When your lungs start to feel heavy, your chest aches, and breathing becomes a chore, it’s not just a bad cold. It could be pneumonia - and not all types are the same. The way you feel, how fast it hits, and even how it’s treated depend on what’s causing it. Three main culprits drive most cases: bacteria, viruses, and fungi. Knowing the difference isn’t just academic - it’s life-saving. Taking the wrong medicine can make things worse, fuel antibiotic resistance, and delay real recovery.
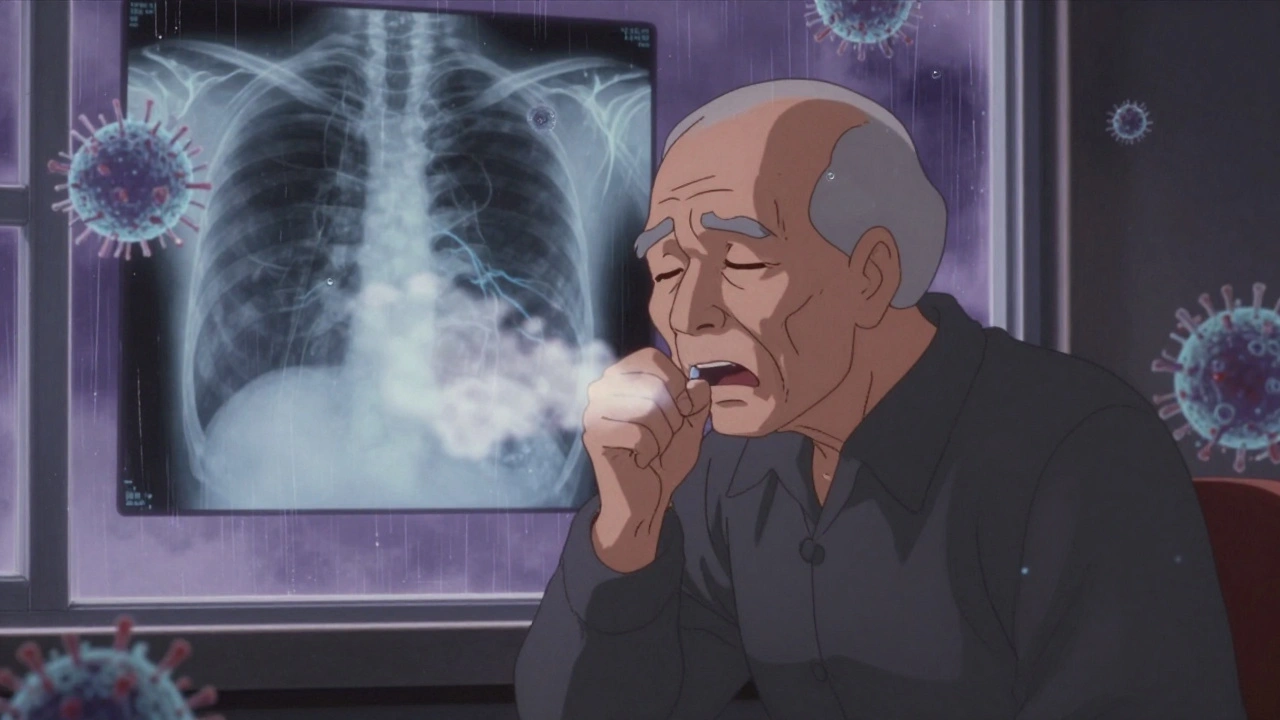
Bacterial Pneumonia: The Sudden Onset
Bacterial pneumonia hits fast. One day you might feel fine; the next, you’re running a high fever - 102°F to 105°F - with chills, sharp chest pain, and a cough that spits out thick, yellow or green mucus. Sometimes, you’ll even see blood in it. Your lips or fingernails might turn blue because your body isn’t getting enough oxygen. This is bacterial pneumonia, and it’s the most common cause of severe lung infections in adults and children.
