Ever felt queasy on a boat ride and then noticed you’re a bit off‑balance even after you step onto solid ground? That isn’t a coincidence - the same inner‑ear mechanisms that trigger motion sickness also keep us upright. Understanding how these two conditions overlap can help you spot the warning signs early and choose the right treatment.
Key Takeaways
- Motion sickness and balance disorders share a common root in the vestibular system of the inner ear.
- Typical symptoms include nausea, dizziness, and disorientation, often worsening together.
- Accurate diagnosis relies on vestibular testing and posture assessments.
- Effective management blends medication, vestibular rehabilitation, and lifestyle tweaks.
- Early intervention can prevent chronic balance issues and improve quality of life.
What Is Motion Sickness?
Motion sickness is a condition that arises when the brain receives mismatched signals about movement from the eyes, inner ear, and muscles. The classic scenario involves sitting in a car, looking at a stationary phone, and feeling the car’s motion through the inner ear - the brain can’t reconcile the two inputs, leading to nausea, cold sweats, and sometimes vomiting.
Common triggers include sea travel, amusement‑park rides, virtual reality headsets, and even reading in a moving vehicle. While most people experience it occasionally, a subset develops a heightened sensitivity that can interfere with daily activities.
Understanding Balance Disorders
Balance disorders are a group of conditions that impair the body’s ability to maintain equilibrium. They range from temporary episodes caused by ear infections to chronic vestibular dysfunctions such as benign paroxysmal positional vertigo (BPPV) or Menière’s disease.
Symptoms often overlap with motion sickness - dizziness, a spinning sensation (vertigo), and unsteady gait - which is why many patients report both issues simultaneously.
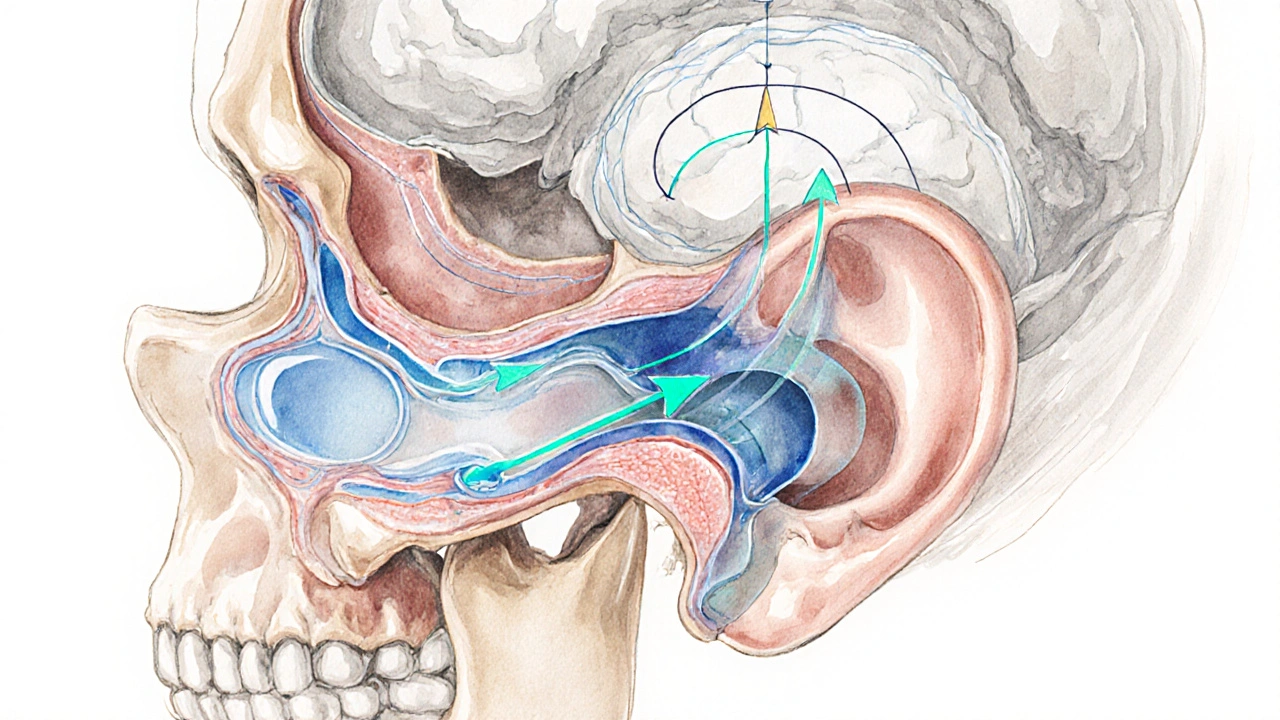
The Vestibular Connection - How the Inner Ear Links Motion Sickness and Balance
The vestibular system is a network of fluid‑filled canals and otolith organs inside the inner ear. It detects angular acceleration (rotations) and linear acceleration (straight‑line movements) and sends this data to the brainstem.
