When a child takes a medicine, their body doesn’t just shrink down to fit an adult’s blueprint. Their organs are still growing. Their enzymes are still waking up. Their chemistry is changing by the week. That’s why a drug that works fine for mom or dad can send a child to the hospital - even at the right dose.
Why Kids Aren’t Just Small Adults
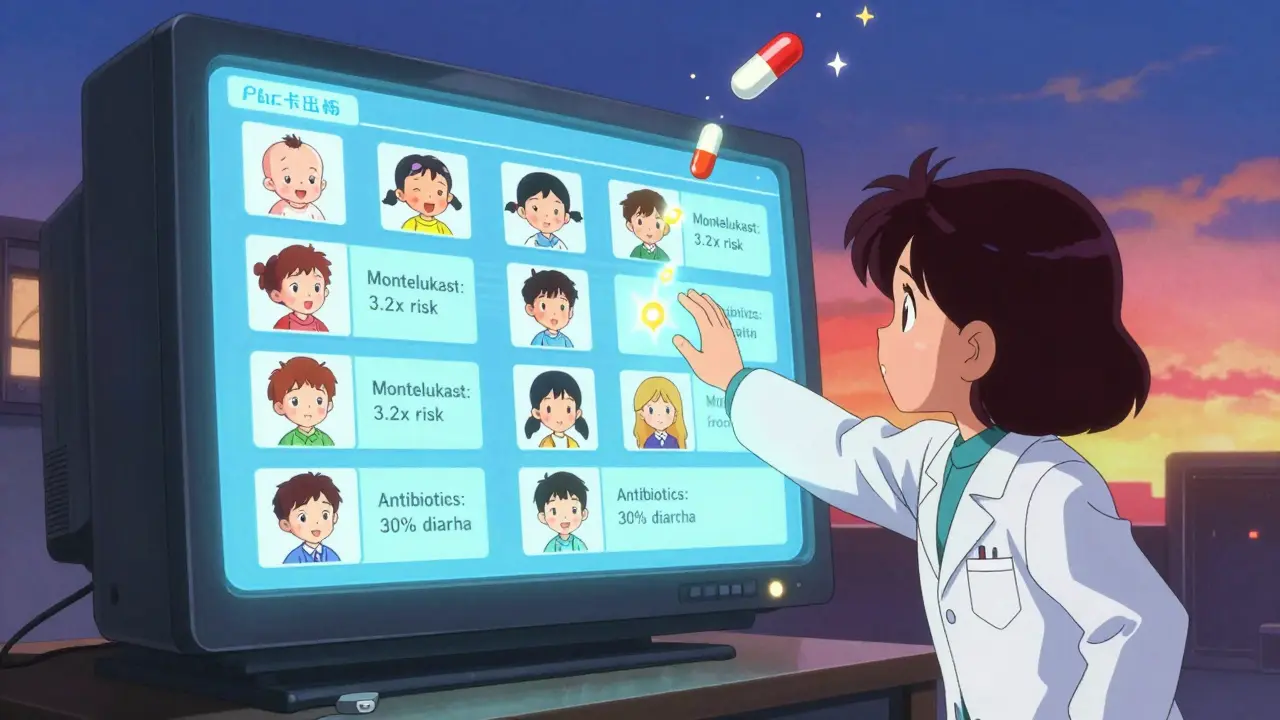
Most drugs are tested first in adults. Then, doctors guess the dose for kids based on weight. But that’s like using the same recipe for a cake and a cupcake - the ingredients might be the same, but how they bake is totally different. Children’s bodies change dramatically in the first few years of life. A newborn has 75-80% water in their body, compared to about 60% in adults. That means water-soluble drugs spread out more, lowering their concentration. By age two, that ratio flips. Liver enzymes that break down drugs? They’re barely active in newborns. By six months, some are working at twice the adult rate. By age five, they’re often faster than adults at clearing certain medications. This isn’t just theory. A 2023 Columbia University study analyzed over 264,000 pediatric drug reactions reported to the FDA. It found that children under two - especially between 12 and 24 months - are at the highest risk for serious side effects. One drug, montelukast (used for asthma), showed a 3.2 times higher risk of mood changes, nightmares, and agitation during that exact window. That’s not a coincidence. It’s biology.The Hidden Dangers: Drugs That Are Riskier for Kids
Some medications are simply not safe for children, no matter the dose. The KIDs List, developed by Mayo Clinic and published in American Family Physician in 2021, highlights the most dangerous ones:- Loperamide (Imodium): Can cause fatal heart rhythm problems in kids under six. Even one extra tablet can be deadly.
