CNS Depressant Combination Risk Calculator
Assess your risk of dangerous interactions when combining cannabis with CNS depressants like benzodiazepines, opioids, or sleep medications. Based on medical guidelines from the American Society of Health-System Pharmacists.
Combining cannabis with other CNS depressants isn’t just a bad idea-it’s a silent danger that’s sending more people to emergency rooms every year. If you’re using marijuana for sleep, anxiety, or pain, and also take Xanax, Valium, opioids, or even sleeping pills, you’re not just doubling down on drowsiness. You’re risking your breathing, your memory, and possibly your life.
How Cannabis Acts Like a CNS Depressant
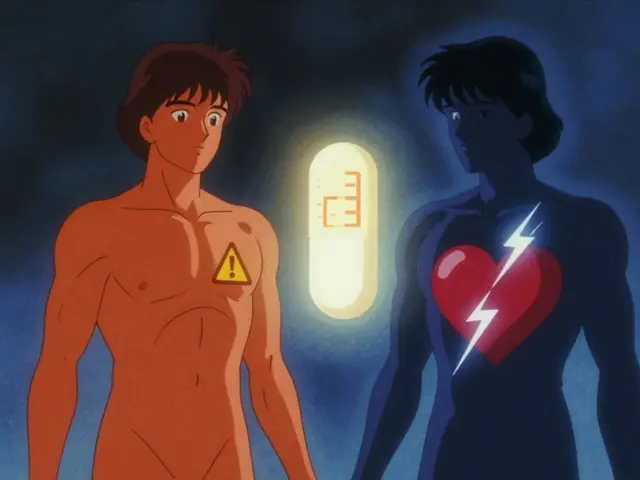
Cannabis isn’t just a mood lifter or a party drug. When you smoke or ingest it, the main psychoactive compound-delta-9-tetrahydrocannabinol (THC)-binds to CB1 receptors in your brain. These are the same receptors involved in regulating sleep, pain, and anxiety. The result? Slowed brain activity, reduced reaction time, and a heavy, relaxed feeling that feels calming… until it doesn’t.That’s because THC’s effects mirror those of prescription CNS depressants like benzodiazepines and barbiturates. Both types of substances enhance GABA, the brain’s main calming neurotransmitter. But unlike alcohol or Xanax, cannabis has a tricky dual nature. At low doses, it can feel stimulating-heart rate spikes, blood pressure rises. At higher doses, especially with THC levels above 10%, it flips into full depressant mode: dizziness, slurred speech, confusion, and extreme fatigue. And when mixed with other depressants, the shift happens faster and harder.
The Additive Effect: More Than Just Drowsiness
Here’s the critical part: the sedation from cannabis and other depressants doesn’t just add up-it multiplies. If you take 5 mg of THC and 0.5 mg of alprazolam, your body doesn’t just feel a little sleepy. It feels like you’ve been hit by a truck. Your breathing slows. Your reflexes vanish. Your ability to think clearly? Gone.A 2020 study in the Journal of Clinical Medicine found that people using both cannabis and benzodiazepines were over three times more likely to end up in the ER than those using benzodiazepines alone. Of those visits, nearly 70% involved respiratory problems. That’s not an accident. It’s a predictable outcome of two substances suppressing the same brainstem functions that keep you breathing while you sleep.
And it gets worse with opioids. Both THC and opioids like oxycodone or fentanyl act on different parts of the brain to slow breathing. Together, they create a dangerous synergy. The risk isn’t just higher-it’s exponential. The FDA has issued clear warnings: combining cannabis with opioids can lead to fatal respiratory depression. There’s no safe threshold. No warning sign that says, “One more puff and you’re done.”
