Diabetes Medication & Alcohol Safety Risk Calculator
When you mix Alcohol a depressant that the liver processes before glucose with diabetes medications drugs used to lower blood sugar, such as insulin, metformin, and sulfonylureas, you create a perfect storm for hypoglycemia and liver stress.
Why the Combination Is a Red Flag
The liver has a dual job: it cleanses toxins like alcohol and it stores or releases glucose to keep blood sugar stable. When alcohol is present, the liver prioritizes breaking it down, temporarily ignoring its glucose‑regulating duties. That short‑circuit can send blood sugar plummeting, especially if you’re on insulin or a sulfonylurea that already pushes glucose down.
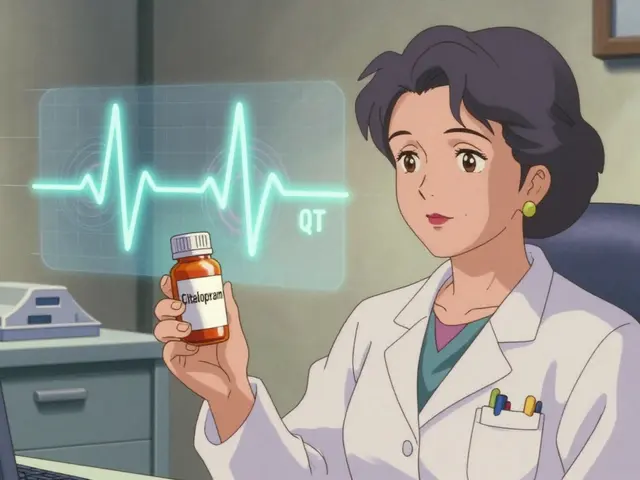
In addition, many diabetes drugs are processed by the same liver enzymes that break down alcohol-CYP2E1, CYP3A4, and CYP1A2. When both compete for these enzymes, the drug’s strength can change, sometimes amplifying side‑effects or leaving the medication less effective.
How Alcohol Triggers Hypoglycemia
Hypoglycemia is the biggest concern flagged by the American Diabetes Association (ADA). The sequence looks like this:
- Alcohol enters the bloodstream and reaches the liver.
- The liver converts alcohol into acetaldehyde, then acetate, using NAD⁺.
- While busy, the liver slows gluconeogenesis-the creation of new glucose.
- Blood glucose drops, sometimes hours after the last drink.
Symptoms-dizziness, slurred speech, confusion-can look a lot like intoxication, making it hard to know which treatment to give. If you mistake low blood sugar for drunkenness, you might delay the glucose rescue and end up in an emergency.
Medications Most Prone to Dangerous Drops
Not all diabetes drugs carry the same hypoglycemia risk. Below is a quick glance at the most common classes.
| Medication | Primary Mechanism | Hypoglycemia Risk with Alcohol | Key Liver Interaction |
|---|---|---|---|
| Insulin | Direct glucose replacement | High - alcohol blocks gluconeogenesis | None (insulin is not metabolized by liver enzymes) |
| Sulfonylureas (e.g., glipizide) | Stimulate pancreatic insulin release | High - additive insulin surge | Metabolized by CYP2C9; alcohol can inhibit clearance |
| Metformin | Reduces hepatic glucose production | Moderate - both lower hepatic output | Both use OCT1 transport; alcohol can worsen GI side effects |
| GLP‑1 agonists (e.g., liraglutide) | Enhance insulin, suppress glucagon | Low to moderate | Minimal hepatic metabolism; low interaction risk |
| SGLT2 inhibitors (e.g., empagliflozin) | Increase urinary glucose excretion | Low - risk mainly dehydration | Primarily renal clearance; alcohol may affect kidneys |
For people on insulin or sulfonylureas, even a single glass of wine on an empty stomach can push glucose below 70 mg/dL. Metformin users often notice amplified stomach upset if they binge drink.
Liver Health Matters
The liver isn’t just a processing plant; it’s a vital regulator of metabolism. Chronic alcohol use can lead to hepatitis, fatty liver, and cirrhosis-all of which impair the organ’s ability to release glucose when needed.
Studies cited by Medical News Today show that moderate drinking (2‑3 drinks per day) already raises liver enzyme levels in many diabetics. When you add a medication that also stresses the liver, the combined effect can accelerate damage.