- Aspirin: Linked to Reye’s syndrome - a rare but often fatal liver and brain disorder - in children recovering from viruses like flu or chickenpox.
- Codeine: Metabolized differently in kids due to genetic variations. One in 30 children are “ultra-rapid metabolizers,” turning codeine into morphine too fast, leading to breathing problems or death.
- Benzocaine teething gels: Caused over 400 cases of methemoglobinemia (a blood disorder that reduces oxygen delivery) between 2006 and 2011. The FDA banned them for children under two in 2018.
How Often Do Side Effects Happen?
You might hear that only 2-5% of children have side effects from medications. That number comes from older studies and doesn’t reflect today’s reality. In outpatient settings, mild reactions like upset stomach or drowsiness do happen in about 15-20% of cases - and usually fade after a few days. But when kids are hospitalized, the numbers jump. One in five hospitalized children experiences at least one adverse drug reaction, and nearly half of those are serious enough to require extra treatment or extend their stay. That’s according to Dr. Michael J. Arnold’s 2021 analysis in American Family Physician. Antibiotics top the list. About 25-30% of kids on antibiotics like amoxicillin-clavulanate get severe diarrhea or vomiting - especially under age two. Antihistamines cause drowsiness or agitation in 15-20% of children, compared to just 5-10% of adults. Psychiatric drugs like SSRIs or stimulants carry 2-3 times the risk of severe reactions in kids under 12.
Why So Many Drugs Are Used Off-Label
Only about half of all drugs prescribed to children have been studied specifically for them. That’s not because doctors are careless. It’s because the system is broken. Drug companies don’t always test medicines on kids. It’s expensive. It’s harder to get consent. And until recently, there was little financial incentive. The Best Pharmaceuticals for Children Act of 2002 offered patent extensions to companies that did pediatric studies. Since then, over 400 drugs have gained new pediatric labeling. But the gap is still huge. In neonatal intensive care units, 79% of drugs are used off-label. For kids with rare diseases, 95% have no FDA-approved treatment at all. And while the global pediatric drug market is worth nearly $100 billion, it’s still only 12-15% of the total pharmaceutical industry - even though kids make up 22% of the U.S. population.What Parents and Caregivers Should Watch For
Not every side effect is an emergency. But knowing the warning signs can save a life.- Mild reactions - nausea, drowsiness, mild rash - often go away after a few days. Keep giving the medicine unless your doctor says otherwise. Track symptoms in a notebook: what time, what dose, how the child acted.
- Call 911 or go to the ER immediately if you see: Trouble breathing, swelling of the face or tongue, rapid or irregular heartbeat (especially if the drug isn’t supposed to speed up the heart), seizures, or sudden confusion.
- Watch for behavioral changes - especially with asthma, ADHD, or sleep meds. New aggression, severe insomnia, or withdrawal can signal a reaction, not just a phase.
What’s Changing - And What’s Next
There’s real progress. In 2023, Columbia University launched KidSIDES, a free public database with 1,847 validated drug-side effect pairs mapped to specific age groups. The FDA’s Pediatric Drug Safety Portal (PDSportal) lets doctors see how a drug’s risks change from infancy to adolescence. The NIH is funding a $15 million study to build age-specific pharmacogenomic guidelines - meaning we’ll soon be able to test a child’s genes to predict how they’ll react to certain drugs. That’s precision medicine for kids. The American Academy of Pediatrics is pushing for a new rule: every new drug targeting childhood conditions must come in a child-friendly formulation. That means not just smaller pills, but flavors, liquids, and dosing tools designed for kids. They estimate this could prevent 30,000 to 50,000 hospitalizations every year.What You Can Do Today
You don’t need to be a doctor to protect your child from dangerous drug reactions.- Always ask: “Has this been tested in kids this age?”
- Double-check the dose. Weight matters - not age. Use a syringe, not a teaspoon.
- Never give aspirin to a child with a fever or virus.
- Keep a list of all medications - including over-the-counter and supplements - and share it with every provider.
- Report side effects to the FDA’s MedWatch program. Your report helps other families.
Are all pediatric drug side effects dangerous?
No. Many side effects - like mild nausea, drowsiness, or a small rash - are temporary and go away after a few days as the body adjusts. These are common and usually not serious. But any new symptom that’s severe, sudden, or worsening should be checked by a doctor right away. The key is knowing the difference between expected mild reactions and warning signs like trouble breathing, swelling, or extreme behavioral changes.
Why is weight used instead of age to calculate pediatric doses?
