Grapefruit Juice Interaction Checker
Grapefruit juice can significantly increase the concentration of certain medications in your bloodstream, potentially leading to serious side effects. This tool helps you determine if your medication interacts with grapefruit juice based on known interactions discussed in the article.
Important Safety Information
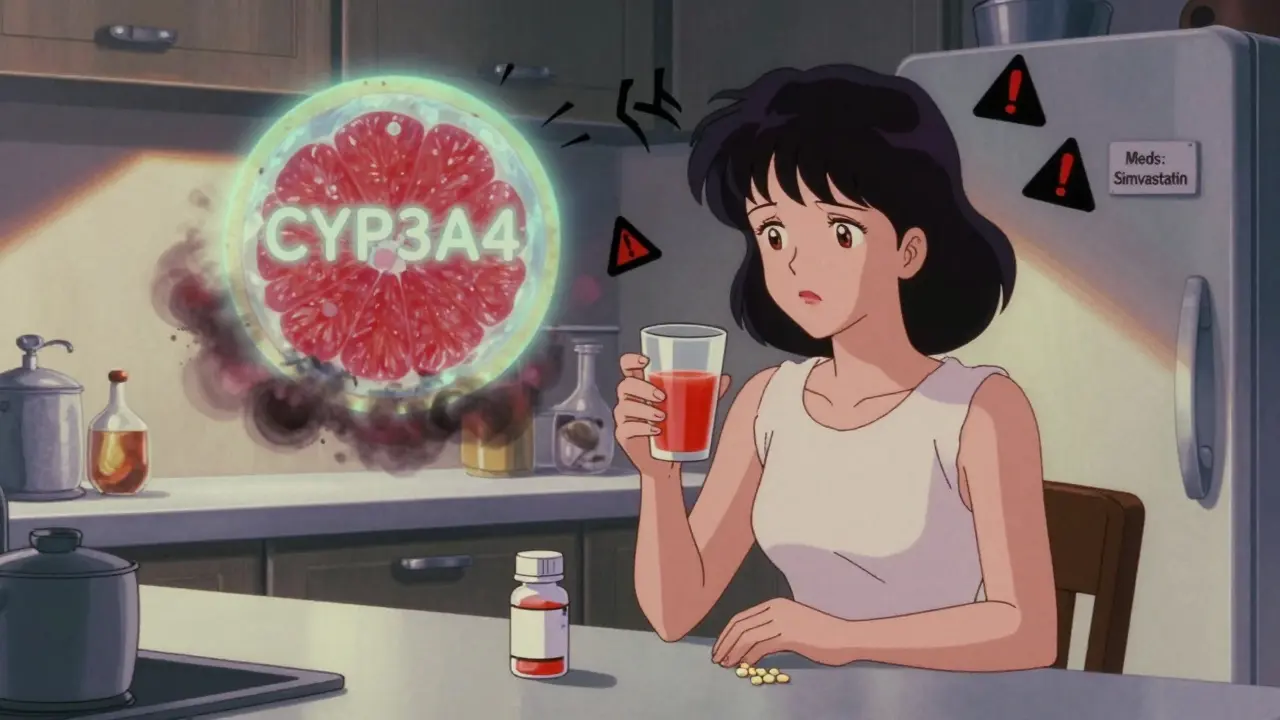
Did you know? Grapefruit juice inhibits the CYP3A4 enzyme in your liver and intestines, which is responsible for metabolizing many medications. When this enzyme is blocked, your body cannot clear the drug effectively, leading to potentially dangerous levels in your bloodstream.
Common affected medications: Statins (simvastatin, atorvastatin), some blood pressure medications (felodipine, nifedipine), and certain antidepressants.
What to do: If your medication interacts with grapefruit juice, avoid consuming grapefruit, grapefruit juice, or Seville oranges. Always check with your pharmacist or doctor before making changes to your diet while taking medications.
When you take a pill for high blood pressure, you expect it to help - not make you sicker. But what if that same pill, when taken with another medication, a supplement, or even grapefruit juice, turns a mild side effect into something dangerous? This isn’t rare. It’s happening every day in homes, clinics, and hospitals. Drug interactions are one of the most overlooked reasons why side effects get worse - and why people end up in the ER when they thought they were just following their doctor’s advice.
