Every pill you swallow, every injection you get, every inhaler you use-none of it works by magic. Medicines are chemicals, carefully designed to interact with your body in very specific ways. But knowing how medicines work isn’t just for doctors. Understanding this is the single biggest thing you can do to use medications safely-and avoid dangerous mistakes.
How Medicines Actually Work in Your Body
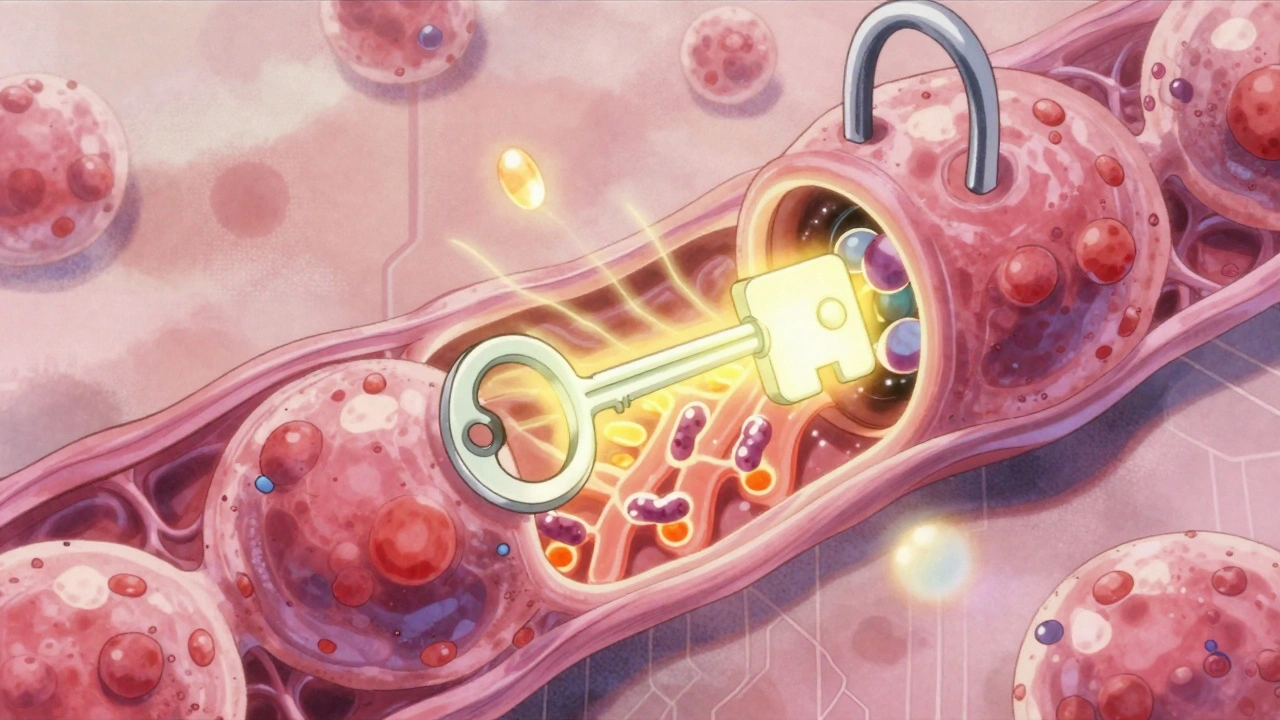
Medicines don’t just float around until they ‘fix’ something. They have a target. Think of it like a lock and key. Your body has millions of tiny receptors-protein structures on cells-that do specific jobs. Some control pain signals. Others regulate mood, blood pressure, or inflammation. Medicines are designed to fit into these locks. Some medicines, called agonists, are like the right key. They slide in and turn the lock, making the cell do what it’s supposed to do. For example, insulin is a natural key your body uses to open receptors that let sugar into cells. If you have diabetes, you’re given synthetic insulin to replace what your body can’t make. Other medicines, called antagonists, are like a broken key. They fit into the lock but don’t turn it. They just block the real key from getting in. That’s how antihistamines work during allergies. They block histamine receptors so your body doesn’t react to pollen the way it normally would. Then there are drugs like aspirin. It doesn’t just block one lock-it shuts down an entire factory. Aspirin stops an enzyme called COX-1 from making prostaglandins, chemicals that cause pain and swelling. No