Ever heard two medicines with nearly the same name confused in a busy pharmacy aisle? Metoprolol tartrate and metoprolol succinate are the poster children for that mix-up. One's fast-acting, the other a slow burner — just the type of detail that separates a dose-saving success from a disaster. But confusion isn't what threatens patients most. It's not knowing which metoprolol version fits your story or when a different beta-blocker outshines them both.
What Sets Metoprolol Tartrate and Succinate Apart?
Let’s slice through the mystery right away: tartrate and succinate are both forms of metoprolol, a beta blocker trusted for decades to manage high blood pressure, fast heartbeats, and certain heart conditions. But they don’t work exactly the same.
Metoprolol tartrate gets in quick. Swallow a tablet, and within an hour or two, your blood levels hit the peak. Doctors prescribe it for immediate needs. Chest pain flares, racing hearts that need corralling rapidly — that’s tartrate territory. The catch? It fades fast, so you’ll need to take it once or even twice daily to keep up.
Now, metoprolol succinate plays the long game. It’s made for a slow drip release over 24 hours, meaning just one pill a day keeps your heart protected round the clock. This makes it a favorite for chronic issues: ongoing hypertension, long-term heart failure care, and stable angina. Patients love that forget-me-not dosing.
The United States Food and Drug Administration (FDA) underscores this – both forms treat high blood pressure, but only succinate wins the nod for heart failure. It’s not semantics; it’s about how the body absorbs and processes each version.
Take a look at this comparison:
| Drug Form | Release Type | Indications | Typical Dosing |
|---|---|---|---|
| Metoprolol Tartrate | Immediate Release | Hypertension, angina, arrhythmias, acute MI | 1-2 times per day |
| Metoprolol Succinate | Extended Release | Hypertension, angina, heart failure | Once daily |
Imagine how these options play out in real life: A young athlete with sudden, scary palpitations might do well on a rapid punch of tartrate. A retiree battling steady but stubborn high blood pressure? The one-a-day succinate simplifies their pillbox.
Why Release Profiles Matter for Daily Life
Ever tried to get a teenager to remember the same thing twice a day? Now imagine organizing that kind of schedule for someone juggling dozens of pills. Sometimes it’s impossible — and this is where release profiles become more than technical jargon. They’re real, practical solutions.
Immediate-release (IR) meds like metoprolol tartrate pop into your blood, peak fast, and disappear just as quickly. That's great when you need a sharp fix, but the need to take them multiple times a day can test your memory and patience.
Extended-release (ER) meds like metoprolol succinate ease in slowly, delivering medicine all day and slashing forgetting risk. Some studies show up to 30% better adherence with once-daily drugs compared to those that demand rounds morning and night. No surprise: if you only pop one pill at breakfast, you’re likely to stick with your therapy longer.
Sound simple? Not always. Some patients feel better control with the peaks-and-valleys of an IR med, while others crave the flat line an ER tablet brings. Busy parents, shift workers, and anyone who travels a lot almost always prefer extended release — it’s just one less thing to stress about. But those dealing with sudden chest pain after a bad meal want the fast action, hands down.
Another real-world wrinkle: the cost. Tartrate is older and usually cheaper, showing up constantly on generics lists, while some insurances cover more extended-release forms for chronic heart conditions. Check with your local pharmacy before locking in a choice based just on convenience.
- If you take other meds that might interact, a once-daily regimen makes it easier to spot culprits if side effects strike.
- If you’ve got a lifestyle full of unpredictable meals, work outs, or even fasting, talk to your doctor about timing — especially IR drugs.
- For anyone with trouble swallowing, both forms come in tablets that you should not chew or crush, but succinate sometimes allows for more flexible dosing and combinations.
Patient Scenarios: When to Choose Tartrate, Succinate, or An Alternative?
Doctors don’t toss metoprolol into a pill organizer by flipping a coin. They weigh patient stories, health risks, and yes, a few overlooked lifestyle quirks. Let’s dig into how that looks in practice.
Meet Sipho, a taxi driver in bustling Durban who needs to control his blood pressure and manage stress-induced palpitations. He works odd hours, grabbing food on the go. Succinate could fit his 5 a.m. to dusty dusk shifts — pop it at sunrise and get on the road. Tartrate would mean carrying a second dose in his pocket, risking a missed or late pill as customers pile in and out.
Now, say there’s Lesedi, a young woman with migraines who’s had a few “heart racing” moments during exams. Tartrate’s short action could help her when needed, without binding her to daily pills or risking dropping her already low blood pressure if used long term.
Then there’s Mr. Ngubane, a retiree with heart failure. His cardiologist won’t budge from succinate — steady blood levels mean fewer hospital visits, less risk of spiraling symptoms, and less “yo-yo” with his blood pressure. In real-world trials, people with chronic heart failure on extended-release beta blockers feel better, land in fewer emergency rooms, and just plain live longer.
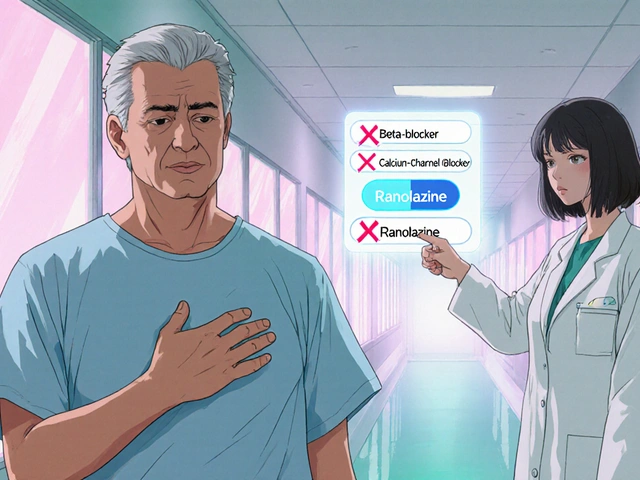
But metoprolol isn’t the only player in the beta-blocker game. For some, especially those with severe asthma or side effects from metoprolol, the best move is actually to look at a metoprolol alternative. Drugs like carvedilol (more suited for heart failure), bisoprolol (often easier on the lungs), or even non-beta-blocker agents such as calcium channel blockers can suit some patient stories better. Switching isn’t always easy — these meds work differently, and the potential for side effects shifts accordingly.
Treatment choices should always account for side effects: metoprolol (tartrate or succinate) can cause tiredness, cold extremities, and sometimes vivid dreams. People with diabetes need to watch out — beta blockers can mask low blood sugar symptoms, upping risk unless you’re extra vigilant. If those become burdensome or dangerous, don’t tough it out: alternatives and dosing tweaks exist for a reason.
- Make sure your doctor knows about your work schedule, lifestyle, and other meds — these tiny details matter.
- When changing from IR to ER (or the reverse), never guess the dose. Extended-release pills aren’t milligram-for-milligram identical and can cause problems if swapped without supervision.
- If you notice sleep changes or rapid fatigue after starting, don’t wait for your next appointment — touch base earlier.
Advice and Tips for the Beta-Blocker Journey
If you’re sorting out metoprolol options for your heart or blood pressure, don’t just shrug and take whatever lands in your pillbox. There’s much more at stake than splitting hairs.
Start with the basics: organize your doses with a smartphone reminder or a pillbox, especially if you’re on tartrate. Missed doses are one of the top reasons for loss of blood pressure control and emergency room visits. Extended-release options remove some of that risk, but if you tend to forget even once-a-days, tie your dose to a daily ritual you never skip (like brushing teeth).
Keep an eye on your body’s clues. If you feel dizzy, lightheaded, or notice shortness of breath, don’t wait it out. These could signal either a too-high dose or an interaction with another med. Grabbing your home blood pressure monitor and writing down readings a few times a week can make a massive difference when you talk to your pharmacist or doctor.
Don’t double up a missed dose, whether you’re on tartrate or succinate; take the next one as scheduled. Skipping a dose or two happens to almost everyone. What's key is not letting it become a routine.
Finally, don’t tackle medication switches solo — especially if you’re shifting to a metoprolol alternative. The chemistry here isn't basic math. There are major differences in how long these drugs act, how your body processes them, and what side effects you might run into.
- Always check your pharmacy’s instructions before splitting or crushing a tablet — most ER versions should be swallowed whole.
- Keep an up-to-date list of all your medications (including vitamins and supplements) in your wallet; emergencies move too fast to hunt down pill bottles.
- If you’re scheduled for surgery or a big dental procedure, tell your care team you’re on a beta blocker — stopping abruptly can trigger dangerous heart rhythms.
Small details — like whether you’re a coffee addict, work odd hours, or deal with depression — can shape which drug helps more and hurts less. Metoprolol tartrate, metoprolol succinate, and their alternatives aren't just chemical names on a label; they're tools that need to fit the way you live. Judging which to use is more art than science, and no one knows your rhythms better than you.






Luke Webster
23 July, 2025 21:05 PMI used to mix these two up all the time till I had a friend almost get dosed wrong at CVS. Now I always check the label twice - tartrate for when you need it fast, succinate for when you want to forget about it till tomorrow. Simple as that.
Also, if you’re on succinate and your doc says ‘once daily,’ don’t be that guy who takes it at midnight because you ‘forgot’ - morning’s better for consistency. Your heart will thank you.
Natalie Sofer
24 July, 2025 04:41 AMmy doctor switched me from tartrate to succinate last year and i swear my life got easier. no more 2x a day reminders, no more panic when i miss a dose. i still get tired sometimes but honestly? better than feeling like my heart’s gonna explode.
ps: i typoed this whole thing but you get the point 😅
Tiffany Fox
24 July, 2025 09:19 AMOne pill a day = life changed. Seriously. I’m a single mom with three kids and a dog that eats meds. Succinate saved me.
Rohini Paul
26 July, 2025 00:09 AMin india most people just take whatever the pharmacist gives them. i saw a guy get tartrate for heart failure once - he didn’t even know the difference. no wonder hospital admissions are so high here.
also, why do docs still prescribe tartrate for hypertension? it’s outdated. succinate is better for long-term. period.
ps: cost matters but not as much as your life. don’t cheap out on your heart.
Courtney Mintenko
26 July, 2025 02:23 AMeveryone’s so obsessed with ‘release profiles’ like it’s some deep philosophy but it’s just chemistry
you’re not special your heart doesn’t need a TED Talk
just take the pill and stop overthinking it
Sean Goss
26 July, 2025 16:52 PMLet’s be clear: the pharmacokinetic disparity between metoprolol tartrate (immediate-release, t½ ~3–7h) and succinate (extended-release, t½ ~12–24h via osmotic delivery) is clinically non-trivial. The FDA’s indication divergence isn’t arbitrary - it’s rooted in CHF mortality data from MERIT-HF and COPERNICUS trials.
Also, the notion that ‘one pill a day improves adherence’ is a neoliberal myth propagated by Big Pharma marketing departments. Real-world adherence is dictated by socioeconomic factors, not dosing frequency.
And for god’s sake, stop using ‘heart failure’ and ‘hypertension’ interchangeably. They’re not the same disease process.
Khamaile Shakeer
26 July, 2025 17:18 PMWait… so you’re telling me the ‘succinate’ one is for old folks and the ‘tartrate’ is for people who panic during Zoom calls?? 😅
Also, why does everyone act like this is new info? I learned this in high school bio. 🤦♂️
PS: my uncle took tartrate for heart failure and ended up in ICU. Don’t be him.
Suryakant Godale
26 July, 2025 23:49 PMWhile the pharmacological distinctions between metoprolol tartrate and metoprolol succinate are well-documented in peer-reviewed literature, the practical implications for patient outcomes are often underemphasized in primary care settings.
It is imperative that clinicians recognize that extended-release formulations are not merely convenient alternatives, but rather therapeutically superior in chronic conditions such as systolic heart failure, as evidenced by the 34% reduction in all-cause mortality observed in the MERIT-HF trial.
Furthermore, the assumption that immediate-release formulations offer superior symptom control during acute episodes must be weighed against the increased risk of non-adherence, which correlates directly with higher rates of hospitalization.
As a medical professional with over two decades of clinical experience, I urge all stakeholders - patients, pharmacists, and prescribers alike - to prioritize evidence-based selection over convenience or cost. The stakes are not theoretical; they are existential.