerships, not left to market forces. The cost of inaction-measured in preventable hospitalizations, iatrogenic harm, and lost productivity-far exceeds the capital investment required.
Transparency is not a burden; it is a covenant between provider and patient. We must demand, as a matter of civil dignity, that every pill bear not only its chemical name, but its origin story.
Mike Berrange
22 January, 2026 04:14 AMEveryone’s freaking out about Indian generics, but have you checked the label on your ‘American-made’ metformin? The active ingredient was probably synthesized in Gujarat. The capsule shell? Made in Shanghai. The tablet press? Bought from a German company but assembled in Mexico. The ‘Made in USA’ sticker is just a sticker. It’s all globalized. We’re not fixing anything by pretending we can go back to 1995.
The real issue? We’ve turned medicine into a commodity. We want it cheap, fast, and invisible. Then we act shocked when it breaks. It’s not the country of origin-it’s the mindset. We treat pills like toilet paper. And we wonder why the quality’s trash.
Ayush Pareek
23 January, 2026 07:07 AMI understand the fear, but let’s not forget: India produces over 60% of the world’s generic drugs. Millions of people in Africa, Latin America, and even the U.S. depend on these medicines. Yes, there are bad actors-but there are also world-class facilities in Hyderabad and Pune that follow GMP standards better than some U.S. plants.
The solution isn’t to shut down Indian manufacturing. It’s to raise the bar for everyone. Invest in training, support regulatory modernization, and create global inspection standards. We can’t isolate ourselves. We need cooperation, not fear.
And honestly? If you’re worried about your levothyroxine, ask your pharmacist for the manufacturer. Many Indian companies like Sun Pharma and Dr. Reddy’s have stellar reputations. Not all generics are the same. Judge the maker, not the country.
Nat Young
24 January, 2026 19:41 PMOh wow, a 54% higher rate of side effects? That’s wild. But let’s not forget-correlation isn’t causation. Maybe the patients taking Indian generics are sicker to begin with. Maybe they’re non-compliant. Maybe they’re on ten other meds. Maybe the FDA database is full of junk reports from people who think aspirin is a conspiracy.
And who says U.S.-made is better? Ever heard of the 2012 fungal meningitis outbreak? That was from a U.S. compounding pharmacy. People died. And no one was screaming about ‘Made in America’ then.
Stop scapegoating. This isn’t about geography. It’s about lazy medicine. If you’re not tracking your patient’s response to a generic switch, that’s your failure-not the manufacturer’s.
Niki Van den Bossche
25 January, 2026 06:10 AMOh darling, we’ve become a nation of pharmacological peasants, bowing at the altar of cost-efficiency while our bodies become collateral in a global supply chain ballet choreographed by Wall Street and the FDA’s half-baked 1980s playbook. The pill you swallow isn’t medicine-it’s a metaphor for late-stage capitalism: identical in appearance, wildly different in soul.
The U.S.-made version? A gilded cage. The Indian one? A prison with no bars. Both are cages. The only difference is the color of the walls.
And yet, we pretend that ‘transparency’ is the answer. As if slapping a ‘Made in India’ sticker on the bottle will magically make your levothyroxine less likely to turn your heart into a drum solo. Please. The real tragedy? We’ve normalized this. We’ve been trained to accept pharmaceutical roulette as just another Tuesday.
What we need isn’t a label. We need a revolution. A cultural reckoning. A collective refusal to treat our bodies like disposable widgets in a global assembly line.
Jaspreet Kaur Chana
25 January, 2026 16:31 PMHey everyone, I work in pharma logistics in India, and I can tell you this: yes, some factories cut corners-but most don’t. We have over 3,000 FDA-approved plants here. Many of them are ISO-certified, automated, and inspected more than U.S. plants. The problem isn’t India. The problem is that we’re judged by the worst, not the best.
Also, you know what’s cheaper than making drugs here? Making them in the U.S. with union labor, OSHA compliance, and EPA rules. That’s why companies leave. Not because they’re evil. Because the math doesn’t work.
Instead of blaming us, help us improve. Fund training programs. Send U.S. inspectors to mentor our teams. Invest in tech transfer. We’re not the enemy-we’re the backbone of global access to medicine. Millions of people in poor countries wouldn’t survive without us.
And if you want to know where your pill came from? Ask your pharmacist. We’re not hiding. We’re just tired of being painted as villains while the real problem-profit-driven healthcare-isn’t even on the table.
Haley Graves
27 January, 2026 15:48 PMIf your doctor prescribes a generic, and you’re worried, ask for the manufacturer name. Most pharmacists can tell you. If they can’t, that’s a red flag. Don’t accept ‘I don’t know.’ Push back. Your life isn’t a gamble.
And if you’re on warfarin, levothyroxine, or seizure meds? Stick with the same brand or manufacturer. Don’t let the pharmacy swap it without telling you. If they do, complain. Write to your state board of pharmacy. This isn’t about being paranoid. It’s about being informed.
And yes-U.S.-made generics are often better. Not because they’re magic. Because the oversight is tighter. So if you can get it, take it. Don’t wait for policy. Advocate for yourself.
ellen adamina
28 January, 2026 23:02 PMI switched to a different generic lisinopril last month and my blood pressure spiked. I went back to the old one and it stabilized. I didn’t say anything until now. I thought it was stress. Turns out, it was the pill. I wish I’d known the manufacturer. I wish I’d asked. I wish someone had told me this could happen.
Just sharing. If you’ve had something similar, you’re not alone.
Gloria Montero Puertas
29 January, 2026 19:27 PMLet’s be honest: you’re not worried about quality. You’re worried about class. You want your medicine to be ‘American’ because you believe that means ‘better.’ That’s not science. That’s nationalism dressed up as healthcare.
And your ‘U.S.-made’ generics? Half of them are still made with APIs from China. You’re not fixing the system. You’re just buying a placebo label.
Stop pretending you’re protecting patients. You’re just comforting your ego.
Tom Doan
30 January, 2026 01:47 AMSo the FDA inspects U.S. plants unannounced... and foreign ones with advance notice. Fascinating. So if I showed up at your house unannounced, you’d panic. But if I gave you a week’s notice? You’d clean up, hide the receipts, and serve tea.
That’s not regulation. That’s theater. And we’re all just audience members, clapping politely while our meds get weaker.
Ayush Pareek
31 January, 2026 23:37 PMTom, you nailed it. That’s exactly how it works. I’ve seen it firsthand. The night before an inspection, they bring in new machines, hire temporary workers, and scrub the floors until they shine. The next day? Back to business as usual.
But here’s the thing-this isn’t unique to India. It happens everywhere. The system is broken. We need random, global inspections. No advance notice. Ever. And if a plant fails? They’re blacklisted for life.