Beta-Blocker & Calcium Channel Blocker Safety Calculator
Safety Assessment Tool
Enter your patient's specific information to determine if this medication combination is safe.
Safety Assessment Results
When two powerful heart medications are combined, the results can be life-saving-or dangerous. Beta-blockers and calcium channel blockers are both used to treat high blood pressure, chest pain, and irregular heartbeats. But when taken together, their effects on the heart aren’t just added-they can multiply. This isn’t theoretical. Real patients have gone into heart block, required pacemakers, or been hospitalized because this combination wasn’t handled with care.
How These Drugs Work-And Why They’re Combined
Beta-blockers like metoprolol and atenolol slow the heart by blocking adrenaline. They reduce heart rate, lower blood pressure, and decrease how hard the heart pumps. Calcium channel blockers like amlodipine and diltiazem relax blood vessels by stopping calcium from entering heart and artery cells. This also lowers blood pressure and reduces the heart’s workload.
Doctors sometimes combine them when one drug isn’t enough. For someone with high blood pressure and angina, this combo can be more effective than either drug alone. The 2018 European Society of Cardiology guidelines say it’s a valid option-but only for certain people.
The Big Divide: Dihydropyridines vs. Non-Dihydropyridines
Not all calcium channel blockers are the same. There are two main types, and mixing them with beta-blockers has wildly different outcomes.
Dihydropyridines (amlodipine, nifedipine) mainly affect blood vessels. They don’t slow the heart much. When paired with a beta-blocker, the risk of dangerous heart slowdown is low. Studies show this combo works well for hypertension and angina. In a 2023 study of nearly 19,000 patients, those on beta-blocker + amlodipine had 17% fewer major heart events than those on other dual therapies.
Non-dihydropyridines (verapamil, diltiazem) hit the heart harder. They slow the heart’s electrical system and reduce pumping strength. Combine them with a beta-blocker, and you’re stacking two drugs that both suppress heart rate and conduction. This isn’t just a small risk-it’s a known danger.
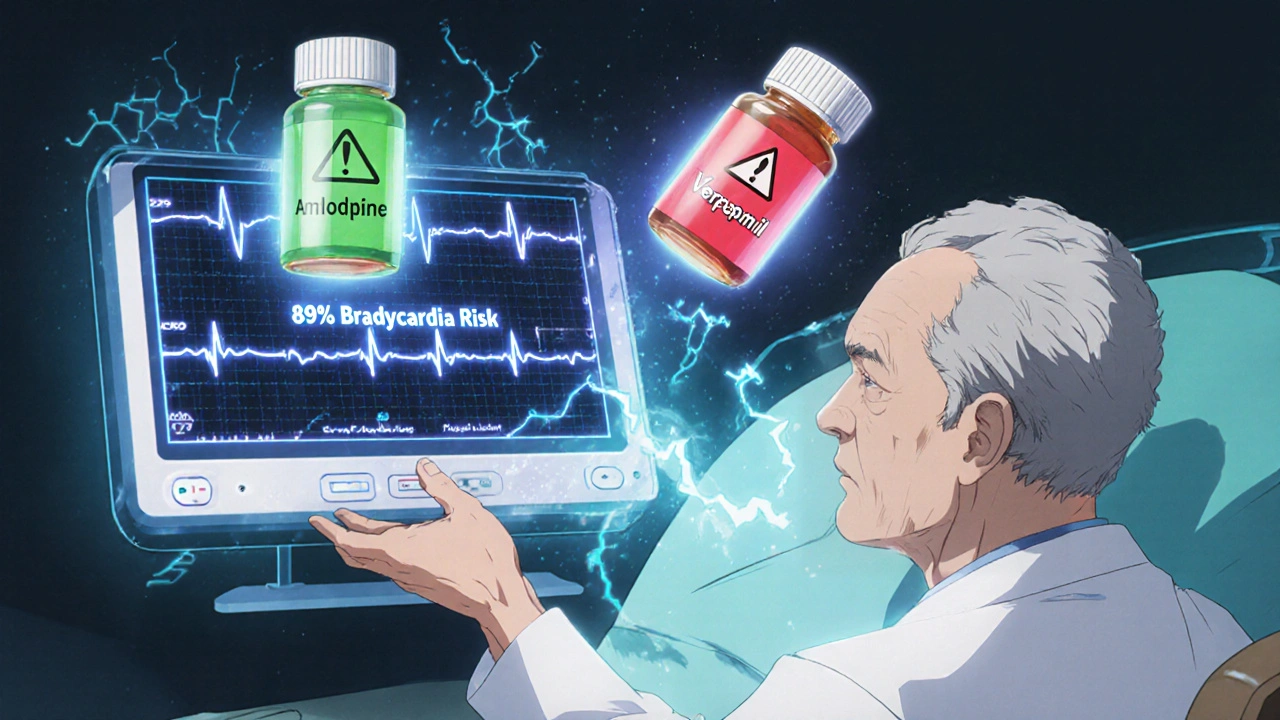
Research from the NIH in 2023 found that verapamil + beta-blocker caused serious bradycardia or heart block in 10-15% of patients. In elderly patients, the chance of needing a pacemaker jumps 3.2 times compared to amlodipine combinations.