Real Stories, Real Consequences
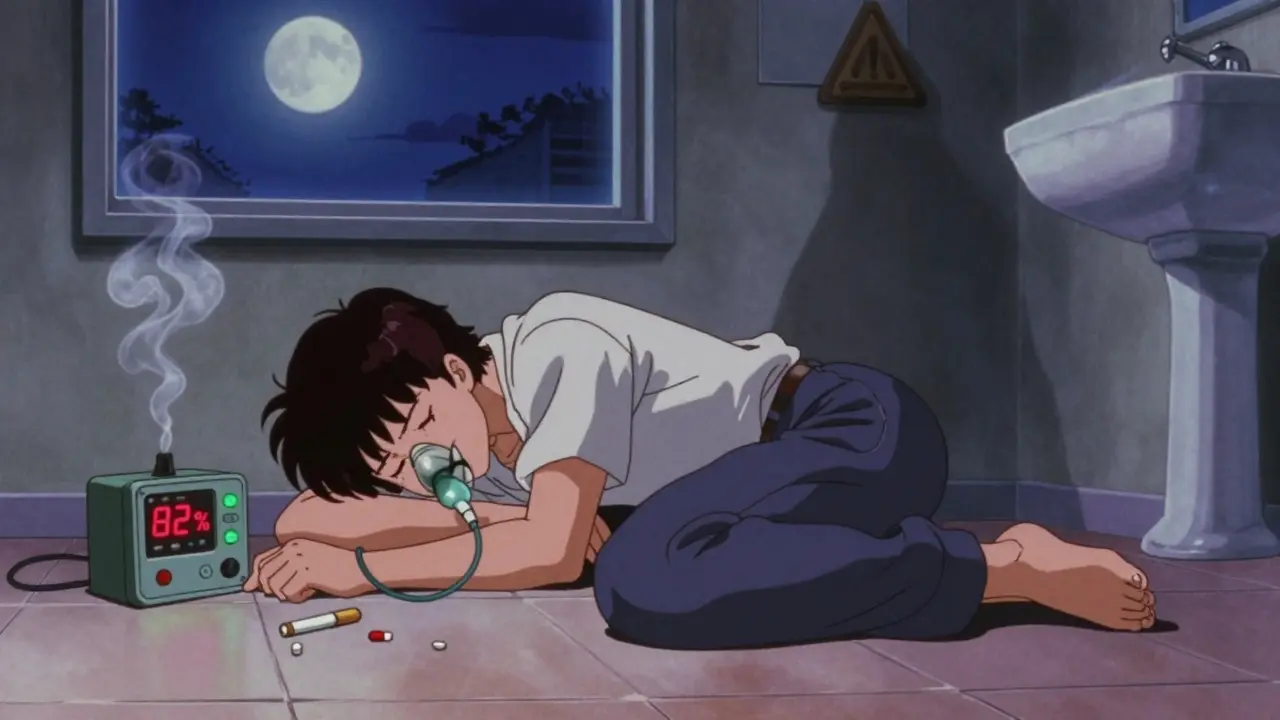
Reddit user u/AnxietyWarrior didn’t think twice. They took half a milligram of Xanax and one hit of 20% THC flower. Six hours later, they woke up on the bathroom floor. Their oxygen level had dropped to 82%. Normal is 95% or higher. That’s hypoxia. Brain damage territory.They weren’t alone. In 2022, U.S. emergency departments recorded over 7,800 visits involving cannabis and benzodiazepines-a 42% jump from just three years earlier. A survey of 1,247 medical cannabis users found that nearly one in five had experienced an episode so severe they needed medical help. One patient described it as “being trapped in my own body, awake but unable to move or speak for hours.”
These aren’t outliers. They’re symptoms of a growing blind spot in medical care. Many doctors don’t ask about cannabis use. Patients don’t volunteer it, thinking it’s “natural” and therefore safe. But natural doesn’t mean harmless. Especially when it’s mixed with prescription drugs.
Who’s at Highest Risk?
