Medication Drowsiness Risk Calculator
How Does This Tool Work?
This calculator helps you understand your risk of medication-induced drowsiness. Enter the medications you're taking, select when you take them, and we'll provide a personalized risk assessment. The tool uses clinical data from the article to give you insights about your specific situation.
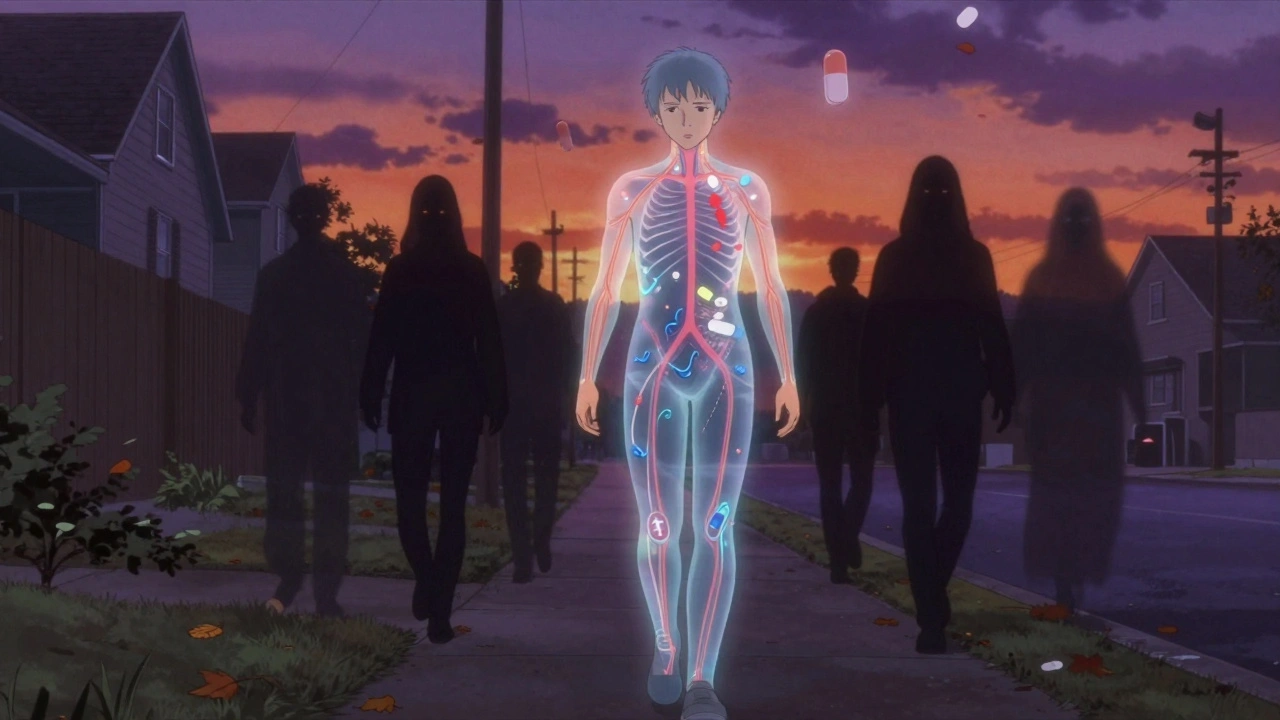
Feeling constantly tired after taking your meds? You’re not alone. About 15-20% of adults experience medication-induced drowsiness, and many don’t even realize their pills are to blame. It’s not just about feeling a little sleepy-it’s about missing work, forgetting appointments, or nearly crashing your car because you couldn’t stay awake. This isn’t normal fatigue. It’s a direct side effect of the drugs you’re taking to feel better.
What Causes Medication-Induced Drowsiness?