Two key structures - the semicircular canals and the otolith organs (utricle and saccule) - work together to inform us of head position and motion. When these organs send inaccurate or contradictory signals, both motion sickness and balance disorders can arise.
Shared Symptoms: Nausea, Dizziness, and Disorientation
Nausea is the most recognizable sign of motion sickness, but it also appears in many vestibular disorders when the brain interprets abnormal motion cues as toxic.
Dizziness, often described as a feeling that the room is spinning, can stem from either condition. In motion sickness, it usually resolves once the motion stops; in balance disorders, it may persist or recur with head movements.
Disorientation - a sense of not knowing which way is up - is particularly common when both the vestibular system and visual inputs are out of sync, such as during virtual reality exposure combined with an underlying vestibular weakness.
Diagnosis - Tests That Reveal the Link
Because the symptoms overlap, clinicians use a battery of vestibular assessments to pinpoint the root cause. Below is a quick guide to the most common tests and what they evaluate.
| Test | What It Measures | Typical Findings in Motion Sickness | Typical Findings in Balance Disorders |
|---|---|---|---|
| Electronystagmography (ENG) | Eye movements in response to vestibular stimulation | Normal or mild latency | Abnormal gain or asymmetry |
| Video Head Impulse Test (vHIT) | Semicircular canal function during rapid head turns | Usually normal | Reduced vestibulo‑ocular reflex gain |
| Dynamic Posturography | Balance performance under changing visual and surface conditions | Occasional sway during motion exposure | Significant instability across conditions |
| Rotational Chair Test | Response of the vestibular system to controlled rotations | Heightened sensitivity at low frequencies | Reduced response amplitude |

Treatment Approaches - From Medication to Rehabilitation
Managing the dual impact of motion sickness and balance disorders often requires a multi‑pronged plan.
Medication
- Antihistamines (e.g., meclizine) dampen vestibular signals and can reduce nausea.
- Scopolamine patches are useful for prolonged travel.
- In chronic vestibular disorders, benzodiazepines may be prescribed short‑term to control vertigo.
Vestibular rehabilitation (VR) is a targeted exercise program that promotes central compensation. It includes gaze‑stabilization drills, balance training on foam surfaces, and habituation movements that gradually expose patients to the motions that provoke symptoms.
Research from the American Academy of Neurology (2023) shows that an eight‑week VR program improves Dizziness Handicap Inventory scores by an average of 20 points, cutting reliance on medication.
Other supportive strategies include:
- Hydration and light meals before travel.
- Choosing a seat with the most stable motion (e.g., middle of a plane, near the ship’s center).
- Using ginger or acupressure bands for mild nausea.
- Limiting visual clutter - look at the horizon rather than reading while moving.
Practical Tips to Manage Both Conditions
Even if you haven’t been formally diagnosed, these everyday habits can keep the vestibular system happy.
- Start with short exposure sessions (e.g., 10‑minute car rides) and gradually increase duration.
- Practice the “two‑step” technique: inhale through the nose for 4 seconds, hold for 2, exhale through the mouth for 6. This breathing pattern stabilizes the autonomic nervous system.
- Incorporate balance‑challenging activities like single‑leg stands or yoga to strengthen proprioceptive feedback.
- When using VR headsets, take 5‑minute breaks every 20 minutes and keep the play area well‑lit.
- If symptoms flare up, stop the motion, focus on a fixed point, and sip water with a pinch of salt to support inner‑ear fluid balance.
Frequently Asked Questions
Can motion sickness cause a permanent balance disorder?
Acute motion sickness itself doesn’t damage the vestibular system, but repeated severe episodes can lead to heightened sensitivity, known as vestibular hyper‑responsiveness. In rare cases, this can evolve into a chronic balance issue if underlying vestibular health is already compromised.
Why do some people feel dizzy long after a boat trip ends?
Post‑travel dizziness often reflects a lag in the vestibular system’s recalibration. The brain needs time to re‑weight visual and proprioceptive cues after the motion stops. Gentle walking and looking at fixed points can speed up this reset.
Is there a test that can differentiate motion sickness from a true vestibular disorder?
Dynamic posturography combined with video head impulse testing is the most reliable approach. Motion sickness typically yields normal vestibulo‑ocular reflexes, whereas a true vestibular pathology shows abnormal gains or asymmetries.
Can vestibular rehabilitation help someone who only gets motion sickness?
Yes. Habituation exercises gradually expose the vestibular system to the provocative motions, reducing the mismatch that causes nausea. Many travel‑frequent flyers report fewer sick days after an eight‑week VR program.
Are there lifestyle changes that lower the risk of both conditions?
Maintaining good hydration, regular exercise that challenges balance, and limiting caffeine and alcohol before travel all support vestibular health. Consistent sleep patterns also help the brain process sensory inputs more smoothly.




George Kata
9 October, 2025 17:50 PMInteresting read on how the vestibular system ties motion sickness to balance issues. I’ve noticed that taking a quick walk after a boat ride helps me recalibrate. Staying hydrated and chewing ginger candy can also calm the nausea. The article’s tip about the two‑step breathing technique is spot on. Keep sharing posts like this, they’re super useful.