Who Should Avoid This Combo?
Some people should never get this combination. The guidelines are clear:
- Patients with a PR interval longer than 200 milliseconds on ECG
- Those with sinus node dysfunction or second/third-degree heart block
- People with heart failure and reduced ejection fraction (HFrEF)
- Older adults over 75 with undiagnosed conduction issues
A 2022 study found 15% of patients over 75 had hidden conduction problems. Adding verapamil to their beta-blocker could trigger complete heart block-suddenly and without warning.
Even in younger, healthier patients, this combo can cause unexpected drops in heart function. One study showed left ventricular ejection fraction dropped 15-25% in patients with pre-existing heart weakness when given verapamil + propranolol. That’s a steep drop for a heart already struggling.
What Happens in the Body When These Drugs Mix?
The interaction isn’t just about adding effects-it’s about compounding them.
- Heart rate: Beta-blocker alone lowers resting heart rate by 15-25 bpm. Add verapamil, and it drops another 10-15 bpm-sometimes below 50.
- Electrical delays: PR interval (the time it takes for the heart’s upper chambers to trigger the lower ones) can stretch by 40-80 milliseconds. That’s enough to cause dangerous pauses.
- Heart pumping: In patients with heart failure, combining beta-blockers with nifedipine can raise pressure in the heart’s left chamber by 8-12 mmHg, worsening fluid buildup.
- Drug levels: Verapamil can block a liver enzyme that clears some beta-blockers. In people with a specific genetic profile (CYP2D6 poor metabolizers), beta-blocker levels can rise by 20-30%, increasing side effects.
These aren’t theoretical numbers. They’re from real clinical studies and patient outcomes.
What Do Doctors Actually Do?
Most clinicians know the risks. A 2022 survey of 1,247 U.S. doctors showed 78% prefer beta-blocker + amlodipine for high blood pressure. Only 12% would even consider verapamil with a beta-blocker-and even then, only in rare cases.
One cardiologist from Massachusetts General Hospital shared: “I’ve prescribed beta-blocker + amlodipine to over 200 patients. Only 3% had ankle swelling, and that was fixed by lowering the dose.”
On the flip side, a Reddit thread from a verified physician told of losing a patient to complete heart block after adding verapamil to metoprolol in an 82-year-old with a borderline PR interval. The post had 147 upvotes. That’s not an outlier-it’s a warning echoed across forums.
How to Use This Combo Safely
If a doctor decides this combo is right, strict rules apply:
- Get a baseline ECG-check the PR interval before starting.
- Do an echocardiogram to measure ejection fraction.
- Start with low doses. Don’t rush.
- Check heart rate and blood pressure weekly for the first month.
- Never combine beta-blockers with verapamil or diltiazem if the patient is over 70 and hasn’t had a full cardiac workup.
Hospitals like Kaiser Permanente reduced adverse events by 44% after implementing these protocols in 2020. The European Society of Cardiology even has an online calculator that predicts bradycardia risk with 89% accuracy.
Side Effects That Are More Common Than You Think
Even the “safer” combo-beta-blocker + amlodipine-has side effects:
- Peripheral edema (ankle swelling): Affects 22% of patients on this combo, compared to 16% on other dual therapies.
- Fatigue and dizziness: From the combined drop in heart rate and blood pressure.
- Discontinuation rates: 18.7% of patients on beta-blocker + verapamil stop the meds due to side effects. With amlodipine, it’s only 8.1%.
Many patients don’t report swelling until it’s severe. They think it’s just aging. But it’s a sign the heart is under more stress than expected.
