Quick Takeaways
- Ranolazine is the only approved oral sodium‑channel blocker for chronic angina.
- It improves exercise tolerance without changing heart rate or blood pressure.
- Guidelines place it after first‑line agents like beta‑blockers and calcium‑channel blockers.
- Common side effects are dizziness, nausea and constipation; monitor QT interval.
- Ideal candidates are patients with refractory angina despite optimal conventional therapy.
When chest pain keeps coming back despite nitrates, beta‑blockers, and calcium‑channel blockers, doctors call it refractory angina. It’s a frustrating gray zone: the heart muscle isn’t getting enough blood, yet the usual meds have hit their limit. Enter Ranolazine, a drug that works a completely different way. This article walks through how it helps, what the evidence says, and how clinicians integrate it into everyday practice.
How Ranolazine Works - A Different Mechanism
Most anti‑anginal drugs lower heart rate or blood pressure, reducing myocardial oxygen demand. Ranolazine skips that route. It blocks the late inward sodium current (late I_Na) in cardiac cells. By curbing excess sodium entry, it prevents calcium overload inside the cells, which in turn reduces diastolic tension and improves coronary blood flow. The net effect is less ischemia without affecting heart rate or systemic blood pressure - a unique advantage for patients who can’t tolerate further drops in either.
Key Clinical Trials - What the Data Shows
Two landmark phase III studies, the ERICA and MERLIN‑TIMI 36 trials, provide the bulk of evidence. In ERICA, patients with chronic angina were randomized to Ranolazine 500‑1000 mg twice daily or placebo on top of standard therapy. After 12 weeks, the ranolazine group walked 45 meters farther on a treadmill (p < 0.001) and reported a 38 % reduction in weekly angina episodes.
MERLIN‑TIMI 36 enrolled over 6,500 patients with non‑ST‑elevation acute coronary syndrome. While the primary endpoint (cardiovascular death, MI, or stroke) didn’t differ, a prespecified subgroup analysis of those with persistent angina showed a 25 % reduction in angina frequency when treated with Ranolazine. These data cement its role as an add‑on therapy specifically for symptom relief.
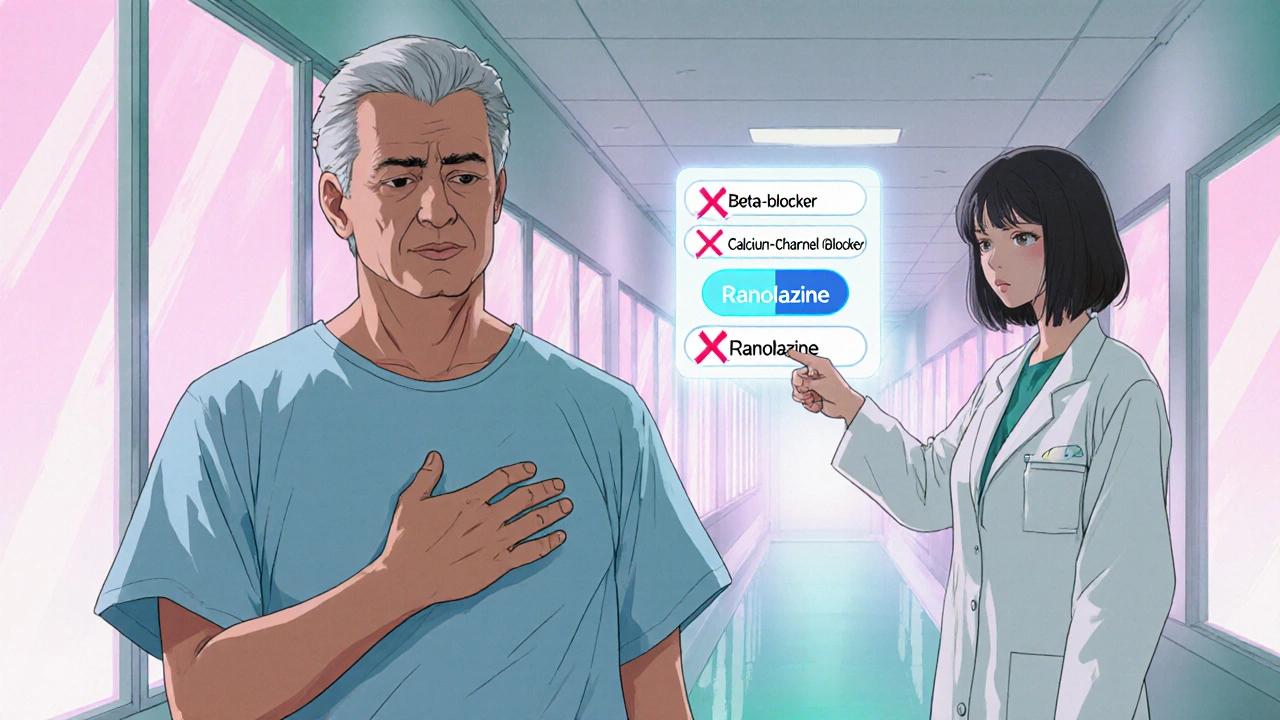
Guideline Position - When to Use Ranolazine
International societies have converged on a similar recommendation:
- NICE guidelines (UK, 2023) list ranolazine as a third‑line oral agent after beta‑blockers and calcium‑channel blockers for chronic stable angina.
