MAOI-Opioid Interaction Checker
This interactive tool helps you determine if your MAOI medication is safe to take with common opioids. Based on clinical evidence from the article "Opioids with MAOIs: The Deadly Interaction You Must Avoid".
Interaction Results
Why Mixing Opioids and MAOIs Can Kill You
It sounds like something out of a medical thriller: you take a common painkiller for a bad back or dental surgery, and within hours, your body starts shutting down. Your temperature spikes to 107°F, your muscles lock up, your heart races, and you can’t breathe. This isn’t fiction. It’s what happens when opioids and MAOIs are taken together. And it happens more often than you think.
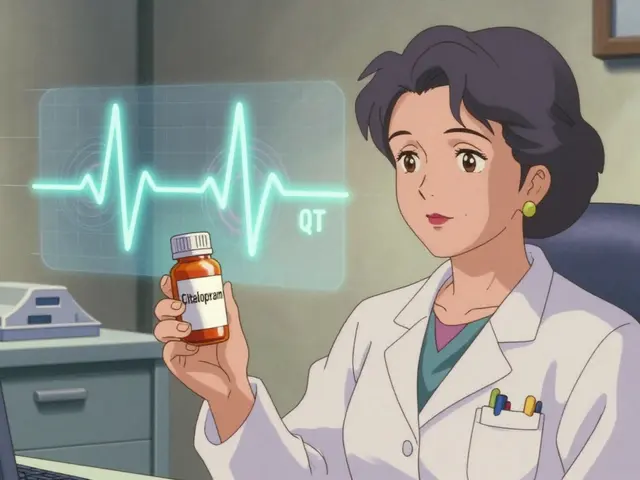
MAOIs - monoamine oxidase inhibitors - are antidepressants like phenelzine (Nardil), tranylcypromine (Parnate), and isocarboxazid (Marplan). They’re not used often anymore, but they’re still prescribed for treatment-resistant depression. About 1.2 million people in the U.S. are on them right now. Meanwhile, opioids like tramadol, methadone, and meperidine are commonly given for pain. The problem? These drugs don’t just coexist - they collide. And the result can be fatal.
The Science Behind the Deadly Mix
MAOIs work by blocking an enzyme called monoamine oxidase, which normally breaks down serotonin, norepinephrine, and dopamine in your brain. When this enzyme is turned off, those neurotransmitters build up. That’s good for mood - but dangerous when opioids come into the picture.
Some opioids - especially tramadol, meperidine, and methadone - don’t just relieve pain. They also flood your system with more serotonin and norepinephrine. Tramadol, for example, blocks serotonin reuptake with the same strength as some antidepressants. Meperidine directly releases serotonin. When you combine these with an MAOI, serotonin levels can jump 300-500% above normal within an hour. That’s not a slight increase. That’s a chemical storm.
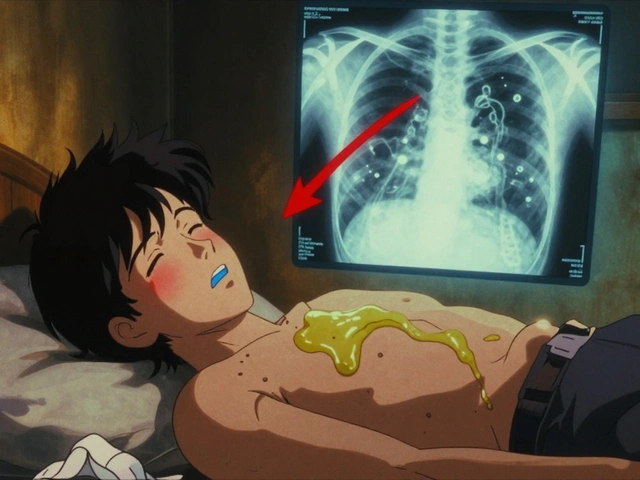
This overload triggers serotonin syndrome - a condition where your nervous system goes into overdrive. Symptoms include high fever, muscle rigidity, confusion, seizures, rapid heartbeat, and dangerously high blood pressure. In severe cases, your organs start failing. Studies show 2-12% of people with severe serotonin syndrome die. And it can happen faster than you’d expect - sometimes within 1-2 hours of taking the opioid.
