When your stomach hurts, you’re tired all the time, and you’re rushing to the bathroom multiple times a day, it’s easy to blame food or stress. But if these symptoms stick around for weeks or months, it might be something deeper - something like inflammatory bowel disease, or IBD. Two main conditions fall under this umbrella: Crohn’s disease and ulcerative colitis. They sound similar, share symptoms, and are often confused. But they’re not the same. And knowing the difference can change everything - from how you’re diagnosed to how you live your life.
Where the Inflammation Happens
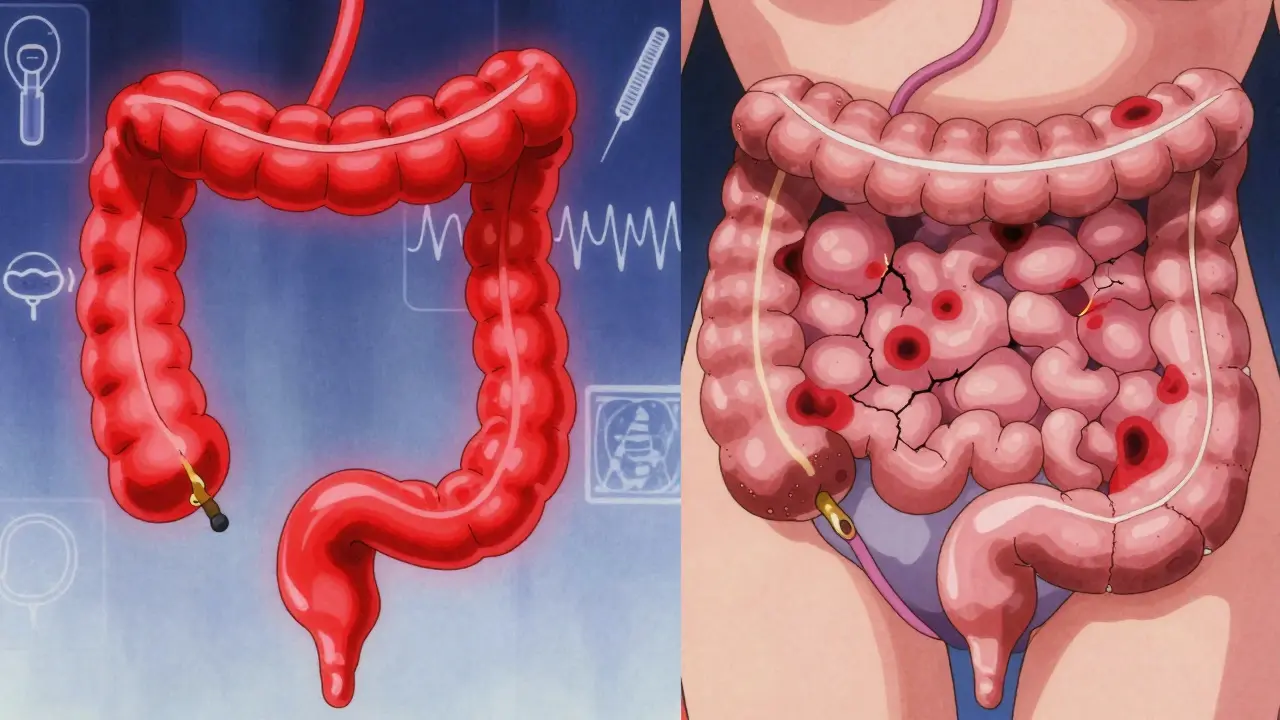
Ulcerative colitis sticks to one place: your colon and rectum. It starts at the very end, in the rectum, and moves upward in a continuous line. If you have UC, your entire colon might be inflamed, or just part of it - but it’s always connected, like a river flowing from one point to another. There are no gaps. No healthy patches in between. Crohn’s disease doesn’t play by those rules. It can show up anywhere - from your mouth to your anus. Most often, it hits the end of the small intestine (the terminal ileum) and the beginning of the colon. But it doesn’t care about continuity. It picks random spots, leaving patches of normal tissue between inflamed areas. These are called "skip lesions," and they’re a dead giveaway for Crohn’s. You can have inflammation in your small bowel, then a few inches later, nothing. Then another patch down near your anus. That’s Crohn’s.How Deep Does It Go?