The main villain is Streptococcus pneumoniae, responsible for over half of all community-acquired cases. It’s not picky - it affects babies, adults, and seniors. Other bacteria like Haemophilus influenzae, Staphylococcus aureus, and Mycoplasma pneumoniae (which causes "walking pneumonia") also show up. Legionella pneumophila, the bug behind Legionnaires’ disease, is rarer but dangerous, especially in older adults or those with weak immune systems.
On a chest X-ray, bacterial pneumonia looks like a solid white patch - usually on one side of the lung. That’s called lobar consolidation. It means the tiny air sacs (alveoli) are filled with pus and fluid. Doctors listen for absent or crackling sounds on one side. Blood tests often show high white blood cell counts, a clear sign your body is fighting a bacterial invasion.
Treatment? Antibiotics. Penicillin, amoxicillin, or macrolides like azithromycin are first-line for most cases. For atypical bacteria like Mycoplasma, doxycycline or fluoroquinolones work better. The key is starting the right one fast. Delayed or wrong antibiotics can turn a treatable infection into a hospital stay - or worse.
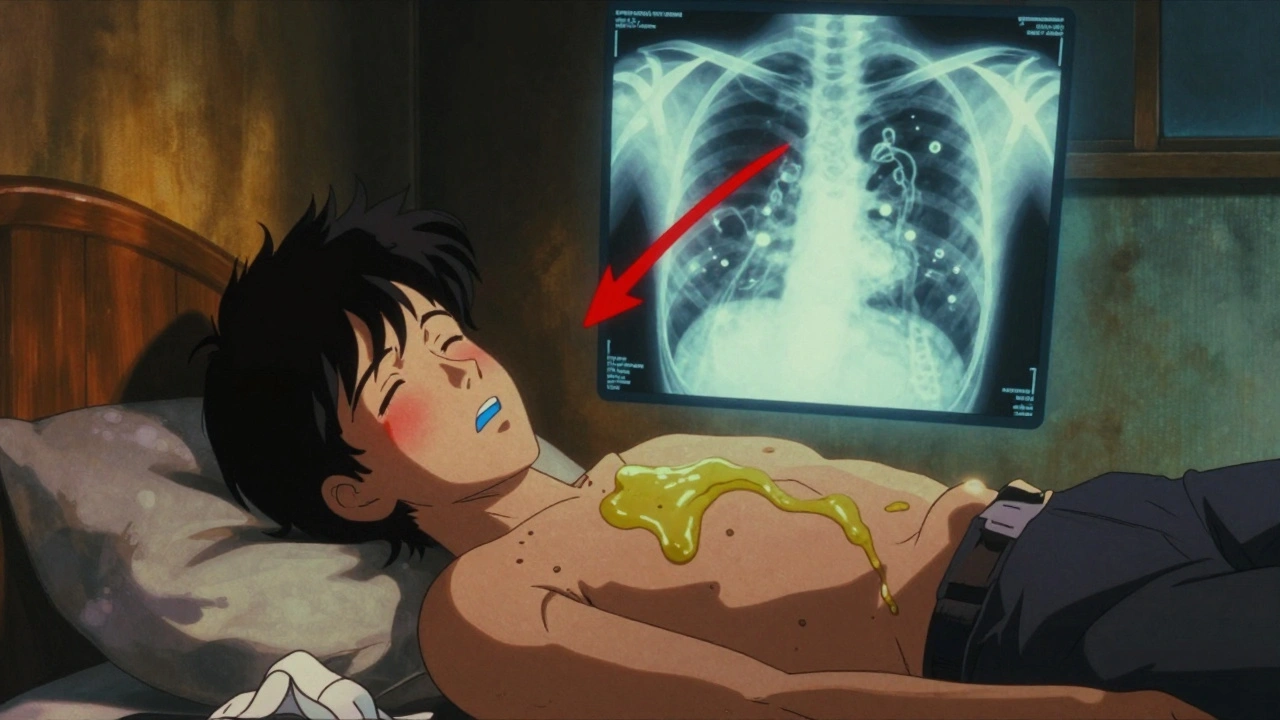
Viral Pneumonia: The Slow Burn
Unlike bacterial pneumonia, viral pneumonia creeps in. You might start with a runny nose, sore throat, or mild fever - the kind you’d write off as a cold. But after three to five days, things shift. Your cough gets worse, your muscles ache, you feel exhausted, and your fever stays low-grade - around 100°F to 102°F. You’re not spitting out thick mucus; your cough is dry, hacking, and relentless.