What Exactly Is a Drug Interaction?
A drug interaction happens when one substance changes how another substance works in your body. It doesn’t mean the drug is broken. It means something else - another pill, a food, a herbal supplement, or even your own genes - is messing with how your body handles it. These interactions don’t always cause obvious symptoms right away. Sometimes, they quietly boost the drug’s effect until you’re suddenly dizzy, bleeding, or having muscle pain so bad you can’t walk. The most common type of interaction is pharmacokinetic. That’s a fancy word for how your body absorbs, breaks down, or gets rid of a drug. The liver is the main player here, especially a group of enzymes called CYP3A4 a liver enzyme responsible for breaking down about half of all commonly prescribed medications. When something blocks CYP3A4 - like the antibiotic clarithromycin or grapefruit juice - your body can’t clear the drug fast enough. The drug builds up. And when it builds up, side effects get worse.How Grapefruit Juice Can Turn a Safe Drug Into a Risk
Grapefruit juice is the classic example. People think it’s healthy. It’s full of vitamin C. But for some medications, it’s like pouring gasoline on a fire. If you’re taking a statin like simvastatin or atorvastatin to lower cholesterol, grapefruit juice can increase the drug’s concentration in your blood by up to 300%. That sounds harmless until you start getting muscle pain, weakness, or dark urine - signs of rhabdomyolysis, a condition where muscle tissue breaks down and can damage your kidneys. Compare that to amlodipine, a blood pressure drug. Grapefruit juice barely affects it. Why? Because different drugs use different enzymes. Simvastatin is heavily dependent on CYP3A4. Amlodipine isn’t. That’s why some people can sip grapefruit juice with their pills and feel fine, while others end up in the hospital. The difference isn’t luck. It’s chemistry.When Two Drugs Team Up to Harm You
Sometimes, it’s not about one drug being too strong. It’s about two drugs working together to create a dangerous effect. This is called a pharmacodynamic interaction. Take warfarin, a blood thinner. It’s meant to keep clots from forming. But if you add aspirin - even a daily baby aspirin for heart protection - you’re doubling the risk of internal bleeding. Studies show this combo increases bleeding risk by 70-100%. And it’s not just aspirin. Garlic supplements, ginkgo, even too much vitamin E can do the same thing. Your doctor might not mention it because