Living with rheumatoid arthritis (RA) isn’t just about pain and stiffness. It’s about knowing if your treatment is actually working-and if not, why. That’s where monitoring tools like CDAI, DAS28, and imaging come in. These aren’t just numbers on a page. They’re the compass that guides your care, helping doctors decide whether to keep going with your current meds, ramp up treatment, or switch entirely. Without them, you’re flying blind.
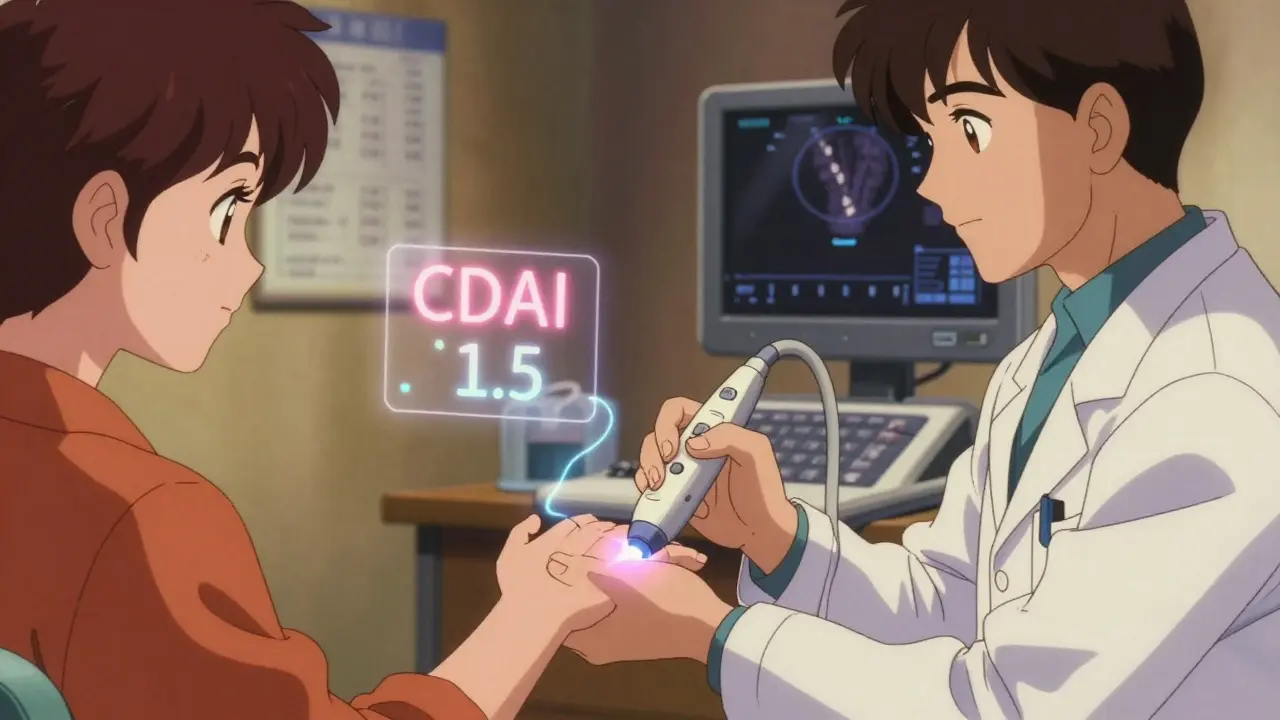
What Is CDAI and Why Do Doctors Use It?
The Clinical Disease Activity Index, or CDAI, is one of the simplest tools doctors use to measure how active your RA is. It doesn’t need blood tests. No labs. Just four things: how many tender joints you have, how many swollen joints, how bad you feel your pain is on a scale of 0 to 10, and how bad your doctor thinks it is on the same scale.
You add those four numbers together. The total? It can range from 0 to 76. If you score below 2.8? You’re in remission. Between 2.8 and 10? Low disease activity. Over 22? That’s high activity-and it’s time to act.