This is viral pneumonia. The usual suspects? Influenza A and B, respiratory syncytial virus (RSV), human metapneumovirus, rhinovirus, and SARS-CoV-2 (the virus behind COVID-19). During flu season, influenza alone causes 20-30% of all viral pneumonia cases. RSV is the top cause in babies under one. And COVID-19? It’s now a major player, especially in unvaccinated or older adults.
On a chest X-ray, viral pneumonia looks completely different. Instead of one solid white patch, you see a hazy, diffuse pattern across both lungs. That’s because the virus attacks the walls of the air sacs and small airways, not the air sacs themselves. It’s more about inflammation and fluid buildup than pus.
Here’s the catch: antibiotics won’t help. They do nothing to viruses. Yet, nearly 30% of people with viral pneumonia are still given antibiotics - a major driver of drug-resistant superbugs. The CDC says this unnecessary use increases resistance by 35% in communities.
For some viruses, antivirals work. Oseltamivir (Tamiflu) can shorten flu-related pneumonia if started within 48 hours. Remdesivir helps in severe COVID-19 cases. But for most, treatment is supportive: rest, fluids, oxygen if needed, and fever reducers. The body fights the virus itself - and that takes time. Recovery can take weeks.
And here’s another danger: viral pneumonia often opens the door for bacterial superinfections. About 25-30% of people with severe flu end up with a second, bacterial pneumonia - usually from Streptococcus pneumoniae. That’s why doctors watch closely after the first week.
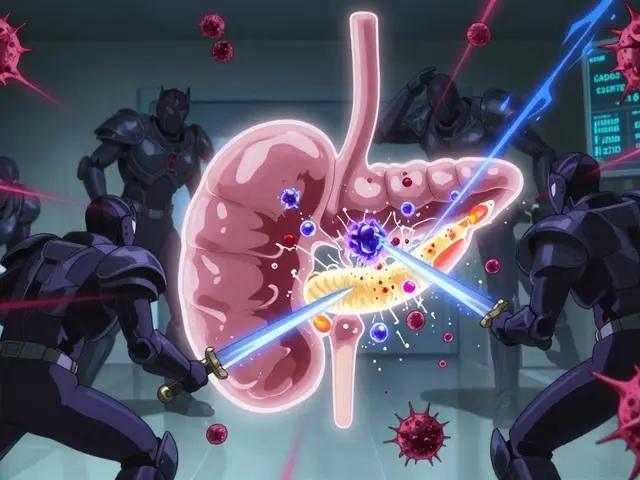
Fungal Pneumonia: The Hidden Threat
Fungal pneumonia doesn’t care about crowded offices or school buses. It thrives in soil, bird droppings, and dusty construction sites. If you’re healthy, your immune system usually keeps these fungi in check. But if you’re immunocompromised - whether from HIV, chemotherapy, an organ transplant, or long-term steroid use - you’re at serious risk.
The three big fungal offenders in the U.S. are Coccidioides (Valley fever), Histoplasma capsulatum (histoplasmosis), and Blastomyces dermatitidis (blastomycosis). Coccidioides is common in the Southwest - Arizona, California, Texas. Histoplasma hides in soil enriched by bat or bird droppings, especially in the Ohio and Mississippi River valleys. Blastomyces likes damp, wooded areas.
People at highest risk? Farmers, landscapers, construction workers, and military personnel. Those who work with soil or disturbed dust have up to 3.5 times higher chance of exposure. Even gardening can be risky if you’re immunocompromised.
Symptoms? Fever, cough with phlegm, night sweats, fatigue, and sometimes nausea or diarrhea. It’s easy to mistake for a cold, flu, or even bacterial pneumonia. But fungal pneumonia doesn’t respond to antibiotics - and if you take them, you’re wasting time while the fungus spreads.