Ulcerative colitis only digs into the innermost layer of the bowel wall - the mucosa. It’s like a sunburn on the surface. Crohn’s disease? It goes all the way through. It eats through the mucosa, the muscle layer, even the outer lining. This is called transmural inflammation. And that’s why Crohn’s causes complications that UC rarely does. When inflammation goes deep, it can scar the tissue, making the bowel narrow - that’s a stricture. It can also punch holes through the wall, creating abnormal tunnels called fistulas. These can connect your bowel to your bladder, skin, or other organs. About one in three people with Crohn’s will develop a stricture in their lifetime. One in four will get a fistula. For people with ulcerative colitis? Those numbers are under 5%.What Happens When Things Get Bad
Both conditions can flare up, making you feel awful. But the emergencies are different. In ulcerative colitis, there’s a rare but dangerous complication called toxic megacolon. Your colon swells up dangerously, like a balloon about to burst. It happens during severe flares, and it’s life-threatening. It affects about 5% of UC patients. You’ll need emergency surgery. Crohn’s disease almost never causes toxic megacolon. But because it can affect the small intestine, it can lead to malnutrition. The small bowel absorbs nutrients - vitamins, minerals, calories. If Crohn’s is eating away at that area, you might lose weight, feel weak, or develop anemia - even if you’re eating fine. About 65% of Crohn’s patients report nutritional issues, compared to just 30% of UC patients.How Doctors Tell Them Apart
There’s no single blood test that says "Crohn’s" or "UC." Diagnosis is a puzzle. Doctors use every piece they can find. A colonoscopy is the gold standard. In UC, they’ll see a smooth, continuous red patch starting at the rectum. Pseudopolyps - little bumps of healing tissue - are common. In Crohn’s, they’ll see patchy inflammation, deep ulcers, and a cobblestone look on the lining. Biopsies