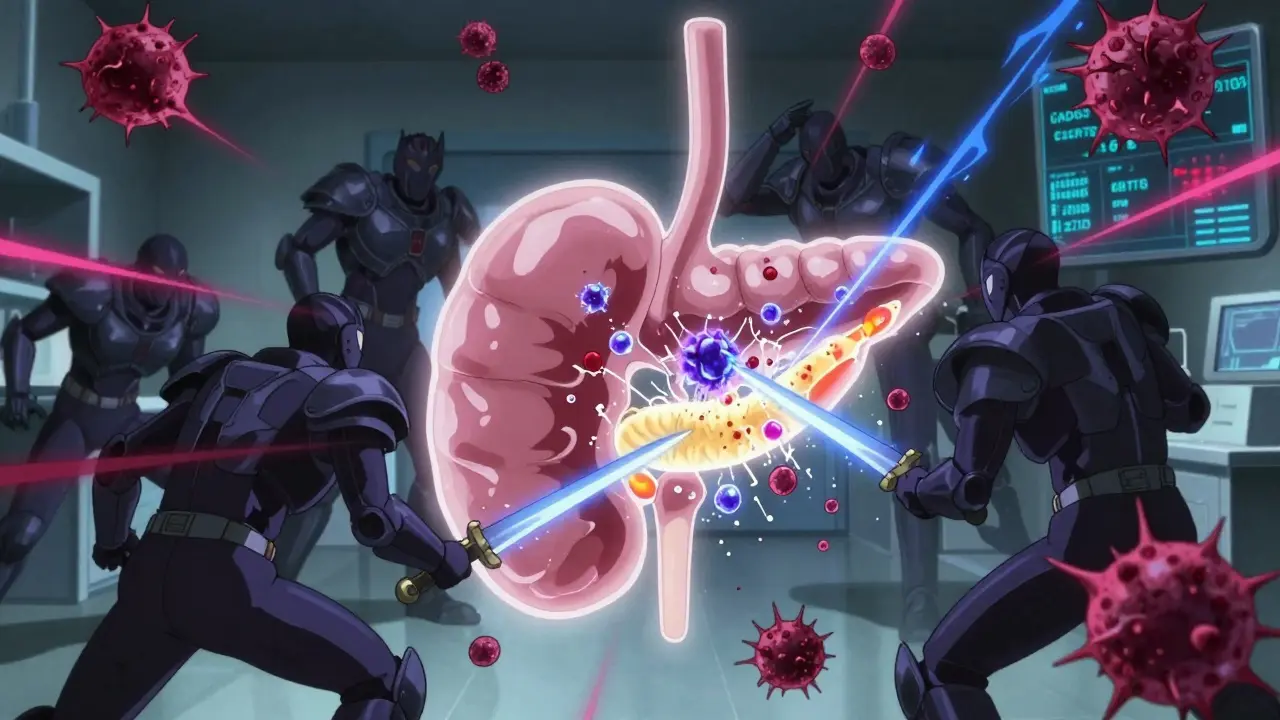
When your immune system turns against your own pancreas, life changes overnight. Type 1 diabetes isn’t just about high blood sugar-it’s the result of your body’s T cells attacking and destroying the insulin-producing beta cells in your pancreas. This isn’t a mistake. It’s an autoimmune war happening inside you, and it starts long before you ever feel sick. By the time someone is diagnosed, they’ve already lost 80-90% of their insulin-making capacity. What’s left isn’t enough to keep blood sugar stable, even with perfect diet and exercise. That’s why managing type 1 diabetes isn’t about fixing a bad habit-it’s about replacing what your body can no longer make.
The Autoimmune Attack on the Pancreas
Type 1 diabetes isn’t caused by eating too much sugar or being overweight. It’s caused by your immune system mistaking your pancreatic beta cells for invaders. These cells sit in clusters called islets, and they’re the only ones in your body that produce insulin. When they’re gone, insulin disappears too. The process doesn’t happen overnight. It begins years before symptoms show up. Researchers call this the silent phase. In this stage, autoantibodies-tiny markers of immune attack-start appearing in the blood. These target proteins like GAD65, IA-2, ZnT8, and even insulin itself. Finding two or more of these autoantibodies means you’re in Stage 1 of type 1 diabetes, even if your blood sugar is still normal.The immune attack isn’t random. Genetics play a big role. People with HLA-DR3 or HLA-DR4 gene variants are 20 to 30 times more likely to develop type 1 diabetes. But genes alone don’t cause it. Something has to trigger the immune system. Viruses like coxsackievirus B are strong suspects. Studies show people who develop type 1 diabetes often had recent enterovirus infections months before diagnosis. Environmental factors like early diet, vitamin D levels, and gut bacteria also influence risk. One 2022 study found that people with type 1 diabetes had significantly lower levels of Faecalibacterium prausnitzii, a gut bacterium that helps reduce inflammation. When that bug is missing, the immune system may become more aggressive.