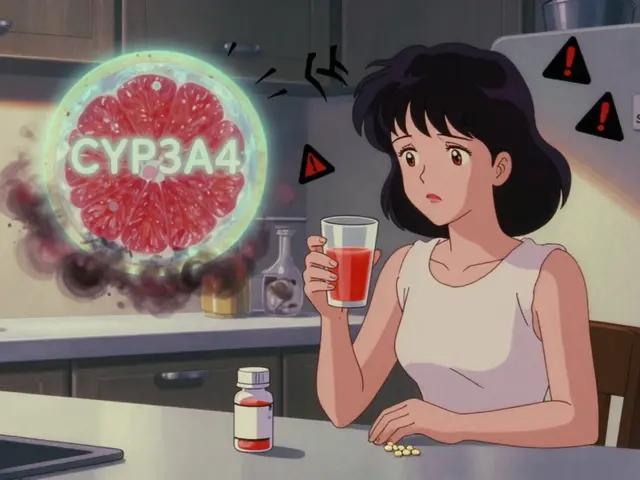
Medication-induced drowsiness, or drug-induced somnolence, happens when a drug slows down your central nervous system (CNS). This isn’t rare-it’s built into how some medicines work. For example, antihistamines like diphenhydramine (Benadryl) and hydroxyzine (Vistaril) are designed to block histamine, a chemical that keeps you alert. But in doing so, they also quiet down brain activity, leaving you foggy and heavy-eyed. Around 50-70% of people who take these first-gen antihistamines report significant drowsiness.
Tricyclic antidepressants like amitriptyline and doxepin work by altering brain chemicals to improve mood, but they also interfere with wakefulness signals. About 30-40% of users say they feel like they’re dragging through the day. Benzodiazepines-such as Xanax, Valium, and Ativan-calm anxiety by boosting GABA, a natural sedative in your brain. The effect can last hours to days, depending on the drug’s half-life.
Even common heart medications like beta-blockers (atenolol, metoprolol) can cause tiredness. They lower your heart rate and blood pressure, which reduces energy flow to your muscles and brain. About 10-15% of users report persistent fatigue. Opioids, muscle relaxants, and even some antibiotics and antivirals have the same effect. The problem gets worse when you combine them. Taking an opioid with a benzodiazepine can dangerously slow your breathing. In 2021, over 16,700 overdose deaths in the U.S. involved this dangerous mix.
Which Medications Are Most Likely to Make You Sleepy?
Not all meds cause drowsiness equally. Here’s a clear breakdown of the top offenders based on clinical data and patient reports:
| Medication Class | Examples | Drowsiness Rate | Notes |
|---|---|---|---|
| First-gen antihistamines | Diphenhydramine, Hydroxyzine, Meclizine | 50-70% | Used for allergies, motion sickness, insomnia |
| Tricyclic antidepressants | Amitriptyline, Doxepin, Imipramine | 30-40% | Often prescribed for chronic pain or depression |
| Benzodiazepines | Alprazolam, Diazepam, Lorazepam | 40-60% | Can cause dependency; withdrawal can be dangerous |
| Beta-blockers | Atenolol, Metoprolol, Propranolol | 10-15% | May improve with switch to nebivolol or bisoprolol |
| Opioids | Oxycodone, Hydrocodone, Morphine | 30-50% | High risk when mixed with other CNS depressants |
| Anticonvulsants | Gabapentin, Pregabalin | 20-35% | Used for nerve pain, seizures, anxiety |
| Muscle relaxants | Cyclobenzaprine, Carisoprodol | 40-60% | Often taken at night, but can linger into morning |
What’s surprising is how often people miss the connection. A 2023 patient behavior study found that 78% of people don’t link their daytime sleepiness to their meds. On average, it takes over 4 months before they talk to a doctor about it. By then, they’ve missed work, fallen once or twice, or felt too tired to enjoy time with family.
Why Timing Matters More Than You Think
One of the simplest fixes? Change when you take your pill. If your medication causes drowsiness, taking it at night instead of in the morning can cut daytime sleepiness by 50-70%. A 2023 clinical review found that 65% of patients who moved their dose to bedtime saw major improvements.
Take tricyclic antidepressants like amitriptyline. Many doctors prescribe them at night anyway because they help with sleep-but patients often take them in the morning by mistake. Switching to evening dosing not only reduces daytime fog but can even improve nighttime sleep quality. Same goes for antihistamines like hydroxyzine or muscle relaxants like cyclobenzaprine. If you’re taking them in the morning, you’re setting yourself up to feel drugged all day.