help too: UC shows inflammation only in the top layers. Crohn’s shows inflammation all the way through. Imaging matters. An MRI enterography can show fistulas and thickened bowel walls - classic Crohn’s signs. A capsule endoscopy (you swallow a tiny camera) can spot inflammation in the small bowel that a colonoscope can’t reach. That’s almost always Crohn’s. Blood and stool tests give clues. A high fecal calprotectin level means active inflammation - common in both. But pANCA antibodies show up in 60-70% of UC patients and only 10-15% of Crohn’s patients. It’s not perfect, but it helps.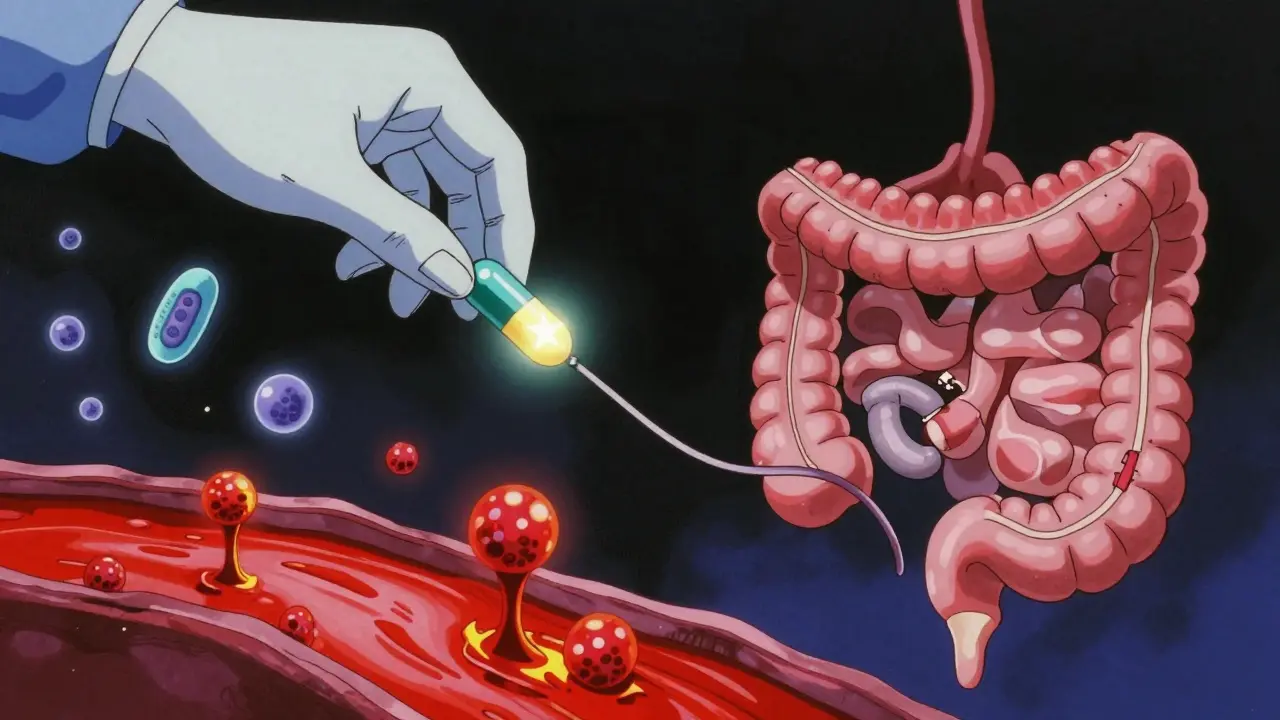
Treatment: Same Tools, Different Strategies
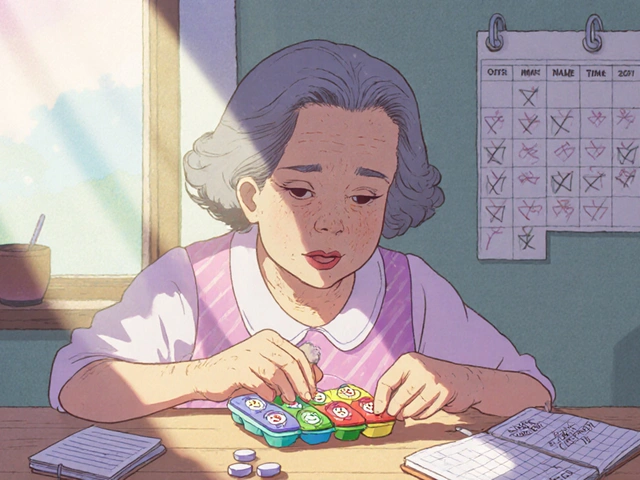
Both conditions are treated with anti-inflammatories, immunosuppressants, and biologics. But how they’re used? That’s where things split. For mild to moderate ulcerative colitis, doctors often start with 5-ASAs - drugs like mesalamine - delivered directly to the colon as enemas or suppositories. That works for 60-80% of people. It’s targeted. Minimal side effects. Crohn’s? Those local treatments don’t work well. The inflammation is too widespread. You need systemic drugs - pills or injections that work all over your body. Immunosuppressants like azathioprine can bring remission in 40-50% of Crohn’s patients within a few months. Biologics like infliximab or adalimumab help about 30-40% of Crohn’s patients stay in remission after a year. For UC, the same drugs work, but less often - around 20-30%.Surgery: Cure vs. Temporary Fix
This is the biggest difference. If you have ulcerative colitis and your symptoms are out of control, you can get your entire colon and rectum removed. That’s called a proctocolectomy. Then, your surgeon can create a pouch from your small intestine and attach it to your anus. You’ll still go to the bathroom normally. And guess what? You’re cured. No more UC. About 10-15% of UC patients end up needing this surgery within 10 years. Crohn’s disease? Surgery