Enzyme competition is another hidden danger. Alcohol induces CYP2E1, which can speed up the breakdown of some drugs, lowering their efficacy. Conversely, certain drugs can inhibit alcohol metabolism, increasing blood alcohol concentration and prolonging intoxication.
Practical Tips to Keep Sugar Stable
Here’s a straightforward checklist you can start using tonight:
- Check your blood glucose before you start drinking. Aim for >100 mg/dL.
- Never drink on an empty stomach. Pair each alcoholic drink with a snack containing 15‑30 g of carbs (e.g., crackers, fruit, a granola bar).
- Limit yourself to one drink per hour and keep total consumption under the “moderate” threshold (up to 1 drink/day for women, 2 for men).
- Set a timer to test glucose every 1‑2 hours while you’re drinking and again before bedtime.
- Carry fast‑acting glucose (glucose tablets, juice) and know the 15‑15 rule: 15 g carbs, re‑check after 15 minutes.
- If you use a pump or basal insulin, consider lowering the dose by 10‑20 % on drinking nights.
- Wear medical ID that lists your diabetes and medication regimen.
These steps address both the immediate hypoglycemia threat and the longer‑term liver load.

Monitoring Tech: From CGM to Smart Apps
Continuous glucose monitors (CGM) like the Dexcom G7 and Abbott FreeStyle Libre 3 now flag rapid glucose drops, which often coincide with alcohol intake. While they don’t detect alcohol directly, their trend alerts give you a heads‑up before you feel any symptoms.
Some newer apps let you log drinks alongside glucose readings, creating a personal pattern map. Over time, the software can suggest safe drinking windows based on your historic data.
When to Seek Professional Guidance
The ADA recommends a personalized discussion with your healthcare provider. Bring a list of:
- Your current medication list (including doses).
- Typical drinking habits (type of alcohol, amount, frequency).
- Recent liver function test results, if available.
Your doctor may adjust medication timing, suggest a lower‑dose sulfonylurea, or switch you to a class with less hypoglycemia risk if you plan to drink regularly.
Key Takeaway
Alcohol and diabetes medications create a risky mix that can trigger low blood sugar and strain the liver. Understanding how the liver processes both substances, knowing which drugs pose the biggest danger, and following a simple safety routine can keep you enjoying a glass responsibly.
Can I have a glass of wine while on metformin?
Yes, but keep it to one small glass (about 5 oz) and pair it with a carbohydrate‑rich snack. Metformin already reduces liver glucose output, so drinking can amplify the effect and worsen stomach upset.
Why does hypoglycemia sometimes happen hours after I stop drinking?
After alcohol is absorbed, the liver stays busy converting it for several hours. During that time, gluconeogenesis stays suppressed, so blood sugar can keep falling even if you’ve stopped drinking.
Is it safer to use insulin pens instead of a pump when I drink?
Both delivery methods carry the same hypoglycemia risk because the insulin dose is the same. However, a pump allows quick basal adjustments, which can be handy if you anticipate a drop.
What liver tests should I ask my doctor for?
Typical panels include ALT, AST, GGT, and bilirubin. Elevated levels may signal that alcohol is already stressing your liver, prompting medication tweaks.
Do SGLT2 inhibitors interact with alcohol?
Interaction is low, but alcohol can increase dehydration, which may boost the risk of urinary tract infections linked to SGLT2 drugs.





Grace Silver
24 October, 2025 22:18 PMMixing alcohol with insulin or sulfonylureas creates a rapid drop in blood sugar because the liver busy breaking down ethanol. When the liver is preoccupied the body can’t release enough glucose and your meds are already pushing insulin levels up. Even a single cocktail on an empty stomach can push numbers below 70 mg/dL within an hour. The key is to keep a carb snack handy and check your glucose before the first sip. Treat the drink like a stress test for your metabolism and you’ll stay safer.
Tamara Schäfer
26 October, 2025 02:04 AMConsidering the liver as a negotiator between alcohol and glucose can help you visualize the risk in a more concrete way. The body’s ability to shift gears depends on having enough glycogen stores, so a light snack before drinking acts like a buffer. If you notice a dip, a quick bite of fruit can reset the balance without overcompensating. Stay mindful of timing – a half‑hour after a drink is often when gluconeogenesis starts to recover. Keep experimenting safely and you’ll find a routine that feels relevent to your lifestyle.