Why is this so popular? Because it’s fast. In a 15-minute visit, your rheumatologist can count your joints, ask you two quick questions, and get a clear picture. A 2023 study of over 3,800 patients found CDAI matched what doctors actually saw in the clinic better than almost any other score. It’s also built into most electronic health records now, so it pops up automatically after you fill out your symptoms.
But here’s the catch: CDAI doesn’t measure inflammation directly. If your body is quietly burning with inflammation but your joints don’t feel swollen, CDAI might say you’re doing fine. That’s why some doctors pair it with imaging or CRP tests-just to be sure.
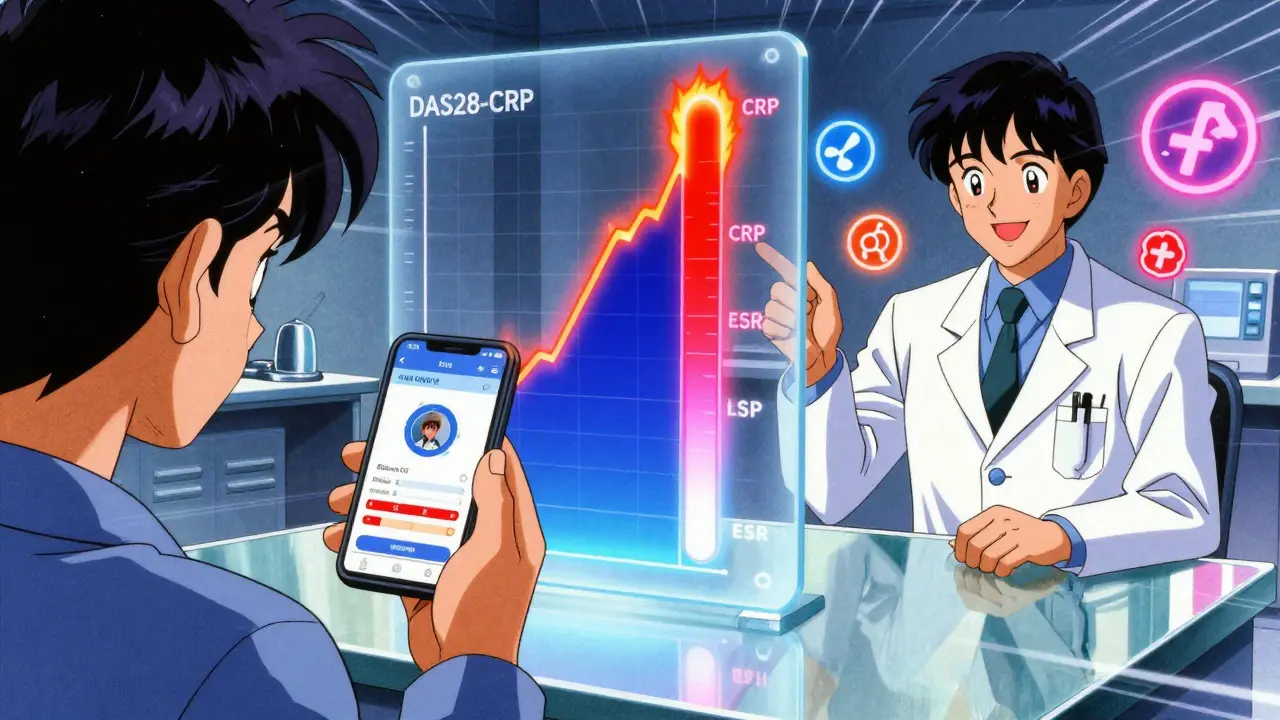
DAS28: The Score That Includes Blood Work
DAS28 is the older cousin of CDAI, developed in the 1990s. It uses the same joint counts-but adds a blood marker. There are two versions: DAS28-ESR (uses erythrocyte sedimentation rate) and DAS28-CRP (uses C-reactive protein). Both give you a number between 0 and 10.