doesn’t cure it. You might have a section of diseased bowel removed - a resection. It helps. But the disease always comes back. In about half of patients, it returns near the surgical site within 10 years. That’s why doctors avoid surgery unless absolutely necessary.What Else Happens Outside the Gut
IBD isn’t just a gut disease. About one in three people with either condition get problems elsewhere. Joint pain? Common. Skin rashes like erythema nodosum? Happens in 10-15%. Eye inflammation? Around 5-10% of cases. But here’s a key distinction: primary sclerosing cholangitis - a liver disease that scars the bile ducts - is strongly linked to ulcerative colitis. About 3-7% of UC patients get it. Only 0.5-1% of Crohn’s patients do. If you have UC and your liver enzymes are high, your doctor will check for this.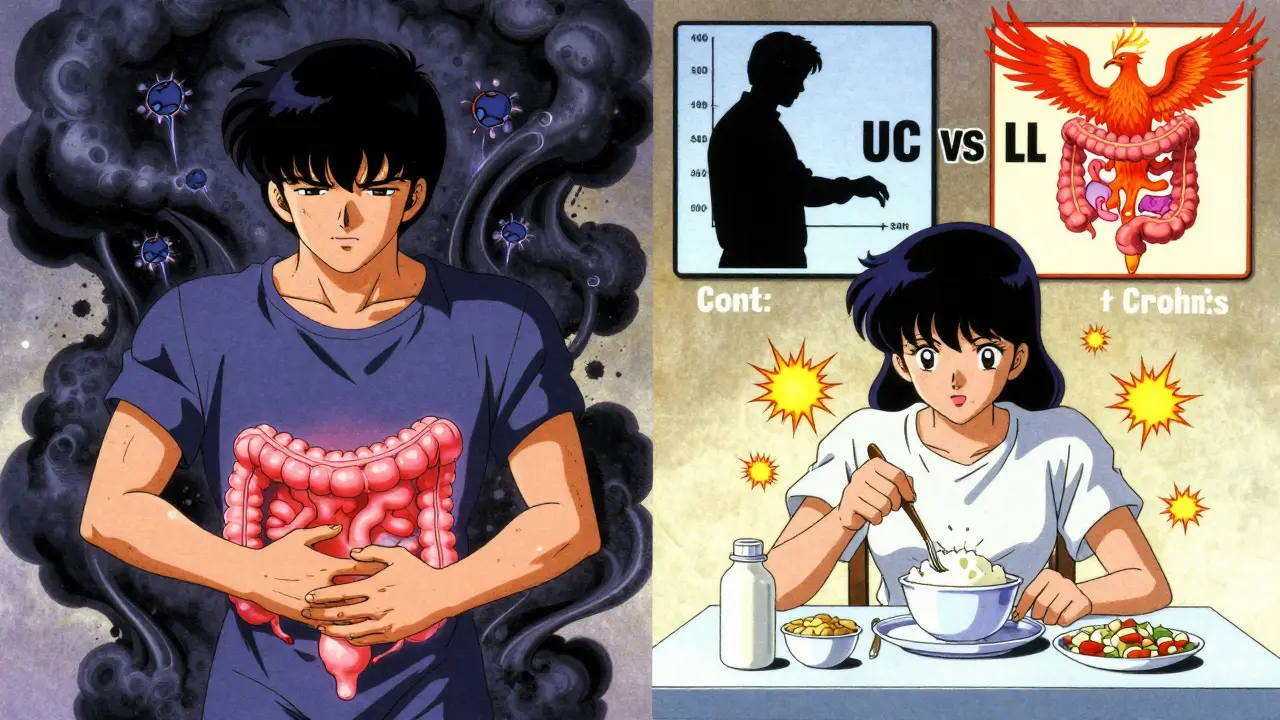
What Patients Say
Real people with these conditions talk about their daily lives. On forums and support groups, UC patients say the biggest problem is urgency - that sudden, uncontrollable need to go. About 87% report it. They also see blood in their stool more often - 75% say yes. For Crohn’s patients, it’s more about food. Dairy, high-fiber veggies, spicy meals - they trigger flares more often. About 45% blame dairy. Stress hits both groups hard. But on Reddit’s IBD community, stress is the top trigger for UC flares. For Crohn’s? It’s food.The Big Picture
About 3 million Americans have IBD - half Crohn’s, half UC. Rates are rising, especially in places like South Africa, India, and Brazil, where diets are shifting toward processed foods. The cost of care is steep. Severe Crohn’s can cost over $38,000 a year. Severe UC? Around $31,000. That’s why early, accurate diagnosis matters. There’s still a group - 10-15% - where doctors can’t tell the difference right away. They call it indeterminate colitis. These patients are monitored over time. Sometimes, new symptoms or complications appear, and the diagnosis shifts.What’s Next?