- The American College of Cardiology (ACC) and American Heart Association (AHA) 2022 update give it a Class IIb recommendation - useful when symptoms persist despite optimal first‑ and second‑line therapy.
In practice, this translates to a step‑wise approach: start with lifestyle change, then nitrates, beta‑blockers, or calcium‑channel blockers. If angina remains uncontrolled, add Ranolazine before moving to more invasive options like revascularization.
Practical Prescribing - Dose, Titration, and Monitoring
Initial dosing starts at 500 mg twice daily with food. After one week, if tolerated, it can be increased to 1000 mg twice daily - the dose most studies used. A few patients benefit from the higher 1500 mg twice‑daily regimen, but the risk of QT prolongation rises.
Key safety checks:
- Baseline ECG to assess QT interval; avoid if QTc > 450 ms.
- Repeat ECG 1‑2 weeks after dose escalation.
- Watch for drug interactions: strong CYP3A4 inhibitors (e.g., ketoconazole) can double ranolazine levels; dose adjustment or avoidance is required.
- Renal or hepatic impairment may necessitate lower dosing - 500 mg twice daily is standard for eGFR < 30 mL/min.
Side‑Effect Profile - What Patients Usually Experience
Overall, Ranolazine is well‑tolerated. The most common adverse events (≥5 % in trials) are:
- Dizziness
- Nausea
- Constipation
- Headache
These usually fade within two weeks. Persistent dizziness or syncope warrants ECG review for QT prolongation. In rare cases, severe arrhythmias have been reported, especially when combined with other QT‑prolonging drugs.
How Ranolazine Stacks Up Against Other Anti‑Anginals
| Drug | Mechanism | Typical Dose | Main Side Effects | Guideline Rank |
|---|---|---|---|---|
| Ranolazine | Late Na⁺ current blocker | 500‑1000 mg BID | Dizziness, nausea, constipation, QT‑prolongation | Third‑line (Class IIb) |
| Beta‑blocker | β‑adrenergic blockade | Metoprolol 25‑200 mg daily | Bradycardia, fatigue, bronchospasm | First‑line (Class I) |
| Calcium‑channel blocker | L‑type Ca²⁺ channel inhibition | amlodipine 2.5‑10 mg dailyPeripheral edema, flushing, constipation | First‑line (Class I) | |
| Nitroglycerin | Vasodilation via NO release | Sublingual 0.3‑0.6 mg PRN | Headache, hypotension, tolerance | Adjunct (Class IIa) |
Choosing the Right Patient - Who Benefits Most?
Ideal candidates share three traits:
- Documented chronic stable angina on optimal doses of a β‑blocker and a calcium‑channel blocker (or other combination).
- Persistent symptoms that limit daily activities (e.g., walking > 200 m triggers chest pain).
- No contraindications: QTc < 450 ms, no severe hepatic dysfunction, and no concomitant strong CYP3A4 inhibitors.
In patients with diabetes, Ranolazine may also improve glycemic control modestly, a bonus noted in the MERLIN‑TIMI 36 subgroup.
Monitoring and Follow‑Up
After starting therapy:
- Schedule a clinic visit or telehealth check at 2 weeks to assess symptom relief and side effects.
- Repeat ECG at 1‑month to ensure QTc remains < 500 ms.
- If nausea persists, split the total daily dose into three administrations (e.g., 500 mg TID) to improve tolerance.
- Re‑evaluate the need for nitroglycerin patches; many patients can discontinue them after achieving stable control with ranolazine.
Frequently Asked Questions
Can Ranolazine be used in patients with heart failure?
Yes, trials have included patients with NYHA class II‑III heart failure. It does not worsen systolic function and may improve exercise capacity, but the QT interval still needs monitoring.
What happens if I miss a dose?
Take the missed dose as soon as you remember, unless it’s less than 6 hours before the next scheduled dose. In that case, skip the missed one and resume the regular schedule to avoid double‑dosing.
Is Ranolazine safe during pregnancy?
Animal studies show no teratogenic effect, but human data are limited. It’s classified as FDA Pregnancy Category C, so it should only be used if the potential benefit justifies the risk.
How long does it take to feel better?
Most patients notice reduced angina frequency within 2‑4 weeks of reaching the target dose. Full improvement in exercise tolerance may take up to 8 weeks.
Can I take Ranolazine with other QT‑prolonging drugs?
Co‑administration is discouraged. If unavoidable, strict ECG monitoring and possibly a reduced ranolazine dose are required.