they’re focused on your heart. But your bleeding risk? That’s just as important. Another scary combo is SSRIs (antidepressants) with tramadol (a painkiller). Both raise serotonin levels. Alone, they’re fine. Together? You can get serotonin syndrome - a rare but life-threatening reaction that causes confusion, rapid heartbeat, high fever, and muscle stiffness. There are hundreds of Reddit posts from people who didn’t know this was possible. One user wrote: “I took Zoloft for anxiety and tramadol for back pain. Three days later, I couldn’t stop shaking. I thought I was having a panic attack. Turns out, it was serotonin syndrome.”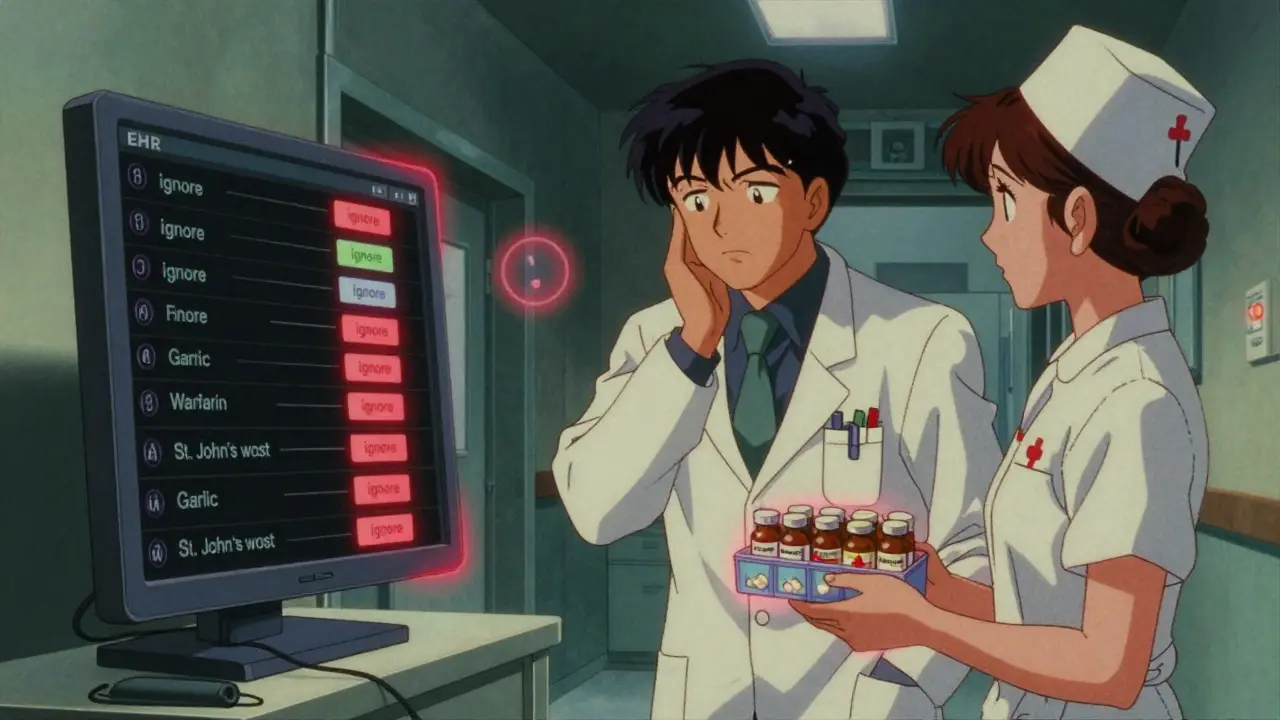
Why Some People Are at Higher Risk
Not everyone reacts the same way. Your genes matter. About 5-10% of white people have a genetic variation that makes them “poor metabolizers” of CYP2D6, another liver enzyme. If you’re one of them and you take codeine - a common painkiller - your body can’t turn it into morphine properly. Instead, you get almost no pain relief. But if you’re a “super metabolizer”? Your body turns codeine into morphine too fast. That’s when you overdose on your own prescription. The same goes for warfarin. Some people need 2 mg a day. Others need 10 mg. Why? Genetics. Age. Liver health. Kidney function. The more conditions you have, the more your body’s ability to handle drugs changes. That’s why older adults on five or more medications have an 80% higher chance of a bad reaction. Polypharmacy isn’t just about taking a lot of pills. It’s about how those pills interact with each other - and with your body.The Most Dangerous Drug Combinations
Some combinations are so risky they’ve been pulled from the market. Cisapride, a stomach motility drug, was taken off shelves in 2000 after 80 deaths linked to interactions with antibiotics like clarithromycin. The combo caused a dangerous heart rhythm called torsades de pointes. Even today, certain antiarrhythmics, antipsychotics, and antidepressants carry black box warnings - the FDA’s strongest alert - because of interaction risks. Here are three of the most dangerous combos still in use:- Statins + Clarithromycin: Increases risk of rhabdomyolysis by 8.4 times. Azithromycin is a safer antibiotic choice here.
- Warfarin + Amiodarone: Amiodarone, used for irregular heartbeat, can double warfarin’s effect. INR levels can spike overnight.
- SSRIs + Triptans: Used for migraines. Together, they raise serotonin syndrome risk - especially in people on multiple antidepressants.