Max Lilleyman
27 October, 2025 04:51 AMAlcohol will blunt the liver’s glucose output and any sulfonylurea dose on top of that is a recipe for danger 🚨. The combo can drop you into hypoglycemia faster than you realize, especially after a night out. Keep a glucose tablet in your pocket and don’t rely on feeling “tipsy” to gauge your level. Your device’s CGM alerts can save you from a scary episode 😬. Treat it like a safety net, not an optional extra.
Brett Witcher
28 October, 2025 08:38 AMWhile the anecdotal warnings are salient, a rigorous pharmacokinetic analysis reveals that ethanol induces CYP2E1, thereby accelerating the metabolism of certain sulfonylureas. Consequently, plasma concentrations may fluctuate, yielding unpredictable glycemic excursions. It is advisable to schedule alcohol consumption at least 24 hours apart from the peak plasma window of these agents. Additionally, the hepatic first‑pass effect may variably attenuate insulin clearance, further compounding risk. Such considerations underscore the necessity of individualized therapeutic planning.
Benjamin Sequeira benavente
29 October, 2025 12:24 PMCut the booze when you’re on insulin and you’ll never drop low again.
Shannon Stoneburgh
30 October, 2025 16:11 PMThat advice ignores the reality that many people enjoy drinks socially and need practical tips, not an all‑or‑nothing rule.
Nathan Comstock
31 October, 2025 19:58 PMOur Great American tradition of responsible drinking gets lost when we ignore the science that alcohol hijacks the liver’s glucose engine, leaving us vulnerable to the very same health crises that undermine our nation’s vitality.
Terell Moore
1 November, 2025 23:44 PMAh yes, because the solution to liver‑mediated hypoglycemia is clearly to banish every glass of wine from the American palate, as if cultural nuance ever factored into metabolic pathways. One might instead consider calibrated dosing and timed meals, but that would demand the unpleasant effort of personal responsibility.
Amber Lintner
3 November, 2025 03:31 AMIf you think a single glass of wine will ruin your glucose control, you’re buying into fear‑mongering; the data shows moderate consumption can be accommodated with minor adjustments.
Olivia Harrison
4 November, 2025 07:18 AMIt’s true that a modest amount of wine isn’t automatically disastrous. Pair it with a balanced snack, keep your CGM alert on, and re‑check your level before bedtime. Those steps let you enjoy social moments while staying within safe glycemic ranges.
Corrine Johnson
5 November, 2025 11:04 AMIndeed-one must acknowledge!!! The interplay between ethanol metabolism and insulin dynamics is not a trivial footnote!!! It demands rigorous scrutiny!!! Oversimplified warnings do a disservice to both clinicians and patients!!!
Jennifer Stubbs
6 November, 2025 14:51 PMWhile the emphatic tone highlights urgency, a balanced risk assessment should weigh frequency of drinking, dosage of medication, and individual hepatic function. Meta‑analyses suggest that occasional moderate alcohol does not significantly increase severe hypoglycemia rates in patients with stable CGM monitoring. Therefore, personalized education supersedes blanket prohibitions.
Abhinav B.
7 November, 2025 18:38 PMIn many South Asian families, a small amount of sharab after dinner is part of celebration, yet we often overlook how our genetic predisposition to enzyme variations can alter alcohol processing. The CYP2E1 enzyme, for example, shows polymorphisms that may make some individuals more susceptible to liver stress when combined with metformin. When you add a sulfonylurea to the mix, the risk of a sudden sugar crash can be amplified beyond what textbooks predict. I have seen patients who thought a single beer was harmless, only to wake up with dizziness and a glucose reading below 60. Their doctors missed the chance to ask about drinking habits during routine visits. A simple questionnaire about weekly alcohol intake can flag those who need dose adjustments. Moreover, cultural stigma around admitting drinking can lead to under‑reporting, so clinicians must create a non‑judgmental environment. Education should include the timing of meals, because a carbohydrate‑rich snack can act as a safety net. It is also wise to schedule CK‑monitoring labs after periods of increased social drinking to catch early signs of hepatic strain. Even if your liver enzymes are within normal limits, chronic low‑grade inflammation may still be present. The interplay between diet, medication, and alcohol is a triad that deserves a holistic view. Practical steps include lowering basal insulin by a modest percent on nights you plan to drink, and keeping rapid‑acting glucose sources within reach. If you use a CGM, set a custom alert for a rapid drop that often coincides with alcohol ingestion. Finally, involve your family in the conversation; shared responsibility reduces the chance of an accidental hypoglycemic event. By respecting both cultural traditions and medical science, you can enjoy a toast without compromising health.