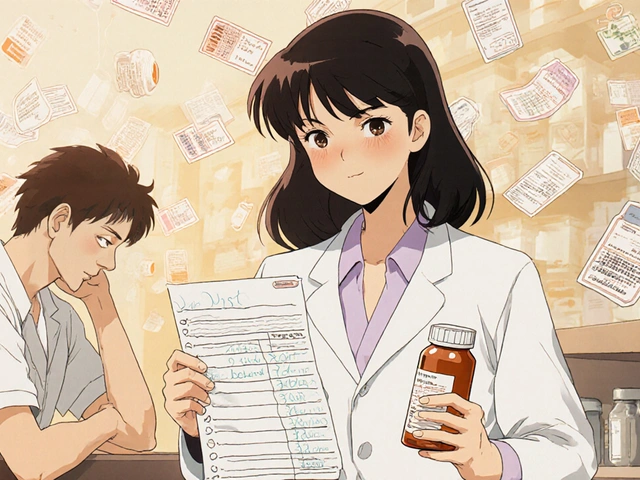
But timing only works if you’re consistent. Skipping doses or switching times randomly can make drowsiness worse. Keep a log: write down when you take each med and how you feel 2-4 hours later. After a week, patterns will show up. Maybe your beta-blocker isn’t the issue-it’s the painkiller you started last month.
What You Can Do (Without Stopping Your Meds)
Never stop a medication cold turkey. Abruptly quitting benzodiazepines, antidepressants, or opioids can trigger seizures, panic attacks, or even life-threatening withdrawal. But you don’t have to suffer either. Here’s what actually helps:
- Get 7-8 hours of sleep every night. If you’re already tired from meds, skimping on sleep makes it worse. Stick to a bedtime routine-no screens an hour before bed.
- Move your body for 20-30 minutes a day. A brisk walk, light yoga, or even stretching improves circulation and brain alertness. One study showed a 30-40% drop in fatigue scores with daily movement.
- Avoid alcohol completely. Alcohol is a CNS depressant. Mixing it with your meds can double or triple drowsiness. It’s not worth the risk.
- Stay hydrated. Dehydration makes drowsiness feel more intense. Drink water throughout the day-don’t wait until you’re thirsty.
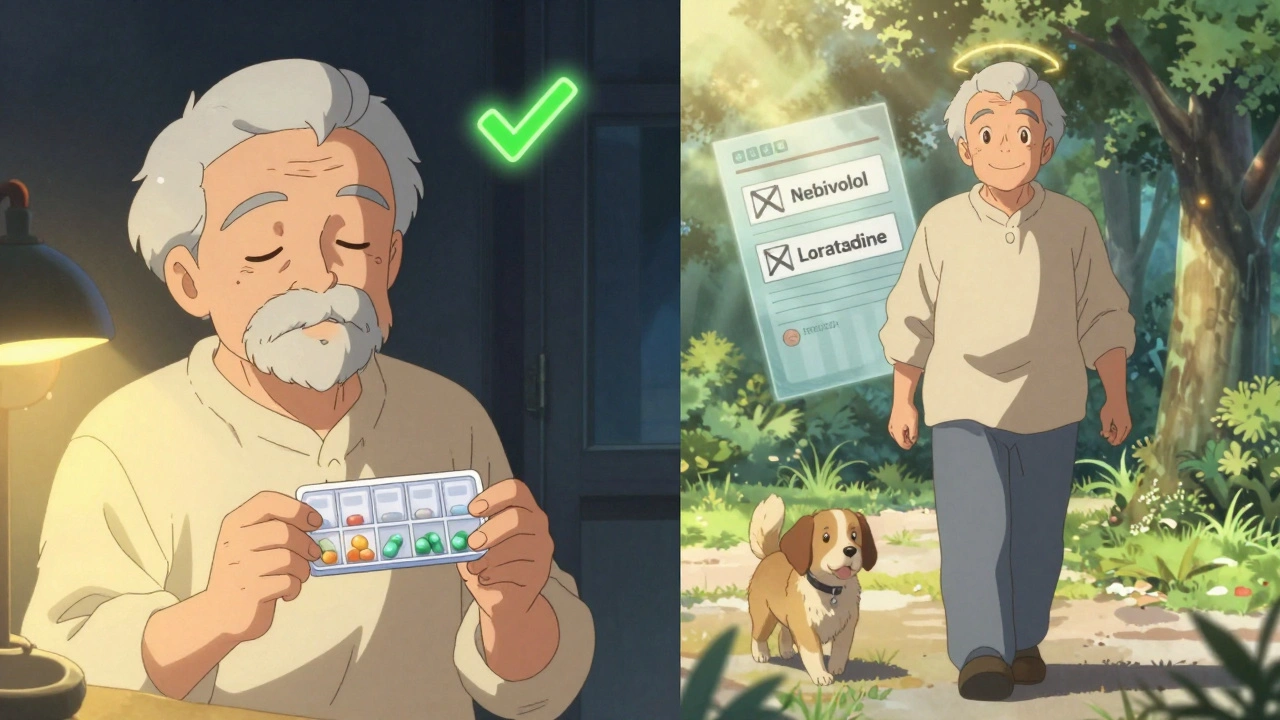
- Try switching to non-sedating alternatives. For allergies, use loratadine (Claritin) or cetirizine (Zyrtec) instead of Benadryl. They’re just as effective and don’t make you sleepy. For depression, newer SSRIs like sertraline or escitalopram are less likely to cause fatigue than tricyclics.