Why Doctors Miss These Interactions
You’d think electronic health records would catch all this. They don’t. A 2023 survey of 3,500 doctors found that 58% admit they sometimes ignore interaction alerts. Why? Because they’re flooded. For every one real danger, there are 10 alerts for low-risk combos. Doctors get so used to clicking “ignore” that they stop paying attention. Nurses notice more. A 2022 study found nurses caught 40% of drug interactions that doctors missed. Why? Because they’re the ones checking pills, asking about supplements, and noticing when a patient says, “I’ve been drinking grapefruit juice every morning for years.” And patients? Many don’t know what to say. They think “I take vitamins” means “I take a multivitamin.” They don’t mention turmeric, St. John’s wort, or CBD oil - all of which interact with common meds.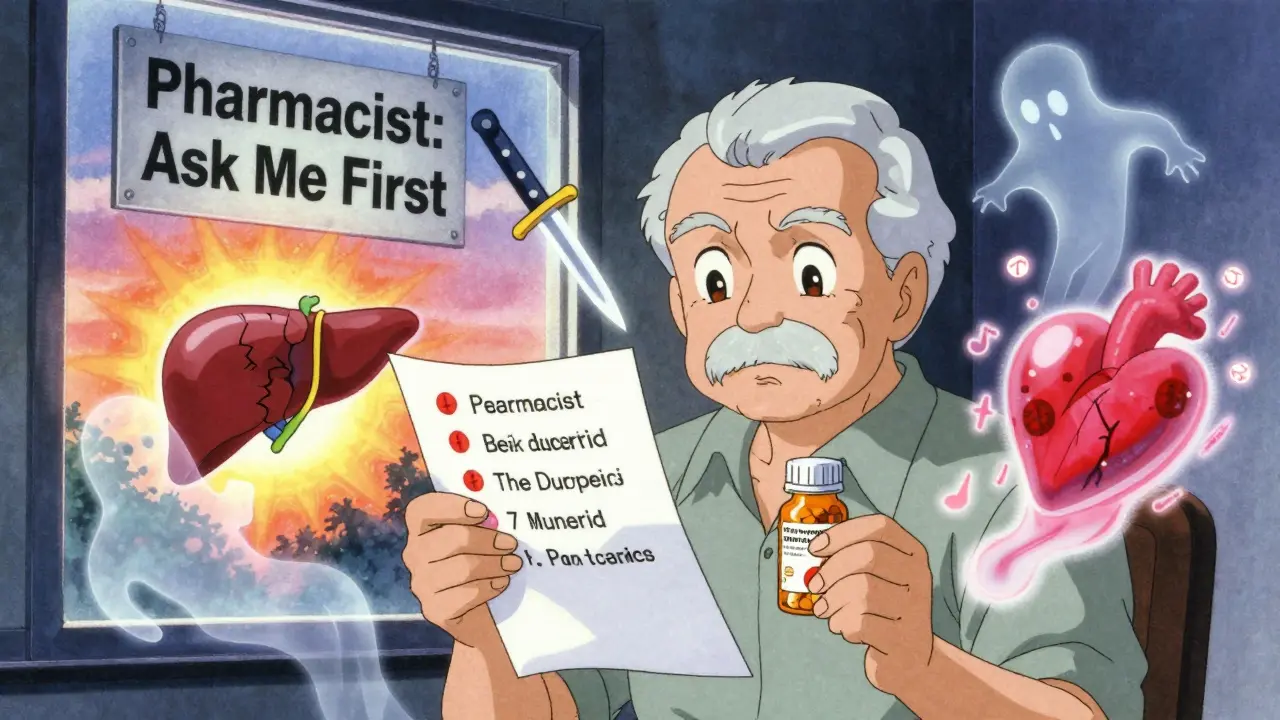
What You Can Do to Stay Safe
You don’t need to be a pharmacist to protect yourself. Here’s what actually works:- Keep a full list of everything you take. Include prescription drugs, over-the-counter meds, supplements, herbs, and even energy drinks. Write it down. Update it every time you start or stop something.
- Ask your pharmacist. They’re trained to spot interactions. Bring your list to the pharmacy every time you refill a prescription. They’ll check for clashes you didn’t know about.
- Don’t assume natural = safe. St. John’s wort can make birth control fail. Garlic supplements can thin your blood. Green tea can interfere with blood pressure meds. Just because it’s herbal doesn’t mean it’s harmless.
- Know your meds. If you’re on a statin, avoid grapefruit. If you’re on warfarin, keep vitamin K intake steady - don’t suddenly eat a bunch of kale or spinach. Consistency matters more than avoidance.
- Speak up. If you feel weird after starting a new drug - dizziness, nausea, muscle pain, bruising - don’t wait. Call your doctor. Say: “I think this might be an interaction.”