Here’s how it breaks down:
- Under 2.6 = remission
- 2.6 to 3.2 = low activity
- 3.2 to 5.1 = moderate
- Above 5.1 = high
The big advantage? DAS28 picks up inflammation even when joints don’t look swollen. That’s useful if you’re on a biologic and your symptoms seem under control-but your CRP is still high. That’s a red flag.
But there’s a downside. Blood results often come back hours after your appointment. One survey found 68% of doctors had to make treatment decisions without knowing their patient’s latest CRP or ESR. That means you might leave the office with a plan that changes the next day when the lab report arrives. It’s frustrating. It’s inefficient.
That’s why in the U.S., CDAI has pulled ahead. In 2015, only 45% of rheumatology practices used it. By 2023, that jumped to 78%. In Europe, DAS28 is still more common-68% of clinics use it. But even there, many are starting to blend both.
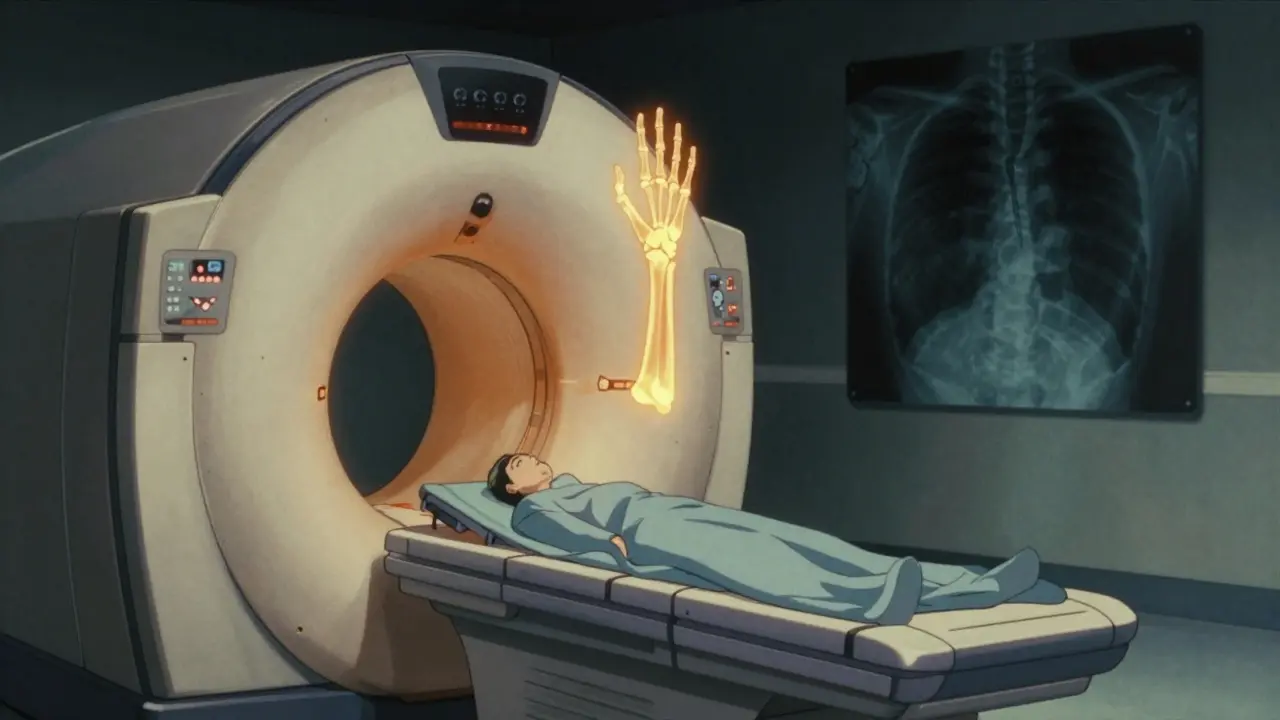
Imaging: Seeing What Your Eyes Can’t
Joint counts and blood tests tell you what’s happening now. Imaging tells you what’s been happening-and what’s coming.