Nick Moore
12 October, 2025 01:23 AMTotally agree, the breathing trick is a game‑changer. I try it on long drives and it keeps the queasy feeling at bay.
Jeffery Reynolds
14 October, 2025 08:56 AMWhile the article does a decent job outlining the vestibular connection, there are a few technical inaccuracies that deserve clarification. First, the term “inner‑ear mechanisms” should be specified as the semicircular canals and otolith organs, not a vague generic. Second, motion sickness is not merely a mismatch of visual and proprioceptive cues; it involves the vestibulo‑ocular reflex and the autonomic nervous system. Third, the claim that antihistamines “dampen vestibular signals” oversimplifies their anticholinergic action, which primarily blocks histamine H1 receptors. Fourth, not all patients with benign paroxysmal positional vertigo will benefit from scopolamine patches; many require canalith repositioning maneuvers. Fifth, the table of vestibular tests omits the caloric test, which remains a gold standard for assessing horizontal canal function. Sixth, dynamic posturography results are influenced by test surface stiffness, a variable the article does not address. Seventh, the statement that “hydration and light meals before travel” prevent motion sickness lacks robust clinical evidence; many studies show mixed outcomes. Eighth, the recommendation to “look at the horizon” is valid, but for VR exposure, a stable visual reference point within the headset is more practical. Ninth, vestibular rehabilitation programs should be individualized; a one‑size‑fits‑all eight‑week protocol may not suit patients with severe BPPV. Tenth, the article mentions “vestibular hyper‑responsiveness” without defining the diagnostic criteria, which can lead to confusion. Eleventh, the role of genetics in susceptibility to motion sickness is an emerging field that merits mention. Twelfth, recent literature suggests that low‑dose propranolol can modulate vestibular sensitivity, an option not covered here. Thirteenth, the discussion of Menière’s disease should include the importance of low‑salt diets and intratympanic steroid injections. Fourteenth, the article could benefit from citing the 2023 American Academy of Neurology guidelines more explicitly. Fifteenth, overall, a more rigorous peer‑reviewed reference list would enhance credibility. In summary, the piece is a good overview but requires these refinements to serve clinicians and patients accurately.
Mitali Haldankar
16 October, 2025 16:30 PMWow, never thought the brain could get so confused – 🤯
snigdha rani
19 October, 2025 00:03 AMSure, the brain can be a drama queen, but the fix isn’t rocket science. Hydrate, avoid heavy meals, and do a few head‑tilt exercises before you board. If you still feel funky, a quick session of gaze‑stabilization can reset things. Honestly, most of the “mystery” disappears with simple habit tweaks.
Mike Privert
21 October, 2025 07:36 AMNice breakdown! Adding a short daily balance drill, like standing on one foot while brushing teeth, can further condition the vestibular system. Consistency is key – even five minutes a day makes a difference.
Veronica Lucia
23 October, 2025 15:10 PMThe interplay between sensory input and perception is a profound reminder of how our bodies maintain stability. When we consciously engage in balance training, we reinforce neural pathways that support equilibrium. It’s fascinating that a simple breath can modulate the autonomic response to motion. Integrating mindfulness with vestibular exercises may unlock even greater resilience.
Sriram Musk
25 October, 2025 22:43 PMStudies show that vestibular rehabilitation improves DHI scores by roughly 20 points after eight weeks, confirming the article’s claim. Moreover, the video head impulse test reliably distinguishes peripheral from central vestibular deficits. For travelers, placing a small mirror to view the horizon can reduce sensory conflict. Finally, low‑dose meclizine remains a first‑line option for short‑term relief.
allison hill
28 October, 2025 05:16 AMHonestly, the heavy reliance on medication feels like a shortcut that the industry pushes. Many patients could achieve similar results with non‑pharmacologic strategies if given proper guidance. There’s also a growing body of evidence suggesting that some drugs may blunt neuroplasticity during rehab.
Tushar Agarwal
30 October, 2025 12:50 PMGood points, Allison 😊. I’ve seen patients thrive after swapping meds for a structured vestibular program, so it’s worth considering.
Richard Leonhardt
1 November, 2025 20:23 PMGreat insights all around! Remember to start with short exposure sessions and gradually increase duration – the body adapts much better that way. Keep experimenting with hydration, diet, and breathing; you’ll find the combo that works best for you.
Shaun Brown
4 November, 2025 03:56 AMThe article attempts to be comprehensive but ends up being a patchwork of loosely connected facts. It jumps from medication lists to breathing exercises without establishing a coherent treatment hierarchy. Readers are left wondering which intervention should take precedence. Moreover, the use of buzzwords like “cutting‑edge” feels disingenuous when the recommendations are largely textbook. The lack of discussion on contraindications for certain drugs is a glaring omission. Overall, the post reads more like a promotional brochure than an evidence‑based guide.
Damon Dewey
6 November, 2025 11:30 AMPretty bland overview, nothing new here.