Diagnosis is tricky. Standard tests often miss it. Doctors need special lab tests - fungal cultures, antigen tests, or PCR panels - to confirm. Chest X-rays might show patchy shadows, nodules, or even cavities. Treatment isn’t simple either. It requires antifungals like fluconazole, itraconazole, or, in severe cases, amphotericin B. Recovery can take months. And for those with weak immune systems, mortality rates hit 10-15%.
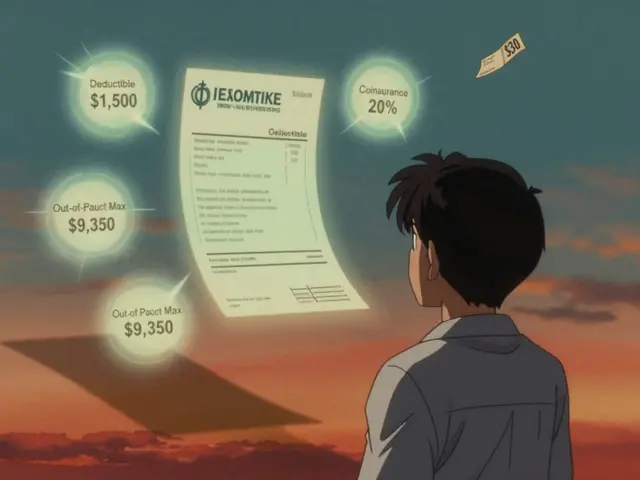
How to Tell Them Apart - And Why It Matters
Here’s a quick guide to spotting the differences:
- Onset: Bacterial - sudden. Viral - gradual. Fungal - slow, often over weeks.
- Fever: Bacterial - high (102-105°F). Viral - low to moderate (100-102°F). Fungal - variable, often persistent.
- Cough: Bacterial - productive with colored mucus. Viral - dry or minimal mucus. Fungal - phlegmy, sometimes bloody.
- Chest X-ray: Bacterial - one lobe white and dense. Viral - hazy, both lungs. Fungal - patchy, nodules, or cavities.
- Treatment: Bacterial - antibiotics. Viral - rest and antivirals if early. Fungal - antifungals only.
Getting the diagnosis right changes everything. A misdiagnosed viral case given antibiotics? No benefit. Just more resistance. A fungal case mistaken for bacterial? The infection spreads. A bacterial case treated as viral? Risk of sepsis.
Modern labs now use multiplex PCR tests that can detect 20+ pathogens from one nasal swab - with 95% accuracy. These are becoming more common in hospitals. But in clinics and homes, doctors still rely on symptoms, X-rays, and blood tests. That’s why knowing the patterns matters.
Prevention: Your Best Defense
Prevention is the most powerful tool you have.
For bacterial pneumonia, the pneumococcal vaccine is your shield. Two types - PCV20 (Prevnar 20) and PPSV23 - cover the most dangerous strains. Kids get it starting at 2 months. Adults 65+ and those with chronic conditions should get both. The vaccine cuts infection risk by 60-70% in children and 45-75% in seniors.
For viral pneumonia, the flu shot is non-negotiable. It reduces pneumonia risk by 40-60% in good-match years. The COVID-19 vaccine cuts pneumonia risk by up to 90% in the first few months after vaccination. RSV vaccines are now available for older adults and pregnant women to protect newborns.
For fungal pneumonia, it’s about exposure. If you’re at risk - immunocompromised, working outdoors in endemic areas - wear a mask when digging, cleaning birdhouses, or disturbing soil. Avoid areas with heavy bat or bird droppings. Talk to your doctor about preventive antifungals if you’re moving to a high-risk zone.
But here’s the hard truth: vaccine rates are still too low. Only 68% of adults over 65 have had the pneumococcal vaccine. For kids under 2, it’s better - 85% - but that still leaves 15% unprotected. Every unvaccinated person is a potential host for these infections.

When to Seek Help
Don’t wait for a crisis. Call a doctor if:
- Your fever stays above 102°F for more than two days
- You’re struggling to breathe, even when resting
- Your lips or nails turn blue
- You’re coughing up blood
- You feel confused, dizzy, or extremely weak
These aren’t signs to tough out. Pneumonia kills about 50,000 people in the U.S. every year. Most of those deaths are preventable with early care.