What’s Changing Now
Technology is starting to help. AI tools now predict dangerous drug combos with 89% accuracy - better than older systems. Some hospitals are using pharmacogenetic testing to see how patients metabolize drugs before prescribing. Early results show a 36% drop in high-risk interactions. The FDA now requires new drugs to be tested against seven major enzymes and three transporters. That means future drugs will come with clearer warnings. But that doesn’t help you today. The real fix? Better communication. Between doctors and patients. Between pharmacies and hospitals. Between what’s written on a label and what’s actually happening in your body.Bottom Line
Side effects aren’t always just a side effect. Sometimes, they’re a signal - a warning that something else is interfering. Drug interactions are preventable. They don’t have to be a surprise. With better awareness, better questions, and better habits, you can avoid the worst of them. Your body doesn’t need more drugs. It needs smarter ones.Can over-the-counter meds cause dangerous drug interactions?
Yes. Pain relievers like ibuprofen and naproxen can increase bleeding risk when taken with blood thinners like warfarin. Antacids with aluminum or magnesium can block absorption of antibiotics like tetracycline. Even common cold medicines with pseudoephedrine can raise blood pressure if you’re on beta-blockers. Always check with a pharmacist before taking OTC drugs if you’re on prescriptions.
Is it safe to take supplements with my medications?
Many are not. St. John’s wort can make antidepressants, birth control, and transplant drugs less effective. Garlic, ginkgo, and ginger can thin your blood and increase bleeding risk with warfarin or aspirin. Curcumin (from turmeric) can interfere with chemotherapy drugs. There’s no universal rule - every supplement has potential risks. Always list them when discussing meds with your doctor.
Why does grapefruit affect some drugs but not others?
It depends on how the drug is processed. Grapefruit blocks CYP3A4, an enzyme in the gut and liver. Drugs like simvastatin, felodipine, and cyclosporine rely heavily on this enzyme to break down. If the enzyme is blocked, the drug builds up. Drugs like amlodipine or rosuvastatin don’t use CYP3A4 much, so grapefruit has little effect. Always check if your drug is on the list of those affected.
Can drinking alcohol increase side effects of my meds?
Absolutely. Alcohol can intensify drowsiness from sedatives, antidepressants, and antihistamines. It can damage the liver when combined with acetaminophen, increasing risk of liver failure. With metronidazole (an antibiotic), alcohol causes severe nausea and flushing. Even moderate drinking can turn a manageable side effect into an emergency. When in doubt, avoid alcohol while on new medications.
How can I tell if a side effect is from a drug interaction?
Look at timing. If a new symptom started after you began a new medication, supplement, or changed your diet (like adding grapefruit juice), it’s likely an interaction. Common signs include unexplained bruising, muscle pain, confusion, rapid heartbeat, or extreme drowsiness. Don’t wait for it to get worse. Contact your provider and list everything you’ve taken recently.






Jesse Lord
8 February, 2026 13:12 PMI've been on statins for years and never knew grapefruit juice could be this dangerous. My mom drinks it every morning with her breakfast. Gonna tell her to stop ASAP. Seriously, this post saved me from a potential ER trip.
Thanks for laying it out so simply.
Patrick Jarillon
9 February, 2026 01:28 AMOh please. This is all Big Pharma fearmongering. They want you to think every natural thing is poison so you'll keep buying their overpriced pills. Grapefruit? It's been eaten for centuries. The real danger is doctors overprescribing statins like they're candy. I stopped mine after reading this and my cholesterol went DOWN. Coincidence? I think not.
Gouris Patnaik
9 February, 2026 21:46 PMIn India, we have been using turmeric and neem with medicines for generations. Your Western obsession with chemical purity is what makes you blind. You think science is the only truth? Ancient wisdom knows the body better than your lab tests. Your system is broken because you trust machines over intuition.
Tola Adedipe
10 February, 2026 16:55 PMI work in a pharmacy and I see this every single day. People come in with 7 prescriptions and 12 supplements and act like they're doing something heroic. I had a guy last week take St. John’s wort with his SSRI and end up in the ER. He didn’t even know they could interact. You don’t need a PhD to know: if it’s not on your doctor’s list, it’s probably not safe. Stop self-experimenting.
