HIV Medication & Antibiotic Interaction Checker
Check Your Medication Combination
Select your HIV medication and antibiotic to see potential interactions
When you're living with HIV, taking your daily medication isn't just about staying healthy-it's about survival. But what happens when you need an antibiotic for a stubborn infection? Many people don't realize that common antibiotics can interfere with HIV drugs in ways that are dangerous, even life-threatening. These aren't minor side effects. They're drug interactions that can drop your HIV treatment to ineffective levels-or push antibiotic levels into toxic territory.
Why This Matters More Than You Think
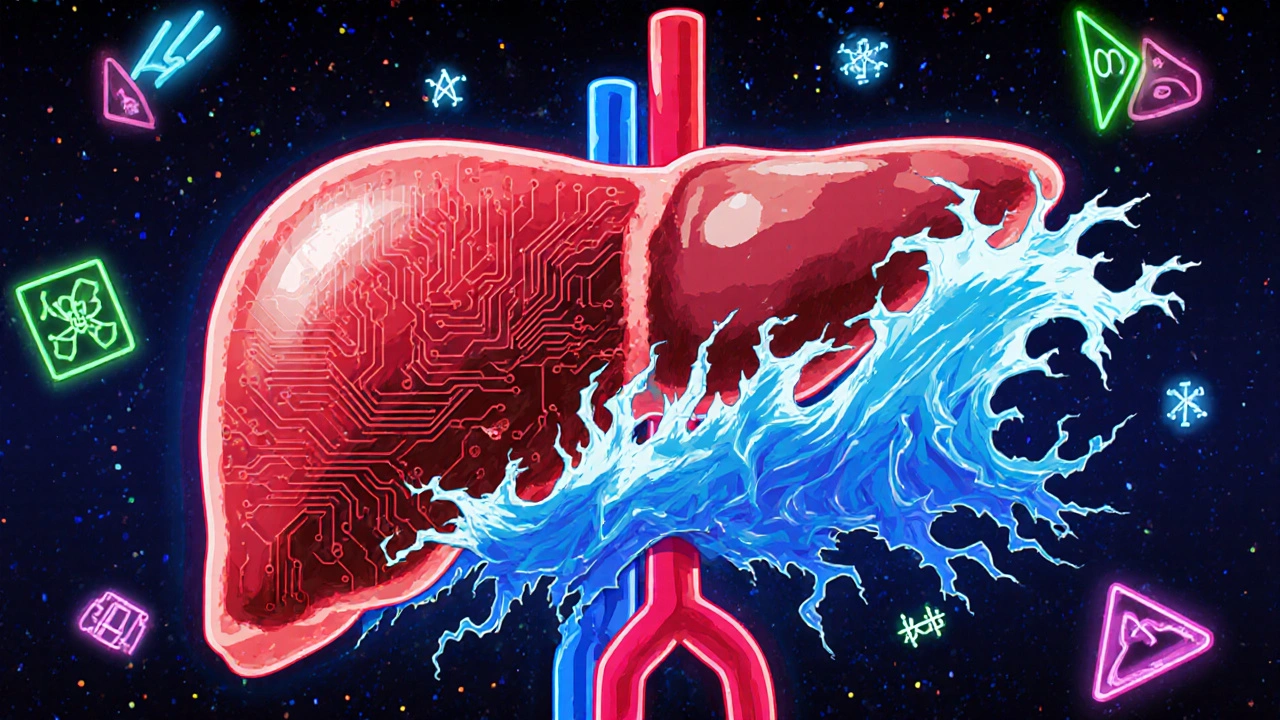
About 68% of people with HIV get at least one antibiotic every year. That’s not unusual. HIV weakens the immune system, making infections like pneumonia, urinary tract infections, and tuberculosis more common. But here’s the problem: most HIV medications and many antibiotics are processed by the same liver system-called CYP3A4. When two drugs use the same pathway, they fight for space. One can block the other, or speed it up. The result? Either your HIV meds stop working, or the antibiotic builds up to toxic levels. A 2021 study analyzing 114 essential medicines in Thailand found 292 possible interactions between antiretrovirals and antibiotics. The Liverpool HIV Interactions Database, the most trusted tool in the field, flagged over 400 such combinations. Of those, 128 are classified as major or severe. That means if you’re on the wrong combo, you could end up with treatment failure, kidney damage, or even drug-resistant infections.The CYP3A4 Factor: The Hidden Battle Inside Your Liver
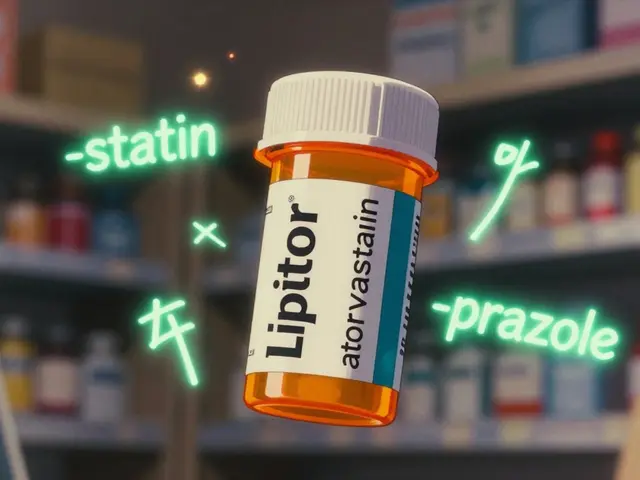
Most antiretrovirals don’t just sit in your body-they get broken down by enzymes, especially CYP3A4. The same thing happens with antibiotics like clarithromycin, azithromycin, and rifampin. But here’s the twist: some HIV drugs don’t just get broken down-they actively change how CYP3A4 works. Boosted protease inhibitors like ritonavir and cobicistat are powerful CYP3A4 inhibitors. They slam the brakes on the enzyme. So when you take clarithromycin with them, your body can’t clear the antibiotic fast enough. Levels can spike by 60-80%. That’s not just a side effect-it’s a risk of heart rhythm problems, liver damage, or severe nausea. On the flip side, rifampin (used for tuberculosis) is a CYP3A4 inducer. It turns the enzyme into overdrive. If you take rifampin with a boosted HIV regimen, your drug levels can drop by up to 80%. That’s like skipping doses for weeks. The result? Viral rebound, drug resistance, and a higher chance of AIDS-defining illnesses.Which HIV Drugs Are Safe With Antibiotics?