Can you get pneumonia from the flu shot?
No. The flu shot contains inactivated virus or just a piece of it - it can’t cause the flu or pneumonia. Some people feel sore, tired, or get a low-grade fever after the shot, but that’s your immune system responding, not an infection. The flu vaccine actually reduces your risk of pneumonia by preventing the flu, which often leads to secondary bacterial pneumonia.
Is fungal pneumonia contagious?
No. Fungal pneumonia isn’t passed from person to person. You catch it by breathing in spores from the environment - soil, dust, bird droppings. That’s why it’s common in certain regions or among people with specific jobs. You can’t catch it from someone else’s cough or sneeze.
Can viral pneumonia turn into bacterial pneumonia?
Yes, and it’s common. After a viral infection weakens your lungs, bacteria like Streptococcus pneumoniae or Staphylococcus aureus can move in. This is called a superinfection. About 25-30% of severe flu cases lead to bacterial pneumonia. That’s why doctors watch patients closely after the first week of illness.
Why do some people get pneumonia more than once?
Several reasons. Chronic conditions like COPD, asthma, diabetes, or heart disease make your lungs more vulnerable. Smoking damages your lung defenses. Older adults and young children have weaker immune systems. And if you’re not vaccinated, you’re exposed to the same bugs again. Each infection can cause lasting damage, making the next one more likely and more severe.
Are home remedies enough for pneumonia?
No. Rest, fluids, and humidifiers can help you feel better, but they don’t treat the infection. Bacterial pneumonia needs antibiotics. Fungal pneumonia needs antifungals. Viral pneumonia may need antivirals. Delaying medical care increases the risk of complications like sepsis, lung abscesses, or respiratory failure. Home care supports recovery - it doesn’t replace diagnosis and treatment.
What’s Next for Pneumonia Treatment?
Scientists are working on smarter ways to tell pneumonia types apart - fast. New blood tests are being tested to detect host-response patterns: how your body reacts differently to bacteria vs. viruses. If successful, these could cut unnecessary antibiotic use by 40%.
Next-gen vaccines are also coming. The 20-valent pneumococcal vaccine (Prevnar 20) already protects against 20 strains - up from 13 in older versions. It’s showing 80% effectiveness in adults. Researchers are also exploring vaccines for RSV, fungal spores, and even broad-spectrum antiviral sprays that could stop infections before they take root.
But the biggest win? Awareness. Knowing the difference between bacterial, viral, and fungal pneumonia isn’t just for doctors. It’s for every parent, every caregiver, every person who’s ever been told, "It’s just a cold." It’s not. It could be pneumonia. And the right treatment starts with the right question: What’s causing this?




Marvin Gordon
5 December, 2025 08:55 AMMan, I had bacterial pneumonia last winter and it knocked me out for weeks. Thought it was just a bad flu until I started coughing up green gunk and my wife made me go to the ER. Got antibiotics right away and was back on my feet in 10 days. Don’t mess around with this stuff.
Also, the pneumococcal vaccine? Got mine last year. Best $50 I ever spent.
Norene Fulwiler
5 December, 2025 16:59 PMI work in a nursing home and see this every season. Older folks often get fungal pneumonia and no one catches it until it’s too late. They’re treated like they have the flu, given antibiotics, and just get worse.
It’s heartbreaking. We push for fungal antigen tests now - it’s changed survival rates. Education saves lives.
Ada Maklagina
6 December, 2025 18:12 PMViral pneumonia is the silent killer. No fever no big deal right until you can’t breathe. Saw my cousin go from 'just a cold' to ICU in 48 hours. Vaccines aren't optional.
Harry Nguyen
8 December, 2025 02:45 AMSo let me get this straight - we’re supposed to trust Big Pharma’s 'antibiotics for bacteria, antivirals for viruses' fairy tale while ignoring that the CDC has been pushing vaccines since the 80s and pneumonia deaths are still rising?
Maybe the real problem isn't the bugs - it's the system that profits off treating symptoms instead of fixing immunity.
And don't get me started on 'walking pneumonia' - that's just corporate speak for 'you're not sick enough to take a day off'.