For decades, X-rays were the only imaging tool available. They show bone damage-erosions, narrowing of joint spaces. But here’s the problem: it takes six to twelve months of active inflammation before X-rays show anything. By then, damage is already done.
That’s where ultrasound and MRI come in.
Ultrasound uses sound waves to show swelling inside joints-synovitis-and even blood flow in inflamed tissue, called power Doppler. It’s quick, cheap (around $150 in the U.S.), and can be done right in the clinic. Studies show it finds inflammation in 85% of cases where a physical exam misses it. And when doctors use ultrasound during visits, they change treatment plans in 22% of cases-just because they saw something the eye couldn’t.
MRI is even more powerful. It shows bone edema-the earliest sign of RA damage-up to a year before X-rays catch it. One study found MRI predicted future bone erosions with 89% accuracy. But it’s expensive ($1,200 per scan), takes longer, and isn’t available everywhere. Most clinics only use it for high-risk patients or when the diagnosis is unclear.
Doctors don’t order MRIs lightly. But when they do, it’s because they’re trying to catch damage before it’s irreversible. That’s the whole point of modern RA care: stop the damage before it starts.
Which Tool Should You Trust?
There’s no single best tool. It’s about using the right one at the right time.
If you’re stable, seeing your rheumatologist every six months, and your symptoms are under control? CDAI is perfect. It’s fast, free of lab delays, and correlates strongly with long-term outcomes. If your CDAI stays below 2.8 for six months? That’s a win.
If you’re on a new drug, your symptoms are flaring, or your blood work is weird? DAS28-CRP gives you extra insight. It tells you if inflammation is still ticking under the surface-even if your joints feel okay.
And if your doctor suspects hidden damage? That’s when imaging steps in. Ultrasound is becoming the go-to for routine checks. MRI is reserved for the trickier cases.
Here’s a real example: Sarah, 52, had been in remission for a year. Her CDAI was 1.5. But her CRP was rising. Her doctor ordered an ultrasound-and found active synovitis in her wrists. They adjusted her medication. Six months later, her CDAI was still 1.5-but now her CRP was normal and the ultrasound was clear. That’s the power of combining tools.
What About Patient Experience?
Monitoring isn’t just for doctors. It’s for you, too.
Many patients now use apps to track symptoms before visits. One survey found 68% of RA patients prefer digital symptom logging. But 42% said they felt anxious knowing their self-reported pain might change their treatment. That’s real. Your perception of pain matters-but it doesn’t always match your doctor’s. One Brazilian study found 33% of patients rated their pain much higher than their doctors did. That doesn’t mean they’re exaggerating. It means pain is personal.
And imaging? Some patients love ultrasound because they can see the swelling on the screen right away. Others hate MRIs-feeling pressured into scans they don’t understand. One forum user wrote: “I had three MRIs in two years. No one explained why. I felt like a lab rat.”
Good monitoring doesn’t just track disease. It includes you. That’s why experts now say: ask questions. Why are we doing this test? What will it change? What if we don’t do it?
The Future: Smarter, Faster, Personalized
The next wave of RA monitoring is already here.
AI tools can now analyze ultrasound images and automatically score inflammation-with 88% accuracy. New software integrates CDAI scores with imaging results and automatically flags when you’re at risk for damage. Some clinics are testing wearable sensors that track your hand movement, sleep, and activity levels 24/7.
By 2027, experts predict half of RA monitoring will come from remote data-your phone, your watch, your home ultrasound device-not just the clinic visit.
But here’s the truth: none of this replaces the human connection. A score can’t tell you if you’re too tired to play with your grandkids. A scan won’t know if you’ve stopped cooking because your wrists hurt too much. That’s why the best monitoring systems combine numbers with conversations.
RA isn’t just about joint counts and blood markers. It’s about your life. The tools are there to help you live better-not just to keep your scores low.