Some patients report success with caffeine-but it’s a double-edged sword. A morning coffee might help you stay awake, but if you drink it after noon, it can wreck your sleep. And if you’re on a benzodiazepine, caffeine can make withdrawal symptoms worse. Use it carefully, and only if you’re not already struggling with sleep.
When to Call Your Doctor
Not all drowsiness is harmless. If you’re experiencing any of these, contact your provider right away:
- Slurred speech, confusion, or trouble walking
- Extreme fatigue that doesn’t improve after 2-4 weeks
- Memory lapses or forgetting to take your meds
- Falls or near-falls, especially if you’re over 65
- Thoughts of self-harm or worsening depression
Your doctor might suggest switching medications, lowering your dose, or adding a non-sedating alternative. For example, switching from propranolol to nebivolol (a newer beta-blocker) helped one Reddit user eliminate afternoon crashes without losing blood pressure control. Or switching from amitriptyline to desvenlafaxine, which one patient said turned their life around-no more 14-hour sleeps.
There’s also new tech on the horizon. Companies like GeneSight offer genetic tests that can predict how your body will react to certain drugs. In trials, patients using these tests had 35% fewer side effects. While not widely covered by insurance yet, it’s worth asking about if you’re on multiple meds and constantly struggling.
What’s Changing in 2025
The FDA is pushing harder for clearer warnings. Since 2016, all opioid and benzodiazepine labels must include black box warnings about deadly sedation. In 2023, the FDA approved solriamfetol (Sunosi), a drug originally for narcolepsy, to treat excessive sleepiness-including that caused by other medications. It’s not a cure-all, but for some, it’s a game-changer when used under specialist care.
Pharmaceutical companies are also designing more “non-sedating” versions of old drugs. Second-gen antihistamines now make up 78% of the allergy market-up from 62% in 2018. That’s progress. But the real solution? Better patient education. The CDC found that people who got clear counseling about side effects had 40% fewer ER visits related to drowsiness.
For older adults, this is critical. The American Geriatrics Society says 34% of medications commonly prescribed to seniors cause drowsiness. That’s why falls are the leading cause of injury in this group. If you or a loved one is over 65, review every pill with a pharmacist. Many can be safely stopped, replaced, or moved to nighttime.
Final Thoughts: You Have Power Here
Medication-induced drowsiness isn’t something you just have to live with. It’s a side effect-and side effects can be managed. Start by tracking your symptoms. Write down what you take, when, and how you feel. Talk to your doctor. Ask if there’s a less sedating option. Consider timing. Stay hydrated. Move every day. Don’t mix with alcohol.
Thousands of people have turned their energy around by making small, smart changes. You can too. The goal isn’t to stop your meds-it’s to take them in a way that lets you live fully, not just survive.
Can medication drowsiness go away on its own?
Yes, for many people, drowsiness lessens after 2-4 weeks as the body adjusts. This is common with antidepressants and some anticonvulsants. But if it persists beyond a month, it’s not normal adaptation-it’s likely the medication’s effect on your system. Don’t assume it’ll get better. Talk to your doctor.
Is it safe to drink coffee to fight medication drowsiness?
It can help in the short term, but it’s risky. Caffeine might mask drowsiness without fixing the root cause. Worse, if you drink it after noon, it can disrupt your sleep, making you even more tired the next day. If you’re on benzodiazepines or antidepressants, caffeine can worsen anxiety or withdrawal. Use it sparingly and never as a long-term fix.