James Moore
8 December, 2025 07:59 AMIt’s fascinating - and frankly, alarming - how deeply embedded the biomedical reductionist paradigm is in our collective consciousness, wherein we treat pathogens as discrete, isolated entities, rather than recognizing pneumonia as a systemic manifestation of ecological imbalance, immune dysregulation, and sociopolitical neglect.
When you consider that 70% of community-acquired bacterial pneumonia cases are linked to chronic stress, poor nutrition, and air pollution - not merely 'Streptococcus pneumoniae' as a villainous microbe - we must shift from a pharmacological paradigm to a holistic, ecological, and preventative framework.
Antibiotics? They’re a Band-Aid on a hemorrhage. The real solution lies in restoring microbiome integrity, reducing environmental toxins, and reestablishing ancestral immune resilience - not in popping pills like candy.
And yet, the pharmaceutical-industrial complex, with its $500 billion annual revenue stream from respiratory infections, has every incentive to keep us believing in the myth of the 'quick fix'.
So yes - get the vaccine - but also grow your own food, breathe clean air, and stop drinking sugar water. That’s the real prophylaxis.
Kylee Gregory
8 December, 2025 09:47 AMI really appreciate how clear this breakdown is. I used to think pneumonia was just pneumonia - until my mom got it after chemo and it turned out to be fungal. Took months to diagnose. We were lucky.
One thing I wish more people knew: even if you’re healthy, if you’re around someone who’s immunocompromised, your 'just a cold' could be deadly to them. That’s why masking during flu season isn’t about you - it’s about protecting the quiet people in your life who can’t fight back.
Lucy Kavanagh
9 December, 2025 13:27 PMDid you know the government hides the truth about fungal pneumonia? The CDC knows Valley Fever is spreading because of climate change and land development - but they don’t warn people because it would scare homeowners in Arizona and Texas.
And the vaccines? They’re not for protection - they’re for tracking. The microchips in the needles? They’re already in your system. You think they’d let you live if you didn’t comply?
My neighbor got pneumonia after the flu shot. He died two weeks later. The hospital called it 'natural causes'.
Ask yourself - why do they push vaccines so hard but never talk about the soil spores? Coincidence? Or control?
Chris Brown
10 December, 2025 00:15 AMIt is a moral failing of the highest order that so many individuals refuse to vaccinate, thereby placing the burden of their negligence upon the shoulders of the vulnerable - the elderly, the immunocompromised, the children who cannot yet make decisions for themselves.
To dismiss pneumonia as 'just a cold' is not ignorance - it is willful indifference. To refuse a vaccine that reduces mortality by 70% is not a 'freedom' - it is a betrayal of the social contract.
I do not say this to be harsh - I say it because someone must.
And to those who claim 'natural immunity' - your body is not a temple. It is a biological machine. And like any machine, it requires maintenance - not superstition.
Stephanie Fiero
10 December, 2025 04:03 AMOMG I JUST GOT DIAGNOSED WITH BACTERIAL PNEUMONIA LAST WEEK AND THIS POST IS SO ON POINT!!!
I thought I was just tired from work - turned out I had a 104 fever and was coughing up chunks. Doc said I was lucky I came in when I did.
Got my azithromycin and am drinking tea and sleeping 12 hours a day. Don’t be like me - if you feel off for more than 3 days, GO TO THE DOCTOR. Seriously.
Also - got my flu shot yesterday. No more excuses.
PS: I typed this with one hand because my other arm hurts from the shot 😅
Michael Dioso
12 December, 2025 03:22 AMEveryone’s talking about vaccines and antibiotics like they’re magic bullets - but nobody’s talking about the fact that 80% of pneumonia cases in the U.S. happen in people who live in cities with bad air quality.
You think a vaccine fixes chronic bronchial inflammation caused by diesel fumes? Nah. You think a shot fixes a 40-year smoker’s lungs? No.
And yet - the whole narrative is pushed by pharma and the media: 'Just get the shot.'
Meanwhile, the EPA is still letting factories dump particulate matter into neighborhoods where kids are dying of pneumonia.
So sure - get the vaccine. But also demand clean air. That’s the real cure. Everything else is just triage.