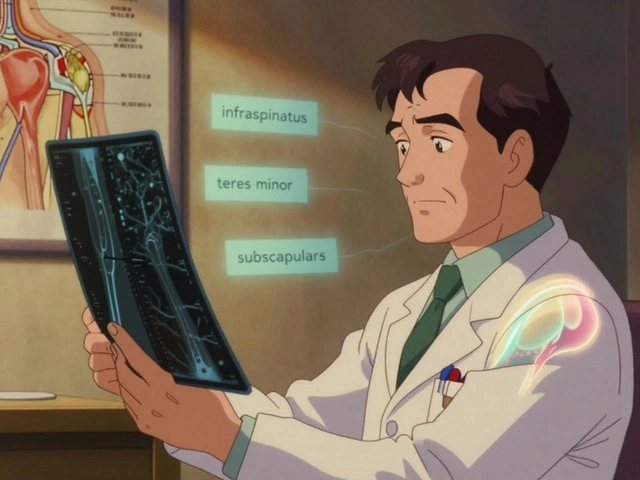
Older adults are the most vulnerable group. Many are managing chronic pain with opioids, anxiety with benzodiazepines, and insomnia with sleep aids. Then they start using cannabis for better sleep or to reduce their opioid dose. It sounds logical. It’s not.Age slows metabolism. Liver and kidney function decline. The body clears these drugs slower. THC lingers longer. The result? A buildup of sedation that can turn a mild nap into a coma. A 2021 study from Washington University showed that cannabis users needed 20-25% more propofol during surgery-but then had 37% more breathing problems afterward. That’s not tolerance. That’s toxicity.
People with sleep apnea, COPD, or heart disease are also at higher risk. Their bodies are already struggling to maintain oxygen levels. Adding cannabis on top? That’s like turning off the alarm before the house is on fire.
What About CBD?
Not all cannabis is the same. CBD-dominant products-those with high cannabidiol and less than 0.3% THC-show far fewer interaction risks. A 2022 double-blind trial in JAMA Internal Medicine gave 127 participants 150 mg of CBD with no THC and 0.5 mg of alprazolam. No significant interaction was found. No drop in breathing. No memory blackouts.This matters. If you’re using cannabis to reduce your reliance on benzodiazepines or opioids, CBD might be your safest path. But don’t assume. Many products labeled “CBD” still contain hidden THC. Always check lab reports. Look for third-party testing. And never use high-THC products if you’re on any CNS depressant.

What Should You Do?
If you’re taking any CNS depressant-prescription or not-here’s what you need to do:- Stop assuming cannabis is safe. Just because it’s legal or “natural” doesn’t mean it’s safe with your meds.
- Tell your doctor. If you’re using cannabis, even occasionally, say so. They need to know to adjust your doses or switch medications.
- Avoid high-THC products. Anything over 15% THC dramatically increases risk. Stick to low-dose options if you must use it.
- Don’t mix timing. Staggering doses by four hours doesn’t eliminate risk-it just delays it. The interaction still happens.
- Watch for warning signs. Extreme drowsiness, slurred speech, confusion, or difficulty waking up are red flags. Don’t wait for a blackout.
Some patients do use cannabis successfully alongside depressants under strict medical supervision. A 2022 case series from the University of Colorado showed 15 chronic pain patients reduced their opioid use by nearly half while using low-dose THC (2.5-5 mg). But every single one was monitored closely by a team. No one was left to guess.
What’s Being Done?
Regulators are catching up. The FDA now requires all prescription depressants to carry warnings about cannabis. The European Medicines Agency did the same in 2023. In California, doctors must complete a 2-hour training on cannabis-depressant interactions before certifying patients for medical marijuana. Since 2022, high-risk combinations have dropped by 28%.The American Society of Health-System Pharmacists created a simple risk tool: score points for THC concentration (up to 5), depressant type (opioids = 4, barbiturates = 5), and age over 65 (2 points). A score over 7? You’re in the danger zone. Time to reconsider.
Research funding has jumped from $28 million in 2020 to over $140 million in 2023. Scientists are now testing whether specific CBD-to-THC ratios can block dangerous interactions. Early results are promising.
Bottom Line
Cannabis isn’t the enemy. But pretending it’s harmless when mixed with depressants is deadly. The science is clear: combining them increases sedation, slows breathing, and raises the risk of overdose. It’s not a myth. It’s not a rumor. It’s documented, measured, and confirmed by hospitals, labs, and emergency rooms across the country.If you’re using cannabis and a CNS depressant, talk to your doctor today. Don’t wait for a blackout. Don’t wait for someone to find you on the floor. Your life isn’t worth the gamble.