prostaglandins? Less pain. But that same action also reduces stomach protection, which is why long-term use can cause ulcers. Not all medicines work the same way. Antibiotics like penicillin don’t target human cells at all. They attack bacteria by breaking down their cell walls. Your body’s cells don’t have those walls, so the drug leaves you alone-but kills the infection.Why Your Body’s Chemistry Matters
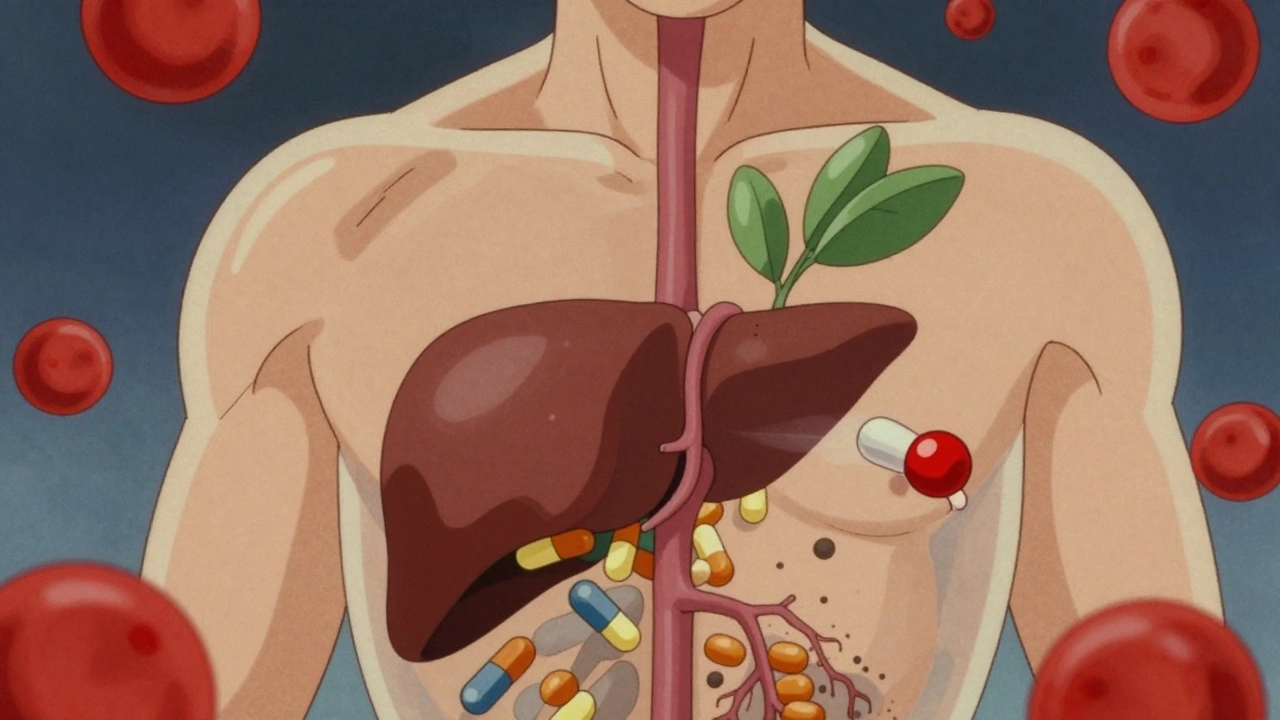
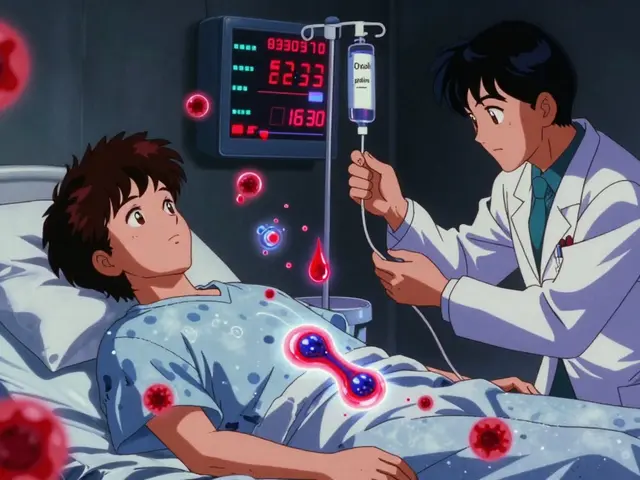
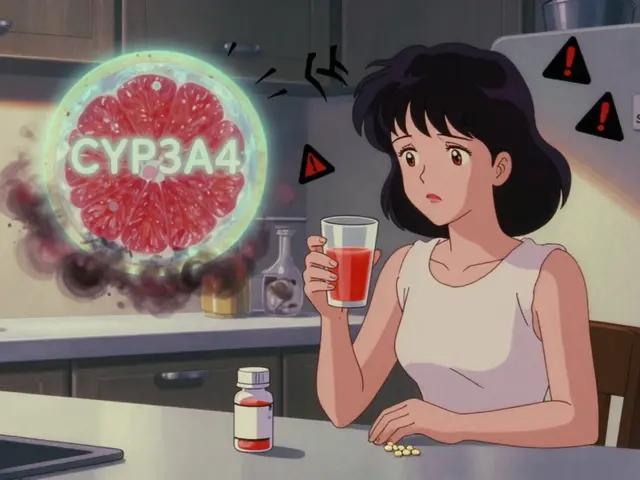
Just because a drug works in a test tube doesn’t mean it’ll work the same way in your body. What happens after you swallow a pill? It goes through your stomach, gets absorbed into your blood, travels to your liver, and then to the rest of your body. Along the way, your body changes it. About 40% to 90% of some oral drugs get broken down by your liver before they even reach your bloodstream. This is called the first-pass effect. That’s why morphine needs a higher dose when taken by mouth than when given through an IV. Your body is filtering it out before it gets to work. Then there’s protein binding. Up to 98% of many drugs stick to proteins in your blood. That’s not bad-it helps them travel. But only the 2% to 5% that’s floating free can actually interact with your cells. If you take another drug that also binds to those same proteins, it can kick your medicine off. That’s why warfarin (a blood thinner) is so dangerous when mixed with some antibiotics or even certain painkillers. Suddenly, more warfarin is free in your blood-and you’re at risk of bleeding. The blood-brain