What’s the Bottom Line?
You don’t need every test every time. But you do need a plan.
- Use CDAI for routine check-ins-it’s fast, reliable, and built into your care.
- Use DAS28-CRP when inflammation might be hiding-especially if you’re on biologics.
- Use ultrasound when your doctor suspects hidden joint damage or needs to confirm a flare.
- Reserve MRI for high-risk cases or when treatment isn’t working and the cause is unclear.
And always ask: What will this test tell us? And what will we do differently if the answer changes?
RA monitoring isn’t about perfection. It’s about progress. And the right tools-used the right way-can keep you moving, working, living.
What’s the difference between CDAI and DAS28?
CDAI uses only clinical measures: tender joints, swollen joints, and patient and doctor global assessments. DAS28 adds a blood test-either ESR or CRP-to measure inflammation. CDAI is faster and doesn’t need lab results. DAS28 gives more insight into active inflammation but depends on blood work, which can delay decisions.
Can imaging show RA before joint damage appears?
Yes. MRI can detect bone edema (inflammation inside the bone) up to 6-12 months before X-rays show any erosion. Ultrasound can spot synovitis (joint lining swelling) before joints become visibly swollen. These are early warning signs that allow treatment to start before permanent damage occurs.
Why do some doctors prefer CDAI over DAS28?
CDAI doesn’t require blood tests, so results are immediate. In real-world clinics, lab delays mean DAS28 scores often can’t be calculated during the visit. CDAI is simpler, faster, and still strongly predicts long-term outcomes like joint damage. For routine care, it’s often more practical.
Is ultrasound better than X-rays for RA monitoring?
For early detection, yes. Ultrasound finds inflammation and fluid in joints much sooner than X-rays, which only show damage after months of disease. Ultrasound is also better at tracking changes over time. But X-rays remain the standard for measuring long-term bone damage in clinical trials because they’re widely available and have decades of historical data.
Should I get an MRI every year if I have RA?
No. MRIs are expensive and not needed for everyone. They’re typically used only when there’s uncertainty about disease activity, if you’re not responding to treatment, or if your doctor suspects hidden damage. Most people with stable RA only need X-rays or ultrasound annually-or even less often.
Can patient-reported scores be trusted?
They’re valuable-but not perfect. Patient reports (like how you feel on a 0-10 scale) help doctors understand your experience. But studies show patients often rate their pain higher than doctors do. That doesn’t mean it’s not real-it means pain is subjective. The best approach is to combine your report with objective measures like joint counts and blood tests.
What happens if my CDAI is low but my CRP is high?
That’s a red flag. It means your joints might not be swollen, but your body is still inflamed. This is called "subclinical inflammation" and can lead to joint damage over time. Your doctor may recommend a change in treatment-even if you feel fine-because the goal is to stop inflammation completely, not just manage symptoms.
Are there any downsides to using too many tests?
Yes. Over-testing can lead to anxiety, unnecessary costs, and even overtreatment. For example, if you’re stable and your CDAI is low, adding an MRI or extra blood tests won’t help-and might cause stress. The key is to use tests strategically: only when they’ll change your treatment plan.




Georgia Brach
23 December, 2025 19:01 PMThe CDAI is a gross oversimplification. Reducing complex systemic inflammation to a sum of four subjective scores ignores the immunological reality of RA. Doctors use it because it's convenient, not because it's accurate. Patients are being misled into thinking they're in remission when their cytokine levels are still spiking.
Payson Mattes
24 December, 2025 22:45 PMHey I read this and I'm just saying... what if the whole RA monitoring thing is just a big pharma scam? I mean, why do we need all these tests? Why not just let people feel their bodies? I heard from a guy on a forum that the FDA gets kickbacks from labs that do DAS28 blood work. And MRI machines? They're basically radioactive candy machines for hospitals. I got my cousin on a special diet and now he's off all meds. Just saying.
siddharth tiwari
26 December, 2025 00:24 AMin india most doc dont even know what cdai is. they just give methotrexate and say come back in 3 month. if pain go then ok if not then add steroid. imaging? who has 1200 rs for mri? we use xray and hope for best. no one care about subclinical inflamation. its all about what you can pay.