Nicola George
27 December, 2025 01:19 AMI've seen this play out in South Africa with folks mixing cannabis and antiretrovirals. Same damn problem. Natural doesn't mean safe. Just means nobody's sued anyone yet.
Liz Tanner
28 December, 2025 04:16 AMMy aunt took Xanax and a gummy with 10mg THC for 'better sleep.' Woke up in the ER with oxygen at 81%. She still says it was 'just a fluke.'
Elizabeth Ganak
29 December, 2025 03:01 AMHonestly? I used CBD oil for anxiety while on propranolol and never had an issue. But I'd never touch high-THC stuff with my meds. Knowledge is power, folks.
Gerald Tardif
29 December, 2025 08:41 AMI'm a nurse who's seen this too many times. People think 'it's just weed' until they're gasping in the hallway. You don't need a PhD to know: don't mix.
Raushan Richardson
30 December, 2025 02:58 AMIf you're using cannabis to cut down on opioids, you're not being brave-you're being smart. But do it with a doctor holding your hand, not some guy on Reddit selling 'healing flower'.
James Bowers
30 December, 2025 04:32 AMThe empirical data is unequivocal. The pharmacodynamic synergy between CB1 agonists and GABAergic depressants results in a non-linear potentiation of respiratory depression, which constitutes a Class I clinical hazard. One must exercise extreme caution.
Will Neitzer
30 December, 2025 11:49 AMAs a physician who has treated dozens of these cases, I urge every patient to disclose cannabis use-not as an afterthought, but as a vital part of their medical history. The risks are not theoretical; they are quantifiable, preventable, and tragically common.
Olivia Goolsby
1 January, 2026 02:34 AMThey don't want you to know this-but the DEA and FDA have known about this synergy since the 90s! They let it slide because Big Pharma profits from prescriptions, and the cannabis industry is a threat! They're hiding the data, covering up the ER visits, and calling it 'natural' to keep you hooked on pills and scared of the plant! It's all a scam!!!
John Barron
1 January, 2026 10:40 AMI've read every paper on this. The 2020 J Clin Med study? Flawed. Small sample. Retrospective. And they didn't control for polypharmacy! Also, CBD doesn't help-it's just a placebo with a fancy label. And don't get me started on 'low-dose THC'-that's a marketing lie. 2.5mg? That's a joke. I've seen people crash on 1mg. 🤡
Janice Holmes
3 January, 2026 09:49 AMI took 15mg THC with 0.25mg Klonopin once. Woke up at 3 a.m. unable to move. Felt like my brain was wrapped in wet concrete. My dog licked my face for 20 minutes until I could blink again. That’s not relaxation-that’s a near-death experience. I haven’t touched either since. 🙏
Robyn Hays
3 January, 2026 21:03 PMI used to think CBD was just hippie nonsense. Then my mom, 72, with COPD and sleep apnea, started using it to replace her lorazepam. No more nighttime confusion. No more falls. She still gets her lab reports checked. Smart, slow, safe. That’s the model.
Anna Weitz
4 January, 2026 23:57 PMThe real danger isn't the weed it's the fear the fear of being honest the fear of asking the fear of admitting you're scared to stop your pills because you don't know who you are without them
Nikki Thames
6 January, 2026 18:29 PMThis is why we need mandatory screening. Everyone on benzodiazepines should be tested for cannabis use. And if they're using it? They need a behavioral intervention. Not advice. Not a pamphlet. A program. You can't just 'tell someone' to stop. Human beings are not rational actors. We are emotional creatures drowning in self-deception.
Monika Naumann
7 January, 2026 09:49 AMIn India, we have used cannabis for centuries in Ayurveda. To compare it with Western pharmaceuticals is a colonial mindset. You poison your body with pills and then blame the plant. The real problem is not cannabis-it is your broken healthcare system that sells addiction as treatment.