barrier is another filter. Most drugs can’t cross it. That’s why you can’t just take a pill to treat Parkinson’s and expect it to reach your brain. That’s why Sinemet® combines levodopa with carbidopa. Levodopa can slip through the barrier; carbidopa stops it from breaking down too early so more of it reaches the brain.When Medications Are Safe to Use
Safety doesn’t mean “no side effects.” It means using the right drug, at the right dose, for the right person, at the right time. Take lithium, used for bipolar disorder. It’s effective-but it’s also dangerous if your blood level is even slightly too high. The safe range is tiny: 0.6 to 1.2 mmol/L. Too low? It won’t work. Too high? You get tremors, confusion, kidney damage. That’s why people on lithium get regular blood tests. Their doctor isn’t just checking if it’s working-they’re making sure it’s not poisoning them. Statins, used to lower cholesterol, are safer because we know exactly how they work. They block an enzyme called HMG-CoA reductase, which your liver uses to make cholesterol. That means we can measure cholesterol levels to see if the dose is right. If your LDL is still too high, we increase the dose. If your muscles hurt, we check for a sign of a rare but serious side effect called rhabdomyolysis. Patients who understand this connection are more likely to report muscle pain early-and avoid hospitalization. But here’s the scary part: 32% of reported drug side effects, according to the FDA, happen because patients didn’t understand how their medicine worked. People on MAO inhibitors for depression ate aged cheese, thinking it was harmless. But aged cheese has tyramine, which reacts with MAO inhibitors to spike blood pressure dangerously. One slice can cause a stroke.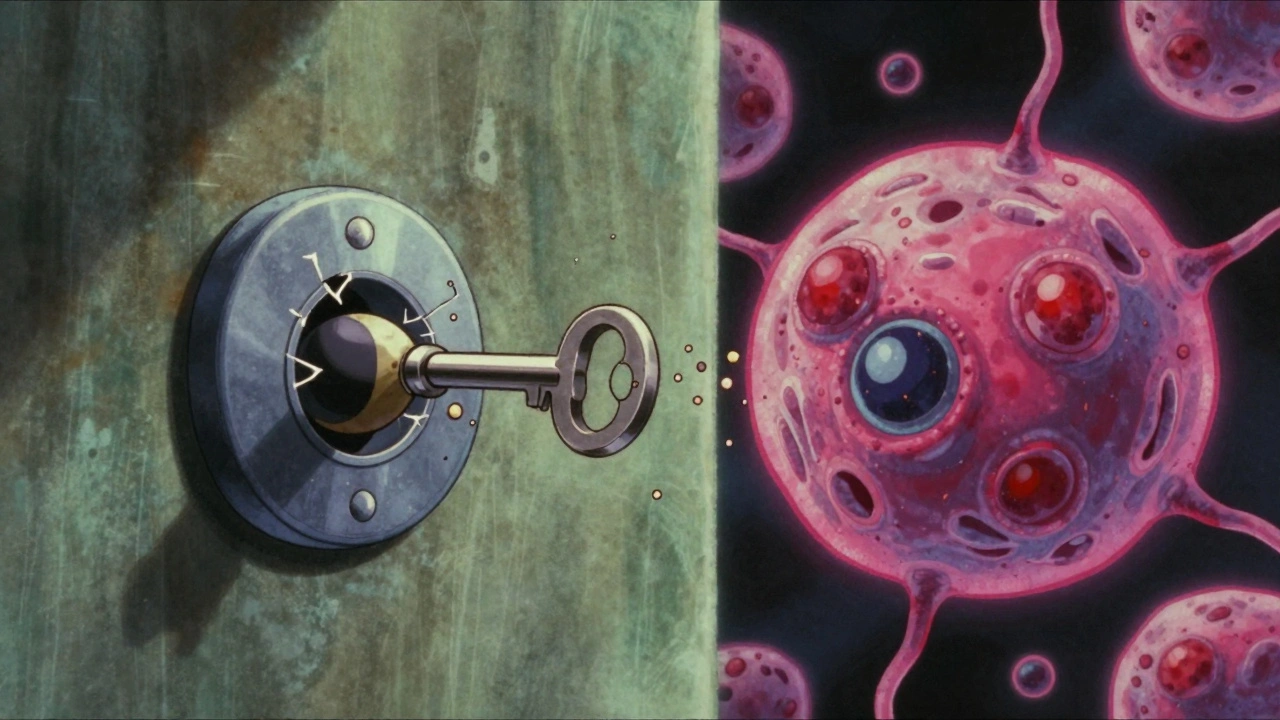
Why Your Doctor Should Explain the Mechanism
Doctors used to think patients didn’t want to know the science. That’s changing. A 2023 survey by the American Cancer Society found that 78% of patients on trastuzumab (Herceptin) for breast cancer felt more confident when they understood it targeted a specific protein (HER2) on cancer cells. They knew what to watch for-like heart issues-and didn’t panic over every little symptom. Patients on warfarin who understood it blocked vitamin K could adjust their diet. They didn’t avoid greens completely-they just kept them consistent. One day, 2 cups of spinach. The next day, 2 cups again. Not 2 cups one day and none the next. That consistency kept their INR levels stable. Pharmacists now use simple analogies: “SSRIs are like putting a cork in the serotonin recycling tube.” That’s why you can’t stop them cold turkey-you’ve got serotonin piling up in the space between nerves. Stop the cork, and the system crashes. Withdrawal symptoms? That’s your brain adjusting.What You Can Do to Stay Safe
You don’t need a pharmacology degree. But you do need to ask three questions:- What is this medicine supposed to do? Is it blocking pain? Lowering blood pressure? Killing bacteria?
- What should I watch out for? If it affects your liver, you might get yellow eyes. If it lowers your blood pressure too much, you’ll feel dizzy. If it interacts with food, know what that food is.