Weight matters more than age because children’s bodies vary widely in size and metabolism, even within the same age group. A 2-year-old weighing 30 pounds processes drugs differently than a 2-year-old weighing 50 pounds. Dosing by weight (mg/kg) accounts for differences in body composition, organ size, and metabolic rate. Age is a rough guide, but weight gives a more accurate starting point - especially for infants and toddlers.
Is it safe to give my child adult medicine if I cut the dose in half?
No. Adult medications are not designed for children’s bodies. The inactive ingredients, coatings, or release mechanisms may be unsafe. Some drugs, like aspirin or codeine, can be deadly even in small amounts. Never split adult pills or guess doses. Always use medications specifically labeled for children or approved by a pediatrician.
What should I do if my child has a reaction to a new medication?
Stop giving the medication and call your pediatrician immediately. If symptoms are severe - like difficulty breathing, swelling, seizures, or loss of consciousness - go to the emergency room or call 911. Keep the medication bottle and write down when the reaction started, what symptoms appeared, and how they’ve changed. This information helps doctors identify the cause and report it to the FDA.
How can I find out if a drug is on the KIDs List?
The KIDs List is available in the May 2021 issue of American Family Physician and through the Mayo Clinic’s website. Ask your child’s doctor if the prescribed medication is on the list. You can also search the FDA’s Pediatric Drug Safety Portal (PDSportal) for safety signals tied to specific drugs and age groups. If a drug is flagged for high risk in children, your doctor should discuss alternatives.
Are generic drugs safer or riskier for children than brand-name ones?
Generic drugs contain the same active ingredient as brand-name versions and are required to meet the same FDA standards for safety and effectiveness. The risk of side effects is not higher or lower based on whether the drug is generic or brand-name. What matters is whether the drug has been studied in children and if the dosage form is appropriate. Always check if the generic version has pediatric labeling - many don’t, even if the brand-name version does.




Enrique González
4 January, 2026 01:36 AMMy niece had a bad reaction to amoxicillin last year - vomiting nonstop for 36 hours. We thought it was a stomach bug until the pediatrician asked about meds. Now I always ask: ‘Is this tested for kids this age?’ Simple question. Life-changing answer.
Doctors don’t always know the latest data. We’ve got to be their partners, not just passive recipients.
Also - use a syringe. Not a spoon. Trust me.
Parenting is full of guesswork. This isn’t one of them.
Aaron Mercado
5 January, 2026 16:09 PMTHIS IS WHY WE NEED TO BAN ALL PHARMA COMPANIES FROM TESTING ON KIDS!!!
They don’t care! They just want profit! Codeine? Aspirin? Loperamide? These are KILLERS disguised as cures!
And the FDA? They’re asleep at the wheel! 79% of NICU drugs are off-label?! That’s not negligence - that’s MASS MURDER BY MATH!!!
My cousin’s baby died from a ‘safe’ dose of something labeled ‘for children’ - it was never tested on babies under 6 months!
WE NEED A REVOLUTION. NOT MORE STUDIES. MORE JAIL TIME FOR EXECUTIVES.
And yes - I’m angry. You should be too.
saurabh singh
7 January, 2026 08:23 AMMan, this hits different coming from the US - in India, we just give whatever’s available and pray. No pediatric labeling? No problem - we crush pills, mix with honey, and hope.
But honestly? This article changed my game. I’m a nurse in Delhi, and I’ve seen kids crash from adult antihistamines. We don’t have PDSportal here, but I’m printing this out and laminating it for our clinic.
Also - no aspirin. Ever. Even if grandma says ‘it worked for me.’ Kids ain’t us.
Thanks for writing this. Sharing with every parent I know.
Dee Humprey
8 January, 2026 17:28 PMMy son had nightmares after montelukast. We thought it was just bad dreams - until I read this.
We stopped it. Within 48 hours, he slept like a log again.
Don’t ignore behavioral changes. They’re not ‘just a phase.’ They’re your child’s body screaming.
Keep a log. Even if it’s just notes on your phone. It helps more than you think.
And if your doctor brushes it off? Find a new one.
❤️
John Wilmerding
9 January, 2026 07:13 AMWhile the data presented is compelling and aligns with contemporary pediatric pharmacokinetic research, it is imperative to recognize that off-label prescribing remains a necessary clinical practice in the absence of robust pediatric-specific trials. The ethical and logistical challenges of pediatric clinical research are well-documented, and the current regulatory incentives, while improved since 2002, remain insufficient to fully close the knowledge gap.
Moreover, the distinction between pharmacodynamic and pharmacokinetic variability across developmental stages must be emphasized in clinical education. Dosing by weight alone is insufficient without consideration of organ maturation, protein binding, and renal clearance trajectories.