The Opioids That Are Most Dangerous
Not all opioids are equally risky. The danger varies by how much they affect serotonin and norepinephrine.
- Meperidine (Demerol): The worst offender. Between 1960 and 2010, it was linked to 37 deaths when combined with MAOIs. The FDA has a black box warning - the strongest possible - against this combo.
- Tramadol: The most common mistake. Many doctors think it’s a "safe" painkiller because it’s not a traditional opioid like oxycodone. But it’s responsible for over half of all serotonin syndrome cases involving MAOIs. A Reddit user named u/ChronicPainWarrior nearly died after taking tramadol for a toothache while on phenelzine. His temperature hit 107.1°F. He needed ICU care for three days.
- Methadone: Used for pain and addiction treatment. It has multiple mechanisms that increase serotonin, and it’s been linked to at least 17 documented cases of serotonin syndrome with MAOIs.
- Morphine, oxycodone, hydromorphone: Lower risk, but still dangerous. They don’t directly boost serotonin, but they can still contribute to the buildup, especially in sensitive individuals.
- Buprenorphine: The exception. Low doses (0.2-0.4 mg) have been used safely in MAOI patients for acute pain in clinical studies. It’s the only opioid currently recommended as an alternative.
How Long Do You Have to Wait?
If you’re stopping an MAOI, you can’t just switch to an opioid the next day. The enzymes your body needs to break down excess serotonin take time to recover.
For irreversible MAOIs like Nardil or Parnate, it takes about 14 days for your body to make new enzymes. That’s why the FDA and every major medical guideline - from the American Psychiatric Association to the Mayo Clinic - insist on a 14-day washout period before starting any opioid with serotonergic activity.
Even then, you’re not safe. Some patients have developed serotonin syndrome after just 10 days. The 14-day rule isn’t arbitrary - it’s based on hard data from clinical cases. For reversible MAOIs like moclobemide, the wait is shorter - just 24 hours - but even that’s not risk-free. There are documented cases of serotonin syndrome with moclobemide and tramadol.
And if you’re switching from an opioid to an MAOI? Same rule applies. Wait 14 days after your last opioid dose before starting the MAOI.
What Should You Do Instead?
If you’re on an MAOI and need pain relief, you have options - but you must be careful.
- Buprenorphine: Low-dose sublingual buprenorphine is the safest opioid choice. Studies show no serotonin syndrome cases in over 140 patients on MAOIs who received it.
- Acetaminophen (Tylenol): Safe and effective for mild to moderate pain. No interaction risk.
- NSAIDs: Ibuprofen, naproxen, and similar drugs are safe. Just avoid them if you have kidney or stomach issues.
- Non-drug options: Ice, heat, physical therapy, nerve blocks, or acupuncture can help manage chronic pain without drugs.
Never use tramadol, tapentadol, methadone, meperidine, or dextromethorphan (found in cough syrups) if you’re on an MAOI. Even over-the-counter cough medicines can be deadly.
Prescribing Errors Are Still Happening - and People Are Dying
You’d think this is a solved problem. But it’s not.
A 2022 study in JAMA Internal Medicine found that 4.3% of MAOI users got a contraindicated opioid within 14 days of starting their antidepressant. That’s over 11,000 dangerous prescriptions every year in the U.S. alone. Many come from primary care doctors who aren’t psychiatrists - and they often don’t know the risks.
Even worse, 31% of emergency room doctors surveyed in 2022 didn’t know tramadol was contraindicated with MAOIs. That’s not a small oversight. That’s a life-or-death knowledge gap.
Electronic health records now have hard stops - systems that block prescriptions when a dangerous combo is detected. Epic Systems blocked over 8,400 such prescriptions in 2021. But 1,200 of them were overridden by doctors. Why? Sometimes because they didn’t know the risk. Sometimes because they thought, "This patient needs pain relief now."
Pharmacies aren’t safe either. A 2022 study found that 5.8% of MAOI patients still got contraindicated opioids filled at community pharmacies. That’s nearly 1 in 17 people.

What Patients Can Do to Protect Themselves
You can’t rely on doctors or pharmacists to catch every mistake. You need to be your own advocate.
- Carry a wallet card: The National Alliance on Mental Illness offers free cards listing all contraindicated drugs. 78% of people who carry them say they use them in emergencies.