Can I switch to a non-sedating version of my medication?
Often, yes. For allergies, switch from diphenhydramine to loratadine or cetirizine. For depression, ask about SSRIs like sertraline instead of amitriptyline. For blood pressure, nebivolol or bisoprolol are less sedating than propranolol. Always consult your doctor before switching-some changes need careful monitoring.
Why do some meds make me sleepy even if I take them at night?
Some drugs have long half-lives-they stay in your system for hours or even days. Hydroxyzine, for example, can linger for up to 12 hours. Amitriptyline builds up in your blood over time. Even if you take it at night, you might still feel foggy in the morning. If this happens, your doctor may lower your dose or switch you to a faster-clearing option.
Is drowsiness from meds more dangerous for older adults?
Yes. As we age, our bodies process drugs slower, so side effects last longer. Seniors are also more likely to take multiple meds, increasing the risk of dangerous interactions. Drowsiness raises fall risk by 20-30%, and falls are the leading cause of injury and death in people over 65. Always review all medications with a geriatric pharmacist if you’re over 65.
What should I do if I feel too drowsy to drive?
Don’t drive. Period. Even if you think you’re fine. Studies show that drowsiness from meds impairs reaction time as much as being over the legal alcohol limit. If you feel sleepy after taking your pill, wait at least 4-6 hours before driving. If you’re still tired, ask your doctor for an alternative. Your safety-and others’-depends on it.
If you’re taking any of the medications listed above and feel constantly tired, you’re not failing-you’re just using a drug that wasn’t designed with your daily life in mind. But you can change that. Start with your pill log. Talk to your doctor. Ask questions. You deserve to feel awake, alert, and in control of your life.



parth pandya
3 December, 2025 19:17 PMso i been takin amitriptyline for 6 months and yeah its like i got a 2pm nap built in to my life lol. switched to sertraline last month and now i can actually play with my kids after work. no more zombie mode.
Albert Essel
4 December, 2025 07:41 AMThe data presented here is both comprehensive and clinically relevant. It's alarming how frequently patients attribute fatigue to lifestyle factors rather than pharmacological side effects. The 78% statistic regarding unrecognized medication-induced somnolence underscores a critical gap in patient education. Clinicians must proactively discuss sedative potential during prescribing, not merely rely on patient self-reporting.
Charles Moore
4 December, 2025 08:30 AMBeen there. Took hydroxyzine for anxiety and thought I was just 'getting older.' Then I switched to buspirone and suddenly I could finish a book without nodding off. Don't feel guilty for needing to feel awake. Your meds should serve you, not the other way around.
Gavin Boyne
4 December, 2025 13:59 PMSo let me get this straight - we’ve got a whole FDA-approved drug called Sunosi to fix drowsiness caused by other drugs… and the original drugs were never re-designed to not cause it? We’re basically medicating the side effects of our medications. Welcome to the pharmaceutical hamster wheel. At this point, I just drink coffee and pray.
Rashi Taliyan
5 December, 2025 05:35 AMMy grandma took 7 meds and fell three times in one month. The pharmacist sat with us for an hour and crossed out four of them. She’s walking again. Don’t be afraid to ask - your life matters more than the pill bottle.
sagar bhute
6 December, 2025 09:40 AMEveryone’s just blaming the meds. What about the fact that half these people are lazy and don’t exercise? If you’re tired all day, maybe you’re just out of shape. Take a walk. Stop whining. And stop mixing alcohol with your pills - that’s not a side effect, that’s stupidity.
Ignacio Pacheco
6 December, 2025 16:08 PMWait - so if I take my beta-blocker at night, I might stop feeling like a wet sock by 3 PM? Why is this not on every prescription label? And why do doctors act like this is normal? This feels like a systemic failure.
Myson Jones
7 December, 2025 17:44 PMAs someone who’s guided dozens of patients through this exact issue, I want to emphasize: drowsiness isn’t a badge of honor. It’s a signal. Track your symptoms. Challenge assumptions. And if your doctor dismisses your fatigue as 'just part of aging' or 'all in your head' - find a new one. You deserve to feel alive, not sedated. I’ve seen people transform their lives with simple timing changes and one medication swap. It’s not magic. It’s medicine done right.