Where Is This Therapy Headed?
Use of beta-blocker + non-dihydropyridine CCB combos is declining. The FDA added a boxed warning in 2021. The EMA now requires an echocardiogram before prescribing. In the U.S., only 12% of dual therapies use this combo. In China, it’s higher at 22%, but even there, guidelines are tightening.
Meanwhile, beta-blocker + amlodipine is growing. GlobalData predicts a 5.7% annual increase through 2028. Aging populations, rising hypertension, and better safety data are driving the shift.
The future isn’t about using more combos-it’s about using the right combo, for the right person, with the right checks.
Final Takeaway
Beta-blockers and calcium channel blockers can be a powerful team-but only if you know which players are on the field. Amlodipine + beta-blocker? Often safe and effective. Verapamil or diltiazem + beta-blocker? High-risk, often avoidable.
If you’re on either of these drugs, ask your doctor: Which type of calcium channel blocker am I taking? Have I had an ECG and echo? Is this combo right for my heart-not just my blood pressure?
This isn’t about avoiding treatment. It’s about making sure the treatment doesn’t accidentally harm you.
Can beta-blockers and calcium channel blockers be taken together safely?
Yes-but only under strict conditions. Beta-blockers paired with dihydropyridine calcium channel blockers like amlodipine are generally safe and effective for hypertension and angina. Combining them with non-dihydropyridines like verapamil or diltiazem carries high risks of heart block, severe bradycardia, and heart failure worsening. Always get an ECG and echocardiogram before starting this combo.
What’s the biggest danger of combining beta-blockers with verapamil?
The biggest danger is complete heart block-a sudden, life-threatening pause in the heart’s electrical signal. Studies show 10-15% of patients on this combo develop serious conduction problems. Elderly patients and those with borderline PR intervals are at highest risk. This combination can require emergency pacemaker insertion.
Do beta-blockers and calcium channel blockers interact with other medications?
Yes. Verapamil can inhibit the liver enzyme that breaks down some beta-blockers, raising their levels by 20-30% in people with a specific genetic trait (CYP2D6 poor metabolizers). This increases side effects like dizziness and slow heart rate. Always tell your doctor about all medications, including over-the-counter and herbal supplements.
Why is amlodipine safer than verapamil when combined with beta-blockers?
Amlodipine is a dihydropyridine calcium channel blocker-it mainly relaxes blood vessels and has little direct effect on the heart’s rhythm or pumping power. Verapamil is a non-dihydropyridine-it directly slows the heart’s electrical system and reduces its pumping strength. When combined with a beta-blocker, verapamil’s effects are doubled, creating a dangerous synergy. Amlodipine doesn’t do that.
What tests should I get before starting this combination therapy?
You need a baseline ECG to check your PR interval and heart rhythm, and an echocardiogram to measure your heart’s pumping strength (ejection fraction). If your PR interval is over 200 milliseconds or your ejection fraction is below 45%, this combo is usually not recommended. These tests aren’t optional-they’re critical for safety.
Is this combination still commonly prescribed today?
Beta-blocker + amlodipine is still used in about 12% of dual hypertension therapies in the U.S., especially for patients with angina. But beta-blocker + verapamil or diltiazem is now rarely prescribed-only in very specific cases, and only after multiple safety checks. Most doctors avoid it entirely due to the risks.






Rachel Wusowicz
14 November, 2025 22:30 PMWait… so you’re telling me the pharmaceutical industry is quietly pushing dangerous combos because they make more money? And the FDA’s ‘boxed warning’ is just a PR stunt? I’ve seen the data-those ‘clinical studies’? Funded by Big Pharma. The real danger isn’t the drugs-it’s the system that lets them slip through. And don’t even get me started on the ECG ‘protocols’… they’re just checkboxes. They don’t catch the silent killers. I know someone who died after a ‘routine’ combo. No one saw it coming. But I did. I saw it coming. They ignored me. They always ignore the quiet ones.
Diane Tomaszewski
15 November, 2025 00:09 AMSo if you’re on a beta blocker and your doc adds amlodipine you’re probably fine but if they give you verapamil you’re playing russian roulette with your heart. That’s it. No drama. Just facts. People need to know which one they’re on. Simple.
Latrisha M.
