What Exactly Is a Rotator Cuff Tear?
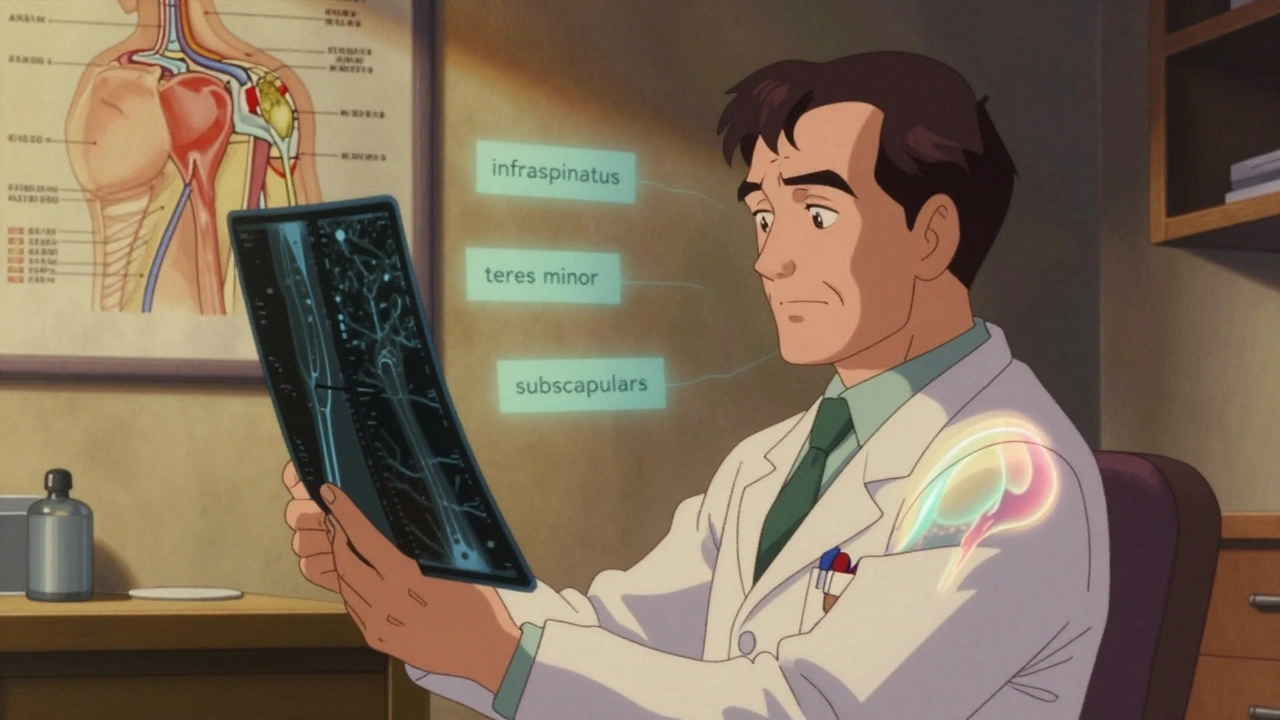
A rotator cuff tear happens when one or more of the tendons connecting the four shoulder muscles to the upper arm bone rip or wear down. These muscles - supraspinatus, infraspinatus, teres minor, and subscapularis - keep your shoulder stable and let you lift and rotate your arm. Tears can be partial, where only part of the tendon is damaged, or full-thickness, where the tendon is completely detached from the bone. They’re not just for athletes. In fact, 54% of people over 60 have rotator cuff tears without even knowing it, according to a 2019 study in the Journal of Shoulder and Elbow Surgery. Many of these tears develop slowly from wear and tear, not from a single injury.
How Doctors Diagnose Rotator Cuff Tears
Before any imaging, your doctor will start with a physical exam. They’ll check your range of motion, test your strength, and perform specific moves like the Empty Can test or Hawkins-Kennedy test to see if pain shows up when you lift your arm in certain ways. These tests are reliable, but they can’t tell you the size or exact location of the tear. That’s where imaging comes in.
X-rays are always the first step. They won’t show the torn tendon, but they reveal bone spurs, arthritis, or changes in the shoulder joint that might be contributing to the problem. Over 100% of initial evaluations include an X-ray - yes, that’s standard.
Now for the real diagnostic tools: MRI and ultrasound. Both are accurate, but they have different strengths.
MRIs give you a detailed, high-res picture of soft tissue. They’re 92% accurate at spotting full-thickness tears and 95% specific for partial tears, according to the Radiological Society of North America. MRI shows exactly how much tendon is missing, whether the muscle has shrunk, and if there’s fluid buildup. It’s the go-to when surgeons need a clear roadmap before operating.
Ultrasound, on the other hand, is faster, cheaper, and doesn’t require you to lie still in a noisy tube. It’s about 87-91% sensitive for full-thickness tears - nearly as good as MRI. Plus, it lets the doctor watch the tendon move in real time. If you lift your arm and the tendon doesn’t glide properly, that’s visible immediately. It’s also safer for people with pacemakers or metal implants, which make MRI impossible.
But ultrasound has a catch: it’s only as good as the person holding the probe. Only 45% of general radiologists are trained well enough to use it reliably. If your clinic doesn’t have a musculoskeletal specialist doing the scan, you might miss something.
Cost matters too. An ultrasound runs $200-$400. An MRI? $500-$1,200. And according to a 2022 