Stages of Type 1 Diabetes: From Silent to Crisis
The progression of type 1 diabetes follows three clear stages, defined by the TrialNet consortium:- Stage 1: Two or more autoantibodies present, normal blood sugar. No symptoms. About 0.4% of the general population is here.
- Stage 2: Autoantibodies + abnormal blood sugar (dysglycemia), still no symptoms. This stage affects about 0.15% of people. The pancreas is losing ground fast.
- Stage 3: Symptoms appear-excessive thirst, weight loss, fatigue-and insulin therapy becomes necessary. This is the classic diagnosis most people know.
Children tend to move through these stages quickly-often within 3 years of the first autoantibody. Adults, especially those with LADA (Latent Autoimmune Diabetes in Adults), can take over a decade. That’s why many adults are misdiagnosed with type 2 diabetes at first. In fact, 12% of adults newly diagnosed with type 1 were initially told they had type 2. That mistake leads to dangerous delays in insulin therapy. Without insulin, the body starts breaking down fat for energy, leading to diabetic ketoacidosis (DKA). DKA happens in 20-30% of children at diagnosis and can be fatal if not treated immediately with IV insulin and fluids.
Managing the Aftermath: Insulin, Monitoring, and Technology
Once beta cells are destroyed, insulin must come from outside. There’s no cure yet, but modern tools make life manageable. The American Diabetes Association recommends multiple daily injections (MDI) or insulin pump therapy. Most people use rapid-acting insulin (like insulin aspart or lispro) before meals and long-acting insulin (like glargine U-300) for background needs. The starting dose? About 0.5 units per kilogram of body weight per day, split evenly between basal and bolus.But insulin alone isn’t enough. You need to know what your blood sugar is doing, all day, every day. That’s where continuous glucose monitors (CGMs) come in. Devices like the Dexcom G7 (approved in 2022) send readings every 5 minutes to your phone. Studies show people using CGMs reduce their HbA1c by 0.4-0.6% and cut hypoglycemic episodes by 40-50%. That’s not a small gain-it’s the difference between constant fear and real freedom.
Even better? Closed-loop systems, or “artificial pancreases.” Tandem’s Control-IQ and Medtronic’s 780G automatically adjust insulin based on real-time glucose data. In 2022, a JAMA study found these systems kept users in target range (70-180 mg/dL) 71-74% of the time. For people on multiple daily injections? Only 51-55%. For kids and teens, the results are even more striking: 78.5% using automated delivery systems hit over 70% time-in-range, compared to just 29.3% on traditional methods.
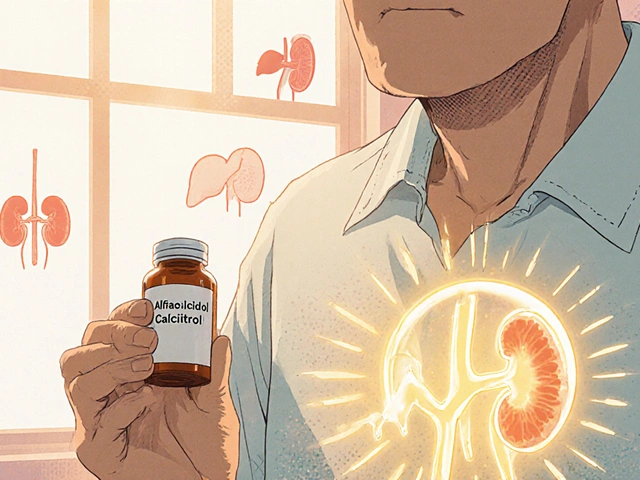
The Rare Overlap: Autoimmune Pancreatitis and Type 1 Diabetes
Most people think type 1 diabetes only affects the endocrine pancreas-the part that makes insulin. But in rare cases, the immune system also attacks the exocrine pancreas-the part that makes digestive enzymes. This is called autoimmune pancreatitis (AIP). It’s not common-only about 1 in 300 people with type 1 diabetes develop it-but when it happens, it changes everything.AIP has two types. Type 1 is linked to high levels of IgG4 antibodies and often affects other organs like the liver or salivary glands. Type 2 is tied to inflammatory bowel disease. Both cause swelling, pain, and poor digestion. If you have type 1 diabetes and suddenly develop belly pain, weight loss, or greasy stools, your doctor should check for AIP. Diagnosis requires imaging, blood tests for IgG4, and sometimes a biopsy.