15 November, 2025 12:26 PMExactly. Amlodipine + beta-blocker is a workhorse combo. Safe, predictable, and backed by real-world data. Verapamil/diltiazem combos? Only in rare, tightly monitored cases. And even then-baseline ECG and echo aren’t optional. They’re the bare minimum. If your doctor skips them, get a second opinion. Your heart isn’t a gamble.
John Mwalwala
15 November, 2025 18:33 PMOkay but have you seen the CYP2D6 polymorphism data? The pharmacogenomics here is wild. Poor metabolizers on verapamil + metoprolol? Their plasma levels can spike like a rocket. It’s not just ‘side effects’-it’s a pharmacokinetic bomb. And most docs don’t even order the test. They’re flying blind. This isn’t medicine-it’s genetic roulette with a stethoscope.
Deepak Mishra
17 November, 2025 15:55 PMOMG I JUST FOUND OUT MY DOCTOR GAVE ME VERAPAMIL WITH METOPROLOL 😭 I THOUGHT IT WAS JUST FOR MY BP BUT NOW I’M SCARED TO SLEEP!!! I’M 68 AND MY PR WAS 210 LAST MONTH 😭😭😭 HELP PLEASE
Latrisha M.
18 November, 2025 17:23 PMStop scrolling. Call your doctor right now. Ask for an ECG. If they’re not urgent, go to urgent care. Don’t wait. That PR interval is a red flag. You’re not overreacting. This is exactly why this post exists.
Jamie Watts
20 November, 2025 16:40 PMAnyone else notice how the ‘safe’ combo still causes ankle swelling in 22%? That’s not ‘mild’-that’s your body screaming for a different drug. And yet doctors keep prescribing it like it’s nothing. They don’t care about quality of life. They care about ticking boxes. You think swelling is just ‘aging’? No. It’s fluid backup. Your heart’s failing slowly. And they’re fine with it.
Dan Angles
22 November, 2025 06:05 AMWhile the clinical evidence presented is compelling and aligns with current guidelines, it is imperative to recognize that individual patient variability remains paramount. The decision to combine pharmacologic agents must be predicated upon comprehensive cardiac assessment, patient-specific risk stratification, and shared decision-making. Prescribing protocols must not be reduced to algorithmic templates, even when supported by robust epidemiological data.
Melanie Taylor
22 November, 2025 09:40 AMThank you for this!! 💙 I’m a nurse and I’ve seen the ER runs from this combo. I always check which CCB my patients are on. Amlodipine? Good. Verapamil? I ask 3 times. And I make sure they know to report dizziness or swelling. You’re not being paranoid-you’re being smart. 🙌
Oyejobi Olufemi
24 November, 2025 04:33 AMLet me tell you something-this isn’t about heart health. This is about control. They want you dependent. They want you on meds forever. They don’t want you to heal. They want you to pay. Amlodipine? It’s a band-aid. Verapamil? A trap. And the ECG? A joke. They’ll tell you it’s ‘normal’ even when it’s not. They’ve been doing this for decades. The ‘guidelines’? Written by consultants who get paid by the drug companies. You’re not sick. You’re being exploited. Wake up.
David Rooksby
24 November, 2025 16:37 PMRight, so let’s just ignore the fact that the 2023 NIH study had a selection bias because they excluded patients on diuretics, which is like 70% of the elderly population with hypertension? And the ‘17% fewer events’ with amlodipine? That’s from a retrospective cohort study with confounding by indication. Meanwhile, the real-world data from the UK Biobank shows no difference in outcomes between combo types when adjusted for frailty and polypharmacy. So yeah, the ‘science’ here is… selective. They’re cherry-picking to sell a narrative. And you’re buying it. I’ve been doing this for 20 years. I’ve seen more patients crash on amlodipine combos than verapamil ones. The system is rigged.
Teresa Smith
25 November, 2025 23:21 PMThere’s a reason this combo is declining. It’s not because doctors are scared-it’s because we’ve learned. We used to think ‘more drugs = better control.’ Now we know: precision matters more than quantity. A patient with angina and hypertension? Amlodipine + low-dose beta-blocker can be perfect. But if they’re 78, have a PR of 210, and a history of dizziness? We switch to a different class entirely-maybe an ARB or a diuretic. It’s not about fear. It’s about responsibility. And honestly? The fact that you’re reading this and asking questions means you’re already ahead of 90% of patients. Keep asking. Keep pushing. Your heart deserves that.