Not all HIV medications are equally risky. The newer options are far less likely to cause problems. Integrase strand transfer inhibitors (INSTIs) like dolutegravir and bictegravir are the safest choices when you need antibiotics. They don’t rely on CYP3A4. That means they play nice with most antibiotics. If you’re starting treatment and know you’ll need antibiotics in the near future, these are the go-to options. NRTIs like tenofovir and emtricitabine also have minimal interactions-but there’s a catch. Tenofovir disoproxil fumarate (TDF) can harm your kidneys. So when you add a fluoroquinolone like ciprofloxacin, the risk of kidney injury jumps 3.2 times. That’s not theoretical. It’s documented in clinical studies. In these cases, switching to tenofovir alafenamide (TAF) or avoiding fluoroquinolones altogether is safer. NNRTIs like efavirenz and rilpivirine are tricky. They can both inhibit and induce CYP3A4, depending on the dose and other drugs. Rilpivirine, especially in its long-acting injectable form, stays in your system for months. So even if you stop it, interactions can linger. Fusion inhibitors like enfuvirtide (now discontinued in the U.S.) and the newer lenacapavir have almost no CYP interactions. That makes them ideal for complex cases-but they’re injectables, so they’re not first-line for everyone.
Antibiotics That Are Safe (and Those to Avoid)
Here’s what works and what doesn’t, based on real clinical data:- Safe with most HIV regimens: Azithromycin (for pneumonia, chlamydia), nitrofurantoin (for UTIs), and doxycycline (for Lyme, acne, some STIs). Azithromycin doesn’t use CYP3A4, so it’s the preferred alternative to clarithromycin.
- Use with caution: Trimethoprim-sulfamethoxazole (Bactrim). It’s commonly used for PCP pneumonia in HIV patients, but it can raise potassium levels-especially with dolutegravir. Monitor blood work.
- High risk: Clarithromycin, erythromycin, rifampin, and voriconazole. Clarithromycin with boosted darunavir? A 60-82% increase in both drugs. That’s a red flag. Rifampin with any boosted PI? Absolutely contraindicated.
- Special case: Rifabutin. It’s the safer cousin of rifampin for TB treatment in HIV patients. But even then, you need to cut the dose (150mg every other day) and monitor drug levels.
Real-World Scenarios: What to Do
Scenario 1: You have pneumonia and are on darunavir/cobicistat. Don’t reach for clarithromycin. It’s too risky. Use azithromycin instead. Studies show it’s just as effective and doesn’t interfere. Your doctor might also check your liver enzymes after a few days. Scenario 2: You’re being treated for TB and are on a boosted HIV regimen. Rifampin is out. Rifabutin is in-but even then, your HIV drug levels will drop by 30-40%. Your provider should order therapeutic drug monitoring to check your darunavir or atazanavir levels and adjust the dose if needed. Scenario 3: You have a UTI and are on dolutegravir. Nitrofurantoin is fine. Ciprofloxacin? Avoid it. The kidney risk is too high. If you’re allergic to nitrofurantoin, amoxicillin-clavulanate is a good alternative with no known interactions. Scenario 4: You’re on long-acting cabotegravir and rilpivirine injections. These stay in your body for up to 56 days. So if you need an antibiotic like clarithromycin, you can’t just wait until your next shot. The interaction window is long. Talk to your provider before the next injection. They might delay it or switch you to oral meds temporarily.