Here’s the catch: steroids, the main treatment for AIP, spike blood sugar. So if you’re on insulin and get diagnosed with AIP, your insulin dose might need to double temporarily. Once the inflammation clears, you may need to dial it back. That’s why managing both conditions requires close teamwork between an endocrinologist and a gastroenterologist. The American Diabetes Association now recommends checking for pancreatic enzyme deficiency in anyone with long-standing type 1 diabetes who has ongoing digestive issues. About 5-10% of these patients need enzyme replacement pills with meals.
New Hope: Disease-Modifying Therapies
For decades, treatment meant only insulin. Now, that’s changing. In November 2022, the FDA approved teplizumab (brand name Tzield)-the first drug that can delay the onset of type 1 diabetes. It’s not a cure. But in the PROTECT trial, it delayed diagnosis by nearly 2.5 years in people with Stage 2 diabetes. That’s two and a half years without insulin injections, without finger pricks, without fear of DKA.Teplizumab works by targeting specific immune cells that attack beta cells. It’s given as a 14-day IV infusion. It’s not for everyone-it’s only approved for people 8 years and older with Stage 2 diabetes and two or more autoantibodies. But it’s a breakthrough. It proves the immune system can be gently redirected before total destruction.
Other promising therapies are in the pipeline. Verapamil, a blood pressure drug, showed in a 2022 trial that it preserved 30% more insulin production over a year in newly diagnosed patients. Stem cell therapy is even more exciting. Vertex Pharmaceuticals’ VX-880 trial replaced destroyed beta cells with lab-grown ones. In a small group of 12 people, 89% became insulin-free within 90 days. One patient even stopped insulin after 18 months. These aren’t science fiction-they’re happening now.
Researchers are also testing drugs like abatacept, which blocks immune signals. In a 2023 study, it slowed beta cell loss by 59% over two years. The future isn’t just insulin. It’s immunotherapy + beta cell support.
What This Means for Daily Life
Managing type 1 diabetes today isn’t about perfection. It’s about progress. You don’t need to hit a 6.5% HbA1c every single month. You need to stay out of the hospital. You need to avoid lows that knock you out. You need to sleep without checking your glucose. That’s what modern tools deliver.For parents of newly diagnosed kids: start with CGM and an insulin pump if you can. Don’t wait. The first year is the hardest, but technology makes it survivable. For adults diagnosed later: get tested for autoantibodies if you were misdiagnosed as type 2. You might be eligible for teplizumab if you’re still producing some insulin.
And if you’re reading this because you or someone you love has type 1 diabetes-know this: you’re not alone. More than 1.25 million Americans live with it. And for the first time in history, we’re not just managing the symptoms. We’re starting to stop the disease itself.
Is type 1 diabetes the same as autoimmune pancreatitis?
No. Type 1 diabetes attacks the insulin-producing beta cells in the pancreas (endocrine function). Autoimmune pancreatitis attacks the enzyme-producing cells (exocrine function). They’re different parts of the same organ, but different diseases. However, in rare cases (about 1 in 300), both can happen together, requiring treatment for both conditions.
Can type 1 diabetes be reversed?
Not yet. But it can be delayed. Teplizumab can postpone diagnosis by over two years in people with early-stage disease. Stem cell therapies have restored insulin production in some patients, but they’re still experimental. For now, insulin remains essential-but the goal is no longer just survival. It’s preventing the disease before it starts.
Why do some people with type 1 diabetes still make some insulin?
Even after diagnosis, some people retain a small number of beta cells that keep making trace amounts of insulin. This is called residual beta-cell function. It’s more common in adults and those diagnosed later. These people often have fewer lows and better blood sugar control. Drugs like verapamil and teplizumab aim to protect these remaining cells.
Are insulin pumps better than injections?
For most people, yes. Pumps allow more precise dosing and can be linked to CGMs for automated adjustments. Studies show users spend more time in target blood sugar range and have fewer severe lows. But pumps aren’t required. Many people manage well with multiple daily injections, especially if they use CGMs and insulin calculators.