New treatments are coming. Fecal microbiota transplants - basically, giving someone healthy gut bacteria - helped 32% of UC patients go into remission in one trial. For Crohn’s? Only 22%. That tells us the gut microbiome reacts differently in each disease. Drugs like mirikizumab (for Crohn’s) and etrolizumab (for UC) are in final testing. Results could be ready by late 2024. These are targeted therapies designed specifically for each condition’s biology.Final Thoughts
Crohn’s disease and ulcerative colitis are both chronic, lifelong conditions. Neither is your fault. Neither is caused by stress alone. But they’re not the same. One is a surface-level, continuous inflammation of the colon. The other is a deep, patchy, full-thickness disease that can strike anywhere in your gut. Knowing which one you have isn’t just about labels. It’s about choosing the right treatment. Avoiding the wrong surgery. Understanding your risks. Managing your diet. Preparing for the future. If you’re living with IBD, work with a specialist who knows the difference. And if you’re unsure? Get a second opinion. Because in IBD, the details matter - more than you think.Can you have both Crohn’s disease and ulcerative colitis?
No, you cannot have both at the same time. They are two distinct conditions under the IBD umbrella. However, about 10-15% of cases are initially unclear and labeled "indeterminate colitis." Over time, as symptoms and complications develop, doctors can usually reclassify the condition as either Crohn’s or UC. In rare cases, a patient’s disease behavior changes so much that the original diagnosis is revised - but it’s still one condition or the other, never both.
Is IBD the same as IBS?
No, they’re completely different. IBD - Crohn’s and ulcerative colitis - causes actual inflammation and damage to the bowel wall. IBS (irritable bowel syndrome) is a functional disorder - meaning the gut looks normal but doesn’t work right. IBS causes bloating, cramping, and changes in bowel habits, but no bleeding, no ulcers, no weight loss. IBD can be confirmed with scans and biopsies. IBS is diagnosed by ruling out other conditions.
Can diet cure Crohn’s or ulcerative colitis?
No diet can cure either condition. But diet can help manage symptoms. Some people with Crohn’s find that avoiding dairy or high-fiber foods reduces flares. People with UC often feel better cutting out spicy or fried foods. Special diets like the low-FODMAP diet or exclusive enteral nutrition (a liquid diet) can help induce remission in some cases - especially in Crohn’s. But these are tools, not cures. Medication and medical supervision are still essential.
Does stress cause IBD?
Stress doesn’t cause Crohn’s or ulcerative colitis. These are autoimmune diseases triggered by genetics and environmental factors like diet, antibiotics, or infections. But stress can make symptoms worse and trigger flares. Many patients report flare-ups after major life events - job loss, divorce, illness. Managing stress through therapy, exercise, or mindfulness doesn’t cure IBD, but it helps you stay in remission longer.
Will I need surgery?
For ulcerative colitis, surgery is a cure - and about 10-15% of people eventually need it. For Crohn’s, surgery is not a cure. About half of people will need at least one operation in their lifetime to remove blocked or damaged sections of bowel. But because Crohn’s comes back after surgery, doctors try to delay it as long as possible. The goal is to use medications to keep the disease under control and avoid surgery unless it’s absolutely necessary.
Can IBD turn into cancer?