- What happens if I miss a dose or stop it? Some drugs need to be tapered. Stopping antidepressants suddenly can cause brain zaps, nausea, or anxiety. Stopping beta-blockers cold can trigger a heart attack.
The Future of Safe Medication Use
Science is moving fast. The NIH’s All of Us program is studying how your genes affect how you respond to drugs. Right now, 28% of bad reactions are linked to genetic differences. In five years, a simple blood test might tell your doctor: “This person metabolizes this drug too slowly. Give them half the dose.” New drugs are being designed with safety built in. Direct oral anticoagulants (DOACs) replaced warfarin for many people because they don’t need constant blood tests. Their mechanism is clear: one blocks factor Xa, another blocks thrombin. No vitamin K interference. No food restrictions. Fewer dangerous interactions. But here’s the truth: technology won’t fix what ignorance creates. Even the smartest drug can be dangerous if you don’t understand how it works. The FDA now requires doctors to complete training on the mechanism of high-risk drugs like natalizumab-because they knew that if doctors understood how it blocked immune cells from entering the brain, they’d know to watch for a rare brain infection called PML.Final Thought: Knowledge Is Your Shield
Medicines are powerful tools. But they’re not harmless. The difference between healing and harm often comes down to one thing: understanding. Not memorizing side effect lists. Not trusting your pharmacist to handle it. But knowing the basic story of how the drug moves through your body and what it’s trying to fix. If you’re on a new medication, ask your doctor or pharmacist: “How does this work?” Then ask: “What should I look out for?” And don’t stop there. If you’re not sure, look it up. Reputable sources like the NIH or FDA have patient-friendly explanations. You’re not just taking a pill. You’re entering a chemical conversation with your body. Know what you’re saying.How do medicines know where to go in my body?
Medicines don’t “know” where to go. They travel through your bloodstream and interact with cells that have the right receptors-like a key fitting into a lock. Drugs are designed to match specific proteins or enzymes. For example, insulin binds to insulin receptors on muscle and fat cells. Antibiotics target bacterial structures your body doesn’t have. If a drug doesn’t find its target, it gets broken down or excreted.
Can I stop taking my medicine if I feel better?
It depends. For antibiotics, stopping early can let surviving bacteria become resistant. For blood pressure or antidepressants, stopping suddenly can cause rebound effects-your symptoms can come back worse. Always check with your doctor before stopping. Even if you feel fine, the medicine might still be working behind the scenes to prevent a relapse or complication.
Why do some medicines have so many side effects?
Because your body is complex. A drug designed to target one receptor might accidentally affect others that look similar. For example, some older antihistamines block histamine receptors in your brain, causing drowsiness. Newer ones are designed to avoid that. Also, if a drug affects a system that does multiple things-like inflammation-it might reduce pain but also weaken your stomach lining. Side effects aren’t always mistakes-they’re often unavoidable trade-offs.
Are natural supplements safer than prescription drugs?
No. “Natural” doesn’t mean safe. St. John’s Wort can interfere with birth control, antidepressants, and heart medications. Kava can cause liver damage. Garlic supplements can thin your blood-dangerous if you’re on warfarin. Supplements aren’t tested the same way as prescription drugs. They don’t have to prove safety or effectiveness before being sold. Always tell your doctor what supplements you take.
What should I do if I think a medicine is causing a side effect?
Don’t ignore it. Don’t stop the medicine without talking to your doctor. Write down the symptom, when it started, and how bad it is. Call your doctor or pharmacist. If it’s serious-like chest pain, trouble breathing, swelling, or black stools-go to the ER. Even if you’re not sure, report it. The FDA’s MedWatch system uses these reports to catch dangerous patterns early.
How can I tell if my medication is working?
It depends on the drug. For blood pressure meds, you’ll check your numbers. For statins, your cholesterol levels. For antidepressants, you might track your mood over weeks. Some drugs, like insulin, give immediate feedback-you feel better when your blood sugar drops. Others take time. If you’re unsure, ask your doctor what signs to look for. Don’t wait for a crisis to know if it’s working.