What’s the best way to prevent complications from type 1 diabetes?
Keep your HbA1c below 7% (or as close as safely possible), use a CGM, check for eye and kidney problems yearly, and control blood pressure and cholesterol. But the biggest factor? Avoiding extreme highs and lows. That’s why time-in-range (70-180 mg/dL) is now a better goal than HbA1c alone. Technology makes this achievable.




Kristen Russell
31 December, 2025 15:46 PMJust got diagnosed last month and this post made me feel less alone. CGM saved my life already.
Lee M
2 January, 2026 09:45 AMThey say it's autoimmune but nobody talks about the glyphosate. Big Pharma knows the truth and they're silencing the research. Your pancreas isn't failing-it's being poisoned by the food system. Wake up.
Bryan Anderson
2 January, 2026 23:57 PMThis is an incredibly well-researched and thoughtful breakdown. I especially appreciate the clarity around the three stages-it’s something I wish more clinicians explained to newly diagnosed patients. The data on teplizumab is genuinely hopeful.
Matthew Hekmatniaz
3 January, 2026 03:21 AMAs someone who grew up in a country where insulin was rationed, I’m in awe of how far we’ve come. But let’s not forget the global inequality here-most people with T1D still can’t access CGMs or pumps. Progress is real, but it’s not universal.
Liam George
3 January, 2026 20:57 PMTeplizumab? Sounds like a controlled release vaccine. Did you know the CDC has been quietly tracking autoantibody spikes since 2015? The timing matches the rollout of mRNA tech. Coincidence? Or is this engineered? The pancreas is the body’s control center-why target it? Look at the patents.
Richard Thomas
4 January, 2026 13:34 PMThere’s something deeply metaphysical about losing a part of yourself that you never knew was there until it was gone. The beta cells didn’t just die-they were erased by an internal war you didn’t ask for. And now you’re left with this mechanical replacement, this constant negotiation between numbers and survival. It’s not just medicine. It’s a new kind of existence. You become a hybrid: part human, part machine, constantly recalibrating your soul against a meter. And yet-there’s grace in it. In the quiet moments before dawn, when the CGM beeps softly and you know you’re still here, still fighting-that’s when you realize you’re not just managing a disease. You’re learning how to live with a ghost that never left.
Paul Ong
6 January, 2026 02:52 AMInsulin pumps are life changing no cap CGMs are the real MVP stop waiting start using tech
Olukayode Oguntulu
6 January, 2026 09:28 AMTypical Western medical reductionism. You speak of autoantibodies and glucose meters as if they are the totality of truth. In Ayurveda, we call this Vata imbalance-disturbance of the vital air. The pancreas is a mirror of suppressed emotion. You do not cure T1D with machines. You cure it with silence, with fasting, with the breath. Your insulin is a bandage on a bullet wound.
jaspreet sandhu
7 January, 2026 07:28 AMEveryone is obsessed with technology but nobody talks about the real problem-why are kids getting this at age 5 now? When I was a boy in Punjab, no one had T1D. Now it's everywhere. It's the processed food, the GMOs, the sugar in everything. Your body isn't broken. You're just eating poison. Stop buying into the insulin industry. Go back to real food.
Alex Warden
7 January, 2026 07:57 AMTeplizumab is a scam. The FDA is just giving out drugs to keep people dependent. We don’t need fancy biologics-we need real American solutions like better diet and more exercise. This is what happens when you let foreign labs run medicine.
LIZETH DE PACHECO
9 January, 2026 02:37 AMMy daughter was diagnosed at 7. We started CGM and pump right away. The difference in her mood, her energy, her confidence-it’s not just numbers. It’s her life. You can do this. You’re not alone.
Heather Josey
10 January, 2026 12:58 PMThank you for including the nuance around autoimmune pancreatitis. I was misdiagnosed with type 2 for three years and only discovered I had T1D after developing chronic pancreatitis. The overlap is rarely discussed, and it’s critical for clinicians to screen for both.
Donna Peplinskie
10 January, 2026 13:39 PMThis is so beautifully written-and so needed. I’ve been living with T1D for 28 years, and I still cry when I read something that captures the emotional weight of it. The fear, the fatigue, the quiet triumphs… you named them all. Thank you.
sharad vyas
11 January, 2026 18:16 PMIn India, we don’t have access to most of this. But I’ve seen children with T1D walking miles for insulin. Technology is great, but what we need most is dignity. Not just pumps and CGMs-just enough insulin to live. That’s the real breakthrough.