Further, the KIDs List, while valuable, should be contextualized within therapeutic necessity - not used as a rigid blacklist. Clinical judgment remains paramount.
mark etang
9 January, 2026 14:25 PMAs a former clinical pharmacist who worked in pediatric oncology, I can tell you: we’re flying blind in 80% of cases.
One kid got a fatal reaction to a chemo combo because the adult dose was halved - but the metabolite buildup was 3x higher due to immature liver enzymes.
We didn’t know until it was too late.
That’s why I now insist on pharmacogenomic testing before any new med. It’s not standard. It should be.
And yes - I’ve lost patients. I still wake up thinking about them.
This isn’t just policy. It’s personal.
Ethan Purser
10 January, 2026 05:24 AMWhat if the real problem isn’t the drugs… but the idea that we can ‘fix’ childhood with chemistry?
We’ve turned kids into data points. A weight. An age. A dose.
But they’re not machines. They’re living, breathing, evolving systems - and we treat them like broken gadgets we’re trying to recalibrate.
Maybe the answer isn’t better dosing… but fewer drugs.
What if we stopped trying to medicate every cry, every tantrum, every sleepless night?
Just… sit with it?
Just… let them be?
…I’m not saying don’t use meds.
I’m saying: why are we so quick to reach for them?
Stephen Craig
11 January, 2026 22:55 PMWeight-based dosing works better than age-based, but only if the weight is accurate.
Parents often guess. Or the scale is broken.
Always double-check the scale. And write it down.
Simple. Critical.
And never trust a pill splitter for kids.
Roshan Aryal
13 January, 2026 01:24 AMOh wow, another American medical elitist rant. You think your fancy FDA labels and Columbia studies mean anything in the real world?
In India, Africa, Latin America - we don’t have PDSportal. We don’t have syringes. We have one bottle of syrup and 12 kids.
You think cutting a pill in half is dangerous? Try giving a 3-year-old half a tablet when you have no idea what’s inside.
So yeah - your ‘science’ is great. But it’s a luxury. Most parents are just trying to keep their kid alive with whatever’s on the shelf.
Stop preaching. Start fixing.
Jack Wernet
14 January, 2026 09:23 AMThank you for this comprehensive and deeply necessary overview. The disparity between adult and pediatric pharmacology remains one of the most under-addressed public health issues in modern medicine.
I have shared this with my medical students and colleagues. The KIDs List should be mandatory reading for all prescribers who treat children.
Additionally, the emphasis on behavioral side effects - particularly with CNS-active medications - is long overdue.
Continued advocacy and research funding are essential. This is not a niche concern. It is foundational.
Charlotte N
14 January, 2026 14:53 PMI didn’t realize how much I didn’t know until I read this
My daughter got amoxicillin and got a rash - we thought it was allergies
Turned out it was just a reaction - stopped it, it went away
But I didn’t know to track it
Now I do
Thanks
Catherine HARDY
15 January, 2026 22:44 PMDid you know the FDA gets paid by drug companies? That’s why they approve stuff that kills kids.
Montelukast? The same company that made Vioxx.
They knew. They just hid it.
Why do you think they pushed it for toddlers? More profit.
And now they’re making a ‘portal’ like it’s a fix?
It’s all a scam.
Don’t trust the system.
Go natural.
Herbs. Homeopathy. Prayer.
They don’t have side effects.
…or do they?
bob bob
17 January, 2026 17:59 PMMy kid had a bad reaction to an antihistamine - hyper, couldn’t sleep, screaming at 3am.
Turned out it was the drug. Not a tantrum.
I felt so guilty.
Now I always ask: ‘What’s the worst thing that could happen?’
And I don’t trust the pharmacist’s advice unless they’ve got a kid.
Just… be careful.
Love you all.
Vicki Yuan
18 January, 2026 03:02 AMOne of the most important things missing from most discussions: formulation matters.
A liquid suspension with artificial flavoring can trigger reactions in kids with sensitivities - even if the active ingredient is safe.
Also: many generics use different fillers than brand-name versions. Some contain dyes or preservatives linked to behavioral changes.
Always check the inactive ingredients. They’re not inert.
And if you can’t find a dye-free, alcohol-free, sucrose-free version? Ask for a compounding pharmacy.
It’s extra work. But it’s worth it.
Uzoamaka Nwankpa
19 January, 2026 20:23 PMMy daughter got a fever after her vaccine. I gave her children’s Tylenol. She got a rash. Then she stopped eating.
Three days later, she was in the hospital.
The doctor said it was the medicine.
I didn’t know.
I just wanted to help.
Now I don’t give anything without asking.
And I cry every time I see a medicine bottle.
Sorry.