- Speak up: Tell every doctor, dentist, and ER provider you’re on an MAOI. Don’t assume they’ll check your chart.
- Check every new medication: Even OTC drugs like dextromethorphan (Robitussin DM), cough syrups, and certain supplements (like St. John’s Wort) can trigger serotonin syndrome.
- Know the signs: Fever, muscle stiffness, confusion, rapid heartbeat, shivering, or sweating - especially after starting a new painkiller - could be serotonin syndrome. If you feel this way, go to the ER immediately.
What to Do in an Emergency
If serotonin syndrome happens, time is critical. The Massachusetts General Hospital protocol says:
- Stop all serotonergic drugs immediately.
- Give benzodiazepines (like lorazepam) to calm seizures and reduce muscle rigidity.
- Use cooling blankets if the body temperature is above 104°F.
- Administer cyproheptadine - an antihistamine that blocks serotonin - at 12mg as a loading dose.
- Get to an ICU. Patients need monitoring for at least 24 hours.
There’s no home remedy. No waiting it out. If you suspect serotonin syndrome, call 911 or go to the nearest emergency room. Delaying treatment increases the risk of death.
The Bigger Picture
MAOIs are rare. But they’re not obsolete. They’re still the only effective treatment for some people with depression that won’t respond to anything else. And pain is universal. The problem isn’t the drugs - it’s the lack of communication.
Regulators are trying. The FDA now requires updated medication guides for all MAOIs, listing 12 contraindicated opioids. The European Medicines Agency now requires mandatory training for prescribers. Digital tools like SerotoninSafe - a new app that integrates with EHRs - have cut prescribing errors by 76% in pilot programs.
But the real solution isn’t technology. It’s awareness. It’s doctors asking, "Are you on an MAOI?" before writing a prescription. It’s patients speaking up. It’s pharmacists double-checking. Because this isn’t a theoretical risk. It’s a proven killer - and it’s still happening every single day.
Can I take tramadol if I’m on an MAOI?
No. Tramadol is one of the most dangerous opioids to combine with MAOIs. It increases serotonin levels and blocks its reuptake, which can trigger serotonin syndrome within hours. Over 68 cases of serotonin syndrome have been documented worldwide with this combination, including fatal cases. Never take tramadol while on an MAOI, even if your doctor says it’s "safe."
How long after stopping an MAOI can I take an opioid?
Wait at least 14 days after stopping an irreversible MAOI like phenelzine or tranylcypromine before starting any opioid with serotonergic activity (tramadol, methadone, meperidine, etc.). For reversible MAOIs like moclobemide, 24 hours is usually enough - but even then, proceed with extreme caution. Always confirm with your prescriber.
What painkillers are safe with MAOIs?
Acetaminophen (Tylenol) and NSAIDs like ibuprofen or naproxen are safe. Low-dose buprenorphine (0.2-0.4 mg sublingual) has been used safely in clinical studies. Avoid all other opioids, including codeine, hydrocodone, oxycodone, and tapentadol. Also avoid dextromethorphan in cough syrups.
Can I use over-the-counter cough medicine if I’m on an MAOI?
No. Many OTC cough syrups contain dextromethorphan, which acts like a serotonin-releasing drug. It has caused serotonin syndrome when combined with MAOIs. Always check the active ingredients. Look for alcohol-free, dextromethorphan-free options, or ask your pharmacist for a safe alternative.
What should I do if I accidentally take an opioid while on an MAOI?
If you’ve taken a high-risk opioid like tramadol or meperidine, monitor yourself closely for symptoms: fever, muscle stiffness, rapid heartbeat, confusion, or sweating. If any appear, go to the emergency room immediately. Do not wait. Call 911 or have someone take you. Bring your medication list. Time is critical - serotonin syndrome can become fatal within hours.


Solomon Ahonsi
3 February, 2026 04:19 AMThis post is literally life-saving. I knew tramadol was sketchy, but I had no idea it was this bad with MAOIs. My cousin almost died from this combo and the ER docs didn't even connect the dots. People need to stop treating pain meds like candy.