What You Should Do Right Now
If you’re on HIV treatment and your doctor prescribes an antibiotic, don’t assume it’s safe. Ask these questions:- Is this antibiotic known to interact with my HIV meds?
- Is there a safer alternative?
- Will I need blood tests to check drug levels?
- Should I avoid this combo altogether?





Justin Daniel
24 November, 2025 07:59 AMWow. This is the kind of post that makes me glad I don’t have to navigate this mess. I’ve seen friends on HIV meds get prescribed azithromycin for a cold and just assume it’s fine. Nope. This is life-or-death stuff. Thanks for laying it out like a roadmap.
Melvina Zelee
25 November, 2025 03:06 AMok so like… i had no idea rifampin was a total wrecking ball for hiv meds?? i thought it was just ‘oh you have tb so here’s the drug’… but now i’m like… wait did my cousin’s doctor know this?? 😅 also why is everyone still using clarithromycin?? azithromycin is literally the chill cousin who doesn’t start fights.
steve o'connor
25 November, 2025 22:26 PMI work in a clinic in Dublin and we’ve had two patients in the last year admitted due to antibiotic-HIV interactions. One was on darunavir/cobicistat and got clarithromycin for sinusitis. Ended up in ICU with QT prolongation. The other? Rifampin. No one checked the Liverpool database. It’s not rocket science. Just… check it.
ann smith
26 November, 2025 13:00 PMThis is so important. 💙 I’ve been on dolutegravir for 5 years and just got a UTI last month. My doctor prescribed nitrofurantoin without hesitation-thank goodness. I always double-check with my pharmacist now. Knowledge is power, and this post is a gift. 🙏
Julie Pulvino
27 November, 2025 16:55 PMI’m 47 and on tenofovir alafenamide. My doc gave me doxycycline for acne last year and I was nervous AF. Looked it up and it was fine. But I didn’t know about the TDF + ciprofloxacin thing. Yikes. I’m switching to TAF next month. This post saved me from a potential kidney disaster. Thanks for sharing.
Patrick Marsh
28 November, 2025 01:48 AMRifabutin. Dose adjustment. Therapeutic drug monitoring. Check the Liverpool database. Don’t guess. Don’t assume. Don’t rely on memory.
Danny Nicholls
29 November, 2025 15:21 PMbro this is wild 🤯 i had no idea antibiotics could wreck hiv meds like that. i thought it was just ‘take your pills’ and ‘take your antibiotics’ and boom you’re fine. turns out your liver is like a tiny bar fight and the drugs are brawling. also i just used the Liverpool checker and my med combo is safe 😅 thanks for the heads up. sharing this with my whole group chat.
Robin Johnson
1 December, 2025 03:10 AMIf you’re on HIV meds and your doctor prescribes an antibiotic without checking interactions, fire them. Seriously. This isn’t optional. This isn’t ‘maybe.’ This is a preventable death. If you’re not using the Liverpool database, you’re gambling with your life. And if you’re a provider? You’re negligent if you don’t know this. Period.
Latonya Elarms-Radford
1 December, 2025 03:18 AMAh, the tragic ballet of pharmacokinetics-where enzymes become silent judges in the courtroom of our cellular existence. We are not mere vessels, but intricate symphonies of metabolic pathways, each note trembling under the weight of pharmaceutical interference. Rifampin, that cruel maestro, conducts a crescendo of CYP3A4 induction, while ritonavir, the brooding baritone, silences the chorus with its inhibitory decree. And yet… we persist. We survive. We are the living archives of medical contradiction, dancing on the edge of biochemical oblivion. Is this not the poetry of modern medicine? Or merely its most haunting elegy?
Mark Williams
2 December, 2025 05:35 AMThe CYP3A4-mediated drug-drug interaction (DDI) profile between boosted protease inhibitors and macrolides represents a clinically significant pharmacokinetic conflict. The inhibition constant (Ki) for ritonavir against CYP3A4 is approximately 0.003 μM, resulting in a 60–82% increase in AUC for clarithromycin. Meanwhile, rifampin induces CYP3A4 expression via PXR activation, reducing darunavir exposure by up to 80%. These are not ‘side effects’-they are pharmacodynamic destabilizations with direct implications for virologic failure and resistance development. The integration of pharmacogenomic screening into routine HIV care is not merely ideal-it is imperative.