Sarah B
10 February, 2026 18:03 PMDoctors dont care. They just want to hit their quotas. I had a dr tell me to stop my blood thinner because I was 'too healthy' and then prescribe me a new one that interacted with my thyroid med. I found out because my cousin is a nurse. Your system is rigged.
Paula Sa
12 February, 2026 05:06 AMI appreciate how you broke this down. I was scared to ask my doctor about my supplements because I didn't want to sound silly. But after reading this, I brought my whole list to my pharmacist last week. She caught three interactions I didn't even know about. Turns out my green tea and my blood pressure med were fighting each other. Small changes, big difference. Thank you for making me feel less alone in this.
Heather Burrows
13 February, 2026 14:58 PMI just don't get why people are so surprised. If you're taking 10 pills a day, of course something's going to go wrong. It's not a conspiracy. It's math. Your body isn't a machine you can plug random things into. It's a delicate ecosystem. And you're treating it like a vending machine. Stop blaming the system. Start taking responsibility.
Marcus Jackson
13 February, 2026 22:38 PMCYP3A4 is the real villain here. And yeah grapefruit juice is the classic example but have you heard of Seville oranges? Same thing. And don't even get me started on pomegranate juice. People think 'natural' means 'safe' but nature is full of toxins. This is basic pharmacology 101. If you're on meds, read the damn leaflet.
Natasha Bhala
15 February, 2026 10:28 AMthis post changed my life honestly
my mom was on warfarin and started taking garlic pills for 'heart health' and started bruising everywhere
i found out bc she dropped her phone and it left a purple mark on the floor
we stopped the garlic and she's fine now
never underestimate the little things
Ashley Hutchins
15 February, 2026 22:07 PMYou think this is bad? Wait till you hear about the 200+ herbal supplements that are banned in Europe but still sold here. And your 'pharmacist' is just a glorified cashier. They don't have time to check. The FDA is corrupt. The real solution? Stop taking pills altogether. Your body can heal itself. Just stop poisoning it.
Lakisha Sarbah
16 February, 2026 03:43 AMI used to think supplements were harmless. Then my aunt had a stroke after mixing fish oil with her blood pressure med. She didn't tell anyone because she thought 'it was just a pill'. Now I carry a printed list of everything I take. I show it to every provider. No shame. No guesswork. Just facts. It's not about being paranoid. It's about being smart.
Niel Amstrong Stein
16 February, 2026 18:42 PMbro i just found out my CBD oil was making my anxiety worse because it interacted with my SSRI 😭
so i stopped it and now i feel like a new person
also i use emoji now so u know im serious
💊➡️🚫
🧠➡️✨
🙏🙏🙏
Joey Gianvincenzi
18 February, 2026 03:15 AMIt is imperative that we recognize the systemic failure in pharmaceutical education and regulatory oversight. The current paradigm, wherein patient safety is subordinated to profit-driven clinical algorithms, is not merely inadequate-it is ethically indefensible. The onus must be placed upon regulatory bodies to enforce mandatory, real-time interaction monitoring systems integrated into all electronic health records. Without structural reform, these preventable tragedies will persist.
Amit Jain
19 February, 2026 22:12 PMThis is why India has 5000 years of Ayurveda and you guys are still arguing about grapefruit. We use ginger, ashwagandha, and turmeric with everything and no one ends up in the hospital. Your science is too narrow. You think one enzyme is the whole story? The body is not a lab. It’s a river. You can't block one tributary and expect the whole system to work. Your medicine is broken because you're trying to fix nature with math.
Savannah Edwards
20 February, 2026 07:58 AMI spent 18 months in chronic pain because I didn't realize my gabapentin and my melatonin were interacting. I thought melatonin was just 'sleep aid'-no one told me it could affect nerve signaling. I finally figured it out when I read a study about GABA receptors. I stopped the melatonin and my pain dropped by 70%. I wish I’d known this sooner. If you’re on any neurological med, don’t assume supplements are harmless. Even the ones that seem 'gentle' can flip a switch you didn’t know existed. Talk to your pharmacist. Don’t wait until you’re shaking.