In summary, Ranolazine fills a niche for patients whose angina won’t settle with traditional drugs. Its unique mechanism, solid trial data, and clear guideline position make it a valuable tool in the cardiologist’s arsenal-provided you watch the QT interval and respect drug‑interaction warnings.




Rachel Zack
26 October, 2025 11:10 AMIt's unethic to push ranolazine without proper risk discusion. Patients deserve clear info before adding another med.
Lori Brown
27 October, 2025 15:10 PMGreat summary! Ranolazine indeed fills that gap when β‑blockers and CCBs aren't enough 😊. Thanks for breaking it down so clearly!
Jacqui Bryant
28 October, 2025 19:14 PMRanolazine can help when other meds fail.
Paul Luxford
29 October, 2025 23:20 PMI appreciate the balanced view on dosing and QT monitoring; it’s essential to keep an eye on cardiac safety.
Nic Floyd
31 October, 2025 03:32 AMFrom a pharmacodynamic perspective ranolazine attenuates the late I_Na current reducing intracellular Ca2+ overload thereby improving myocardial perfusion while sparing heart rate and systemic blood pressure effects 🚀 the drug’s efficacy is evident in ERICA & MERLIN‑TIMI 36 especially for refractory angina patients with preserved ejection fraction and without significant QTc prolongation considerations should include baseline ECG & review of concomitant CYP3A4 inhibitors for drug‑drug interactions
Johnae Council
1 November, 2025 07:49 AMHonestly this stuff feels like a marketing gimmick – add another pill, more side effects, and the same old “talk to your doc” disclaimer. Not convinced it’s worth the hype.
Manoj Kumar
2 November, 2025 12:09 PMAh, the eternal quest for relief – we chase the elusive “perfect” drug while the universe chuckles at our hubris. Ranolazine may be a small piece of the puzzle, but don’t expect it to solve the cosmic tragedy of chest pain.
Hershel Lilly
3 November, 2025 16:32 PMBuilding on the pharmacology, the reduced diastolic tension also translates to better subendocardial perfusion during stress which can be objectively measured with myocardial perfusion imaging.
Carla Smalls
4 November, 2025 20:59 PMStay positive! Even if you experience mild nausea, it usually fades and the improvement in walking distance can be a game‑changer for daily activities.
Monika Pardon
6 November, 2025 01:29 AMOne might wonder whether the pharmaceutical giants have a hidden agenda, subtly nudging clinicians toward Ranolazine while downplaying alternative lifestyle strategies. Nonetheless, the data remains solid, albeit presented with a polished veneer.
Rhea Lesandra
7 November, 2025 06:02 AMRanolazine represents a valuable addition to the anti‑anginal arsenal, especially for patients whose symptoms persist despite optimal first‑line therapy. Its unique mechanism of late sodium current inhibition distinguishes it from traditional agents that primarily lower heart rate or blood pressure. By mitigating intracellular calcium overload, the drug improves myocardial relaxation and enhances subendocardial perfusion during diastole. Clinical trials such as ERICA demonstrated a meaningful increase in exercise tolerance, with participants walking an average of 45 meters farther on a treadmill. Moreover, the MERLIN‑TIMI 36 subgroup analysis revealed a 25 % reduction in weekly angina episodes, underscoring its symptomatic benefit. Importantly, the medication does not exacerbate bradycardia or hypotension, making it suitable for patients who cannot tolerate further hemodynamic shifts. Dosing starts conservatively at 500 mg twice daily, with a titration to 1000 mg BID once tolerability is confirmed, and occasional escalation to 1500 mg BID in refractory cases. Safety monitoring should include a baseline ECG to assess QTc, followed by repeat ECG after dose adjustments, given the potential for QT prolongation. Drug interactions warrant caution, particularly with strong CYP3A4 inhibitors, which can double plasma concentrations of Ranolazine. Renal and hepatic impairment also dictate dose reductions to avoid accumulation. Common adverse effects such as dizziness, nausea, and constipation are generally mild and transient, often resolving within two weeks. Patient education on recognizing persistent dizziness or syncope is crucial to prompt ECG review for possible arrhythmias. In practice, Ranolazine is positioned as a third‑line oral agent per NICE and ACC/AHA guidelines, filling the therapeutic gap before considering invasive revascularization. While it is not a disease‑modifying therapy, its role in enhancing quality of life is undeniable. Clinicians should assess individual patient profiles, including comorbidities and concomitant medications, to tailor therapy appropriately. Ultimately, when used judiciously, Ranolazine can transform the daily experience of those living with refractory angina.
Kasey Marshall
8 November, 2025 10:39 AMOverall the benefits outweigh the risks if monitored properly.
Dave Sykes
9 November, 2025 15:19 PMKeep pushing forward with Ranolazine when standard meds fall short – it’s a solid option that can really make a difference for patients.