Long-standing ulcerative colitis increases the risk of colon cancer, especially if the entire colon is affected for more than 8-10 years. Regular colonoscopies with biopsies are recommended to catch precancerous changes early. Crohn’s disease also carries a slightly increased risk, but it’s lower than UC. The risk is higher if you have inflammation in the colon. Keeping the disease under control with medication reduces cancer risk significantly.





Michael Bond
27 December, 2025 07:58 AMThis post nailed it. I’ve had Crohn’s for 12 years and no one ever explained skip lesions like that before.
Now I get why my colonoscopy looked like someone threw darts at my intestine.
Kuldipsinh Rathod
27 December, 2025 08:21 AMBro in India we call this ‘gut drama’ and nobody takes it seriously till you collapse. I lost 20kg in 3 months and my uncle said ‘just eat less spicy food’.
Turns out I had Crohn’s. This article? Lifesaver.
SHAKTI BHARDWAJ
28 December, 2025 23:19 PMTHIS IS ALL WRONG!! I have UC and my whole small intestine is on FIRE!! My doctor said I have Crohn’s but I KNOW I have UC because I cried at a taco truck!!
Also I think the government is hiding the real cure in a secret bunker under Disney World!!
AND WHY IS NO ONE TALKING ABOUT THE ALTERNATIVE THERAPIES?? I drank lemon water with cayenne and I’m cured!!!
Matthew Ingersoll
29 December, 2025 22:58 PMThe distinction between transmural and mucosal inflammation is clinically critical. The data on fistula formation and nutritional deficiencies aligns with recent meta-analyses from the Journal of Crohn’s and Colitis.
It’s also worth noting that geographic variation in IBD incidence correlates strongly with dietary shifts toward ultra-processed foods, as referenced in the 2023 Lancet Global Health report.
carissa projo
30 December, 2025 03:59 AMThere’s something so deeply human about how this post doesn’t just list facts - it holds space for the quiet, exhausting reality of living with IBD.
You don’t just have a disease. You have a body that betrays you on Tuesdays when you’re running late for work. A gut that screams when you’re trying to hug your kid. A life that gets rearranged around bathroom locations.
And yet - you keep showing up. You keep eating. You keep laughing. You keep loving.
This isn’t just medical info. It’s a quiet anthem for everyone who’s ever whispered ‘I’m okay’ while crying in a public restroom.
You’re not broken. You’re not weak. You’re just surviving - and that’s enough.
Bryan Woods
30 December, 2025 22:07 PMAccurate and well-structured. The comparison of surgical outcomes between UC and Crohn’s is particularly useful for patients considering long-term management options.
It’s also reassuring to see the emphasis on indeterminate colitis as a legitimate diagnostic category rather than a failure of testing.
Ryan Cheng
1 January, 2026 03:18 AMOne thing this doesn’t mention enough: mental health. IBD isn’t just a gut thing - it’s a brain thing too.
Depression and anxiety aren’t side effects - they’re part of the disease cycle. When your body’s screaming, your mind starts screaming back.
Therapy isn’t optional. It’s as essential as your meds. Find someone who gets it - not just a generalist who says ‘try yoga’.
Shreyash Gupta
2 January, 2026 17:23 PMlol why are people so obsessed with labels? I have both. Or neither. Or maybe I’m just allergic to modern food.
Also I think my dog cured me with his vibes 🐶✨
Also I drank kombucha for 47 days and now I’m a unicorn 🦄
Ellie Stretshberry
4 January, 2026 15:35 PMI had UC for 8 years and got my colon removed. I didn’t think I’d ever feel normal again.
Turns out I can eat pizza now. And sleep through the night.
It’s not perfect. But it’s better.
Thank you for writing this.
Zina Constantin
6 January, 2026 13:16 PMFor anyone reading this and feeling alone - you’re not.
You’re part of a quiet army of people who show up even when their guts are falling apart.
And if you’ve ever Googled ‘can I die from this’ at 3am - you’re braver than you know.
Keep going. Your story matters. Even the messy, bloody, exhausted parts.