George Firican
4 February, 2026 10:00 AMThe biochemical cascade here is terrifying when you really sit with it. MAOIs don't just inhibit one enzyme-they dismantle the body's natural brake system on neurotransmitters, and then you throw in a drug that slams the gas pedal on serotonin production. It's not a drug interaction, it's a neurological grenade. And the fact that this still happens in 2024, with all our digital alerts and EHRs, speaks to a systemic failure in medical education. We've optimized for efficiency, not vigilance.
Matt W
5 February, 2026 19:30 PMI'm on Nardil and had a tooth extraction last year. My dentist asked if I was on antidepressants, I said yes, and he immediately called my psychiatrist. We ended up using buprenorphine at 0.3mg. Zero issues. Don't be afraid to ask for alternatives. Your life is worth the extra step.
Anthony Massirman
7 February, 2026 14:12 PMTramadol is a trap. Don't fall for it.
phara don
8 February, 2026 07:14 AMIs there any data on how often this happens in the elderly? My grandma was on Parnate and got prescribed tramadol for arthritis. She didn't tell anyone because she didn't think it mattered. She ended up in the hospital with a 105°F fever. We were lucky.
larry keenan
9 February, 2026 00:40 AMThe pharmacokinetic half-life of irreversible MAOIs is approximately 14 days, correlating with the resynthesis rate of monoamine oxidase enzymes in hepatic and neuronal tissues. The clinical recommendation is thus not arbitrary but grounded in enzymatic turnover kinetics. Furthermore, the serotonergic activity of tramadol is mediated via SERT inhibition and mu-opioid receptor agonism, both of which synergize pathologically with MAOI-induced monoamine accumulation.
Nick Flake
10 February, 2026 13:31 PMThis is the kind of post that makes me want to hug every doctor who takes the time to learn this stuff 🤍. And every patient who speaks up. We're not just talking about chemistry here-we're talking about people. Real people. Grandmas, dads, college kids with back pain. This isn't a footnote. It's a headline waiting to happen. Share this. Print it. Tape it to your fridge.
Chinmoy Kumar
12 February, 2026 08:14 AMi didnt know this at all. i have friend on maol and he took tramadol for back pain. he was fine but i think he was lucky. i will tell him to read this. thank you for posting
Vatsal Srivastava
12 February, 2026 21:49 PMThe real issue is that MAOIs are obsolete. Why are we still prescribing them? SSRIs work fine for 99% of people. This whole thing is just a relic of 1960s psychiatry clinging to a dying ideology. Stop romanticizing the 'last resort' drugs. They're a liability.
Monica Slypig
13 February, 2026 04:00 AMI'm American and I'm sick of this. Canada and the UK have better systems. Here, any Joe with an MD can write a script without knowing what's in it. My cousin almost died because her PCP didn't even know what MAOI stood for. This is why we need universal healthcare-so people aren't at the mercy of some overworked doc who doesn't know his own specialty.
Becky M.
14 February, 2026 11:10 AMi carry my nami card everywhere. even my dentist has it taped to his wall now. i used to be shy about it but after my friend got hospitalized for mixing dextromethorphan and phenelzine, i realized silence = danger. if you're on an maol, speak up. no one will think you're weird. they'll think you're smart.
Dan Pearson
15 February, 2026 17:08 PMOh so now we're making a whole Reddit post about how tramadol is bad? Wow. Groundbreaking. I bet the FDA didn't know that either. Also, who even uses MAOIs anymore? Are we still in the 80s? This is like warning people not to drink bleach and soda together. It's common sense. Why is this trending?
Marc Durocher
15 February, 2026 19:22 PMI used to work in pharmacy. I saw this exact combo get filled 3 times in one month. Once, the pharmacist flagged it, the doctor called back and said, 'She's in so much pain, just give it to her.' The patient was 72. She ended up in the ICU. We don't need more data. We need more courage. Someone has to say no.
Brett MacDonald
16 February, 2026 13:12 PMi think the real problem is that people think pain is something to be erased. like its a glitch in the system. but pain is communication. and drugs like maol and opioids are just band-aids on a screaming wound. maybe we should stop trying to numb everything and learn to listen to our bodies instead.
Sandeep Kumar
17 February, 2026 07:40 AMThis post is just western medical propaganda. In India we use ayurvedic painkillers and nobody dies. You people are too dependent on chemicals. This is why your healthcare system is broken.