Knowing how your medicine works doesn’t make you a pharmacist. But it makes you a safer, more confident patient. And in a world where medications can save lives-or hurt them-that’s not just helpful. It’s essential.



Elliot Barrett
10 December, 2025 23:21 PMFinally someone explains this without the corporate fluff. I used to take ibuprofen like candy till I read it shuts down your stomach's protective enzymes. Now I know why I got that ulcer. Thanks for not sugarcoating it.
Andrea Beilstein
12 December, 2025 00:12 AMIt's fascinating how we've turned chemistry into a conversation with our own biology
Every pill is a whispered negotiation between science and survival
We don't just take drugs we enter into silent treaties with our cells
And yet we treat them like candy or magic bullets
What if we started seeing medicine not as a fix but as a dialogue
A dance of molecules that requires respect not just compliance
The body isn't a machine to be fixed it's a living ecosystem we're subtly tuning
And when we ignore the language of that system we pay the price in pain or worse
iswarya bala
13 December, 2025 18:12 PMOMG this is so helpful!! I always thought natural stuff is safer but now i get why st johns wort messed with my birth control 😅 thanks for breaking it down so simple!!
Simran Chettiar
15 December, 2025 04:06 AMThe underlying philosophical implication of pharmacological mechanism is not merely biochemical but ontological in nature
Medication as a technological intervention into the corporeal self reveals a fundamental epistemic shift in modern medicine from holistic healing to molecular targeting
The reductionist paradigm has yielded remarkable efficacy yet simultaneously estranged the patient from the experiential dimension of their own physiology
When we cease to comprehend the symbolic architecture of drug action we regress into passive consumers of biomedical technology rather than active participants in our own somatic sovereignty
This is not merely a matter of safety but of existential agency in the age of pharmaceutical hegemony
om guru
15 December, 2025 18:16 PMUnderstanding drug mechanism is essential for patient safety
Always consult qualified healthcare professionals before making any changes to medication regimen
Consistency and awareness prevent adverse outcomes
Knowledge empowers
Respect the science
Richard Eite
15 December, 2025 18:47 PMUSA has the best meds in the world and you people still don't get it
Europe and India are still using 1980s medicine while we got gene-targeted biologics
Stop whining about side effects and take your pills like adults
Also St Johns Wort is for hippies not real people
Katherine Chan
16 December, 2025 23:45 PMThis made me feel so much less alone in my meds journey
I used to panic every time I felt weird after a new prescription
Now I know its just chemistry talking not my body breaking
Thank you for making this feel human not scary
Keep sharing this kind of stuff please
Philippa Barraclough
17 December, 2025 17:04 PMThe concept of the first-pass effect is particularly compelling when considered alongside variations in hepatic enzyme expression across populations. The CYP450 system demonstrates significant polymorphic variation which directly impacts bioavailability and therapeutic efficacy. For instance, individuals of East Asian descent often exhibit reduced CYP2D6 activity, which alters the metabolism of numerous antidepressants and beta-blockers. This genetic variability underscores the necessity of personalized dosing rather than standardized protocols. Furthermore, the interplay between drug-protein binding and renal clearance introduces additional layers of complexity that are rarely addressed in patient education materials. The current paradigm of pharmacological instruction remains frustratingly reductive.
Tim Tinh
19 December, 2025 09:02 AMJust wanted to say this is the best thing I've read all week
I used to think my anxiety meds were just making me numb
Now I get that they're slowly rewiring how my brain handles stress
My therapist never explained it like this
Thanks for the clarity
Olivia Portier
20 December, 2025 14:07 PMSo many people dont realize that warfarin isnt the enemy its the inconsistency that kills
I had a friend who ate kale one day and skipped it the next
Her INR went crazy and she ended up in the ER
Now she eats the same amount every day and its fine
Knowledge really is power
Shubham Mathur
22 December, 2025 01:49 AMFinally someone gets it! The body isn't a broken machine to be fixed it's a living system that needs respect
Pharma companies don't want you to understand this because then you'd question why they push one-size-fits-all doses
Genetics matter
Diet matters
Timing matters
Stop treating medicine like a vending machine and start treating your body like the miracle it is