Diana Alime
27 December, 2025 08:04 AMI HATE when my dr says 'your CDAI is low so you're fine' and I'm crying in the car because I can't lift my coffee cup. I'm not exaggerating. I'm just... broken. And then they order a stupid ultrasound like I'm some lab rat and I feel like I'm being judged for not being 'well enough'. Why can't they just believe me? I'm not lazy. I'm not crazy. I'm just sick.
Adarsh Dubey
29 December, 2025 01:02 AMThis is actually one of the clearest explanations of RA monitoring I've seen. The balance between clinical tools and patient experience is handled well. I appreciate that it doesn't push one method as the universal answer. Real care is adaptive, not algorithmic. Good job.
Bartholomew Henry Allen
29 December, 2025 03:24 AMEurope still using DAS28? Pathetic. American medicine is superior. We don't waste time waiting for lab results. We act fast. CDAI is the future. If you're not using it you're practicing 20th century medicine. The rest of the world needs to catch up. No excuses.
Jeffrey Frye
29 December, 2025 04:12 AMSo let me get this straight... you're telling me that if my joints don't swell but my CRP is up, I'm still at risk? But my doctor says I'm 'in remission' because my CDAI is 1.2? That's... kind of terrifying. I mean, I'm not mad, just... confused. Like, if I'm not supposed to feel fine, why does everyone act like I should be? And why does it feel like I'm the only one who notices this gap?
niharika hardikar
31 December, 2025 00:16 AMThe integration of power Doppler ultrasound into routine rheumatology practice represents a paradigm shift in disease activity quantification. The ability to detect synovial vascularization prior to morphological joint destruction aligns with the treat-to-target paradigm. However, the lack of standardized training protocols across institutions introduces significant interobserver variability, thereby compromising longitudinal reliability. One must therefore contextualize imaging findings within the broader clinical-immunological matrix.
Jillian Angus
31 December, 2025 16:05 PMI've had two MRIs and one ultrasound. I didn't ask for any of them. They just happened. I didn't understand why. I just nodded. Now I feel like I'm being watched. Like my body is data. I don't need more scans. I need someone to sit with me and say 'this sucks'. That's all.
Aurora Daisy
2 January, 2026 13:49 PMOh look, another article that treats RA like a spreadsheet. How quaint. Let me guess - next they’ll be attaching QR codes to our wrists so we can ‘scan our pain levels’ while sipping our oat milk lattes. Meanwhile, actual people are lying on the floor trying to reach the bathroom. Numbers don’t cure. Compassion does. But who’s getting paid to write that article?
Paula Villete
3 January, 2026 17:28 PMIt's funny how we chase perfect scores while ignoring the messy truth: RA doesn't care if your CDAI is low. It waits. It hides. It steals your mornings, your laughter, your ability to hold your child. The tools help - yes. But they're not the cure. The cure is showing up, even when the numbers say you're fine. Even when the world says you should be better. You're not broken because your CRP is high. You're human.
Andrea Di Candia
4 January, 2026 05:27 AMThank you for writing this. I’ve been trying to explain to my family why I can’t just ‘push through’ when my CDAI is low but my body feels like it’s been run over. This article gives me the language to say: it’s not in my head. It’s not weakness. It’s inflammation that doesn’t always show up where you’re looking. That’s huge.
Dan Gaytan
6 January, 2026 04:56 AMMy rheum just started using ultrasound in her office 😍 I saw the swelling in my wrist on the screen for the first time and I cried. Not because it was bad - because I finally saw it. I wasn’t imagining it. I’m not crazy. And now we’re adjusting my meds. Thank you for making this so clear. I’m sharing this with everyone I know.