When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But how do manufacturers prove that? In the past, they’d copy the formula, run a few tests at the end of production, and hope it passed. Today, that’s no longer enough. Quality by Design (QbD) has become the standard for developing generic drugs - not as a bonus, but as a requirement. It’s not about testing quality into a product after it’s made. It’s about building it in from day one.
What Exactly Is Quality by Design?
Quality by Design, or QbD, is defined by the International Council for Harmonisation (ICH) as a systematic approach that starts with clear goals and uses science and risk management to understand how a drug is made. It’s not a new idea - it’s been around since 2005 - but it’s only in the last decade that regulators like the U.S. Food and Drug Administration (FDA) made it mandatory for all new generic drug applications.
Before QbD, manufacturers followed a recipe: mix for 15 minutes, compress at 12 kN, dry at 45°C. If the final product failed a test, they’d throw it out and try again. No one really knew why it failed. QbD flips that. Instead of fixed numbers, you define ranges - and prove, through science, that the product stays safe and effective within those ranges. This is called the design space. If you stay inside it, you don’t need to ask regulators for permission every time you tweak a process.
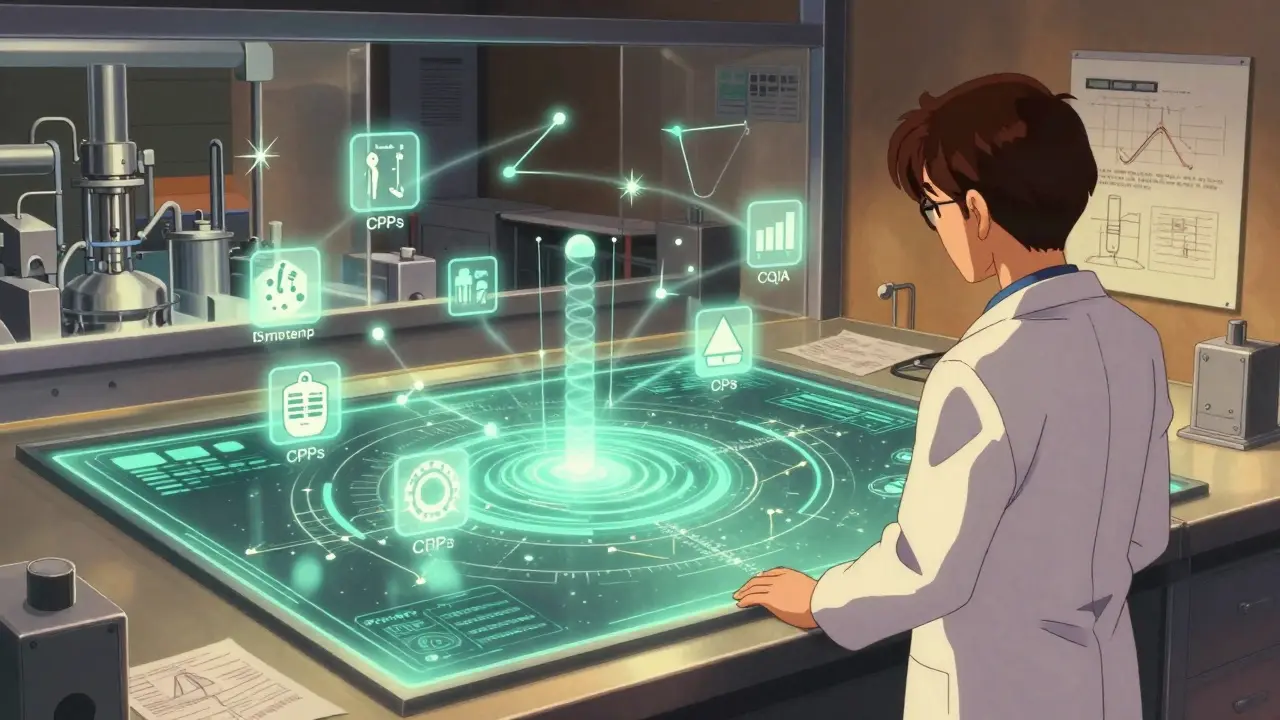
The Five Pillars of QbD in Generic Drugs
QbD isn’t a single step. It’s a chain of five connected elements, each building on the last.
- Quality Target Product Profile (QTPP) - This is your starting point. What should the drug do? How fast should it dissolve? What impurities are allowed? For generics, the FDA requires at least 95% similarity to the brand-name drug in key performance measures, especially dissolution. If your tablet doesn’t release the drug like the original, it won’t work the same way in the body.
- Critical Quality Attributes (CQAs) - These are the measurable traits that directly affect safety or effectiveness. For most generic tablets, that’s dissolution rate (f2 similarity factor >50), content uniformity (RSD ≤6.0%), and impurity levels (following ICH Q3B limits). You can’t test your way out of poor CQAs - you have to design them in.
- Critical Process Parameters (CPPs) - These are the manufacturing variables that impact CQAs. A granulation moisture level of 1.5-3.0%, compression force between 10-15 kN, or drying temperature at 40-50°C aren’t arbitrary. They’re the result of Design of Experiments (DoE) studies that map cause and effect. Too much moisture? The tablet crumbles. Too little? It won’t bind properly.
- Design Space - This is where QbD shines. Instead of one set point, you define a multidimensional range of CPPs that consistently produce quality. The FDA accepts design spaces built on data from over 100 simulated batches. Once approved, you can adjust parameters within this space without submitting a new application. That’s flexibility. That’s efficiency.
- Control Strategy - How do you make sure you stay in the design space? That’s where Process Analytical Technology (PAT) comes in. Tools like near-infrared spectroscopy let you monitor moisture, blend uniformity, or tablet hardness in real time - not after the fact. Companies using PAT reduce end-product testing by 35-60%, according to the Parenteral Drug Association.
Why QbD Beats the Old Way
Traditional development is like driving with your eyes closed - you only know if you’re on the road when you crash. QbD is like having GPS and sensors telling you exactly where you are at all times.
Since the FDA made QbD mandatory in 2017, approval rates for generic applications have jumped 23%. Review times dropped by nearly five months per application. Why? Because regulators aren’t guessing anymore. They see the science. They see the risk analysis. They see the data proving the product will work consistently.
Companies using QbD also get fewer Complete Response Letters (CRLs) - the dreaded “we need more info” notices from regulators. QbD-based submissions see 31% fewer CRLs than traditional ones. That means faster market access and less wasted time.
And it saves money. One manufacturer reported saving $1.2-2.8 million per product annually by avoiding costly regulatory submissions for minor process changes. When a supply chain disruption hits - say, during a pandemic - companies with approved design spaces can switch suppliers or adjust parameters without halting production. One company kept 99.8% on-time delivery for simvastatin during the worst of the pandemic - all because their QbD control strategy allowed 11 adjustments without prior approval.
The Catch: Cost, Complexity, and Over-Engineering
QbD isn’t free. It’s not even cheap.
Initial development costs rise by 25-40%. Timelines stretch by 4-8 months. You need scientists trained in risk management (ICH Q9) and design of experiments. You need $500,000+ in analytical equipment. You need software like MODDE Pro - $15,000 per user per year.
And here’s the real danger: over-engineering. Some companies apply full QbD to simple immediate-release tablets - products with decades of proven performance. One case study showed a firm spending $450,000 on DoE studies for a drug where the design space was already well known. That’s like using a rocket ship to deliver groceries.
Experts warn that QbD must be proportionate. For ultra-low-cost generics - products with annual sales under $50 million - the cost of QbD can eat up more than 15% of lifetime revenue. That’s not sustainable. The Generic Pharmaceutical Association advises a risk-based approach: go deep on complex products (inhalers, patches, modified-release tablets), and keep it lean on simple ones.
Real-World Successes and Failures
At Hikma Pharmaceuticals, implementing QbD for their generic esomeprazole cut post-approval deviations from 14 per year to just 2. That saved $850,000 annually in quality investigations.
At Teva, a QbD-based continuous manufacturing design space for levothyroxine improved batch consistency by 28%. That’s huge for a drug where even tiny variations can affect thyroid levels.
But it’s not all smooth sailing. The European Medicines Agency found that 63% of QbD failures in generics come from poor understanding of how formulation affects performance - especially in modified-release products. Some companies can’t establish a meaningful link between in vitro dissolution and what happens in the body (in vivo). Without that, you’re just collecting data, not building knowledge.
Indian manufacturers, facing tighter budgets, have adopted QbD at 68% rates - lower than the 89% seen in the U.S. and EU. But the top 10 Indian generics firms spent $227 million on QbD capabilities in 2022. They know: if you want to sell globally, you need to play by the global rules.
The Future: QbD, Continuous Manufacturing, and AI
QbD isn’t standing still. It’s merging with other modern tools.
The FDA’s Emerging Technology Program has approved 27 QbD-based continuous manufacturing applications - all with 100% success. Continuous manufacturing means drugs are made in a steady flow, not in batches. It’s faster, more consistent, and easier to control with real-time sensors - perfect for QbD.
New guidelines like ICH Q14 (Analytical Procedure Development) require more robust method validation, but they also speed up approval for QbD-aligned submissions. By 2027, McKinsey predicts 95% of new generic approvals will include QbD.
And AI? It’s coming. Machine learning can predict how changes in particle size or binder concentration will affect dissolution - cutting down the number of experiments needed. The tools are here. The data is there. The next wave of QbD won’t just be science - it’ll be smart science.

Who Needs QbD - And Who Doesn’t?
QbD is essential for:
- Complex generics: inhalers, transdermal patches, injectables, modified-release tablets
- Products targeting global markets (FDA, EMA, PMDA)
- Companies planning long-term supply chain resilience
QbD may be overkill for:
- Simple immediate-release tablets with well-established profiles
- Ultra-low-cost generics where development costs can’t exceed 15% of projected revenue
- Products with no clinical variability risk
The key is not whether you use QbD - it’s how you use it. Tailor it. Don’t force it.
Getting Started With QbD
If you’re developing a generic drug today, here’s your roadmap:
- Start with the Reference Listed Drug (RLD). Characterize it deeply - dissolution, particle size, polymorph form. Use published data to cut development time by 30%.
- Define your QTPP. Match the RLD’s performance as closely as possible.
- Identify your CQAs. Focus on what matters: dissolution, uniformity, impurities.
- Use DoE to find your CPPs. Don’t guess. Test.
- Build your design space. Prove it with 100+ simulated batches.
- Implement PAT. Real-time monitoring reduces waste and speeds approval.
- Use risk-based bracketing for multi-strength products. One set of studies can cover 3-5 doses.
The FDA offers free QbD training modules. The Parenteral Drug Association has certified practitioner courses with 85% pass rates. You don’t need to figure this out alone.
Final Thought: It’s Not Just Compliance - It’s Competitive Advantage
QbD isn’t just about passing a regulator’s checklist. It’s about building a better product, faster, with fewer surprises. It turns generic drug development from a guessing game into a science. Companies that embrace it don’t just survive - they lead. They get faster approvals. Lower costs. Stronger supply chains. And trust from regulators and patients alike.
The question isn’t whether you should use QbD. It’s how deeply you’ll go - and whether you’ll use it to catch up… or to pull ahead.
Is QbD mandatory for all generic drugs?
Yes, for all new Abbreviated New Drug Applications (ANDAs) submitted to the FDA after October 1, 2017. The European Medicines Agency and Japan’s PMDA also require QbD for complex generics. While not every simple generic needs a full QbD package, regulators expect a science-based justification for any development approach.
How does QbD improve bioequivalence?
QbD doesn’t replace bioequivalence studies - it strengthens them. By ensuring the in vitro dissolution profile matches the brand-name drug (f2 >50), QbD provides a reliable predictor of in vivo performance. This reduces the need for costly clinical trials. For complex products like extended-release tablets, where bioequivalence is hard to prove clinically, QbD’s scientific control over release mechanisms is often the only viable path to approval.
What’s the biggest mistake companies make with QbD?
Applying full QbD to simple products where it’s unnecessary. Spending $400,000 on DoE studies for a basic immediate-release tablet with a well-known formulation is wasteful. The best QbD strategies are tailored - deep for complex products, lean for simple ones. Regulators appreciate proportionality.
Can small generic manufacturers afford QbD?
Yes, but strategically. Start with one product. Use free FDA training. Partner with contract labs for PAT testing. Use risk-based bracketing to cover multiple strengths with one set of studies. Many small firms succeed by focusing on niche complex generics where QbD gives them a competitive edge - not by trying to compete on price alone.
How long does QbD development take compared to traditional methods?
QbD adds 4-8 months to development for simple products, and 6-12 months for complex ones. But the trade-off is faster regulatory approval - 9.2 months on average vs. 13.9 months for non-QbD applications. Plus, you avoid costly delays later from process changes or regulatory requests.
Does QbD guarantee product quality?
No guarantee - but it dramatically reduces risk. QbD doesn’t eliminate variability; it understands and controls it. By defining design spaces and using real-time monitoring, you catch problems before they reach the patient. It’s not perfection - it’s predictability.
What role does PAT play in QbD?
PAT is the eyes and ears of QbD. Near-infrared spectroscopy, Raman imaging, and other real-time tools let you monitor critical parameters during manufacturing - moisture, blend uniformity, tablet hardness - without stopping the line. This reduces end-product testing by 35-60% and ensures every batch meets specs. Without PAT, QbD becomes just paperwork.
How is QbD changing global generic markets?
It’s raising the bar. The WHO now includes QbD in its prequalification program. India and China are investing heavily to meet global standards. Companies without QbD can’t compete for high-value markets like the U.S. and EU. It’s turning generic drugs from low-cost commodities into scientifically validated medicines - and the companies that adapt are the ones winning contracts.




Blow Job
25 December, 2025 01:54 AMFinally, someone gets it. QbD isn’t just bureaucracy-it’s what keeps your grandma’s blood pressure med from turning into a placebo. I’ve seen too many batches fail because someone thought 'close enough' was good enough. Not anymore.
Christine Détraz
25 December, 2025 13:11 PMI used to think this was all overkill until my dad’s thyroid med started acting up. Turns out, tiny changes in dissolution can wreck your whole day. QbD doesn’t just make drugs safer-it makes them predictable. And that’s worth every penny.
Ajay Sangani
27 December, 2025 03:17 AMyou know… i think this whole qbd thing is like trying to build a perfect sandcastle with a bulldozer. sure it looks nice on paper, but for a simple pill that’s been around since the 90s? why do we need 100 simulations? sometimes the old way just… works.
Pankaj Chaudhary IPS
27 December, 2025 17:27 PMIndia is not behind-we are adapting strategically. While some Western firms waste millions on over-engineered QbD for simple tablets, Indian manufacturers are focusing on high-complexity generics where it matters. We are not cutting corners-we are cutting waste. This is smart globalization.
Aurora Daisy
28 December, 2025 05:59 AMOh great, so now we’re treating aspirin like a SpaceX rocket. Next they’ll require quantum entanglement testing for ibuprofen. The FDA’s obsession with ‘science’ is just a fancy way of charging companies $2M to make a pill they’ve been making since 1987.
Paula Villete
28 December, 2025 23:37 PMokay but like… if you’re spending $450k on doe for a basic immediate release tablet… are you sure you’re not just doing this for your resume? i mean, i get it, you wanna look smart… but your shareholders are crying in the corner.
Georgia Brach
29 December, 2025 20:50 PMThe 23% increase in approval rates is misleading. It’s not that QbD improves quality-it’s that regulators are now drowning in submissions that at least look like they followed the checklist. Real innovation? Still buried under compliance paperwork.
Katie Taylor
30 December, 2025 11:17 AMStop treating patients like lab rats. If your generic doesn’t work like the brand, you’re not a manufacturer-you’re a criminal. QbD isn’t optional. It’s the bare minimum. Anyone who resists it should be banned from making medicine.
Isaac Bonillo Alcaina
31 December, 2025 22:40 PMYou’re all missing the real issue. Big Pharma pushed QbD to lock out small players. Now only corporations with $500k+ in PAT equipment can compete. This isn’t science-it’s a monopoly play disguised as regulation.
suhani mathur
1 January, 2026 13:38 PMPat is the unsung hero here. I’ve seen labs waste weeks testing final batches-only to find out the whole run was off because a humidity sensor failed at hour 3. With PAT? You catch it at minute 10. No drama. No recalls. Just clean data.
Diana Alime
3 January, 2026 04:46 AMso like… i just read this whole thing and my brain is like… why are we even doing this? i just want my cholesterol pill to not kill me. why do i need a 12-page risk assessment for a 5mg tablet? i’m tired.
Chris Buchanan
3 January, 2026 06:35 AMHere’s the truth: QbD isn’t about making pills-it’s about making regulators sleep at night. And honestly? I’m fine with that. If it means fewer recalls, fewer lawsuits, and fewer people getting sick because someone ‘eyeballed’ a compression setting… then yeah, let’s over-engineer the hell out of it.
John Pearce CP
4 January, 2026 17:25 PMRegulatory harmonization is not a favor-it is a geopolitical imperative. Nations that fail to adopt QbD at scale will become pharmaceutical backwaters. The U.S. and EU are not merely setting standards-they are defining the future of global health infrastructure. Resistance is not just imprudent; it is negligent.
Payson Mattes
4 January, 2026 21:39 PMWait… so if they can monitor moisture in real time… does that mean the government can track your pills? Like… are they watching your blood pressure meds right now? I read somewhere the FDA has a backdoor in every PAT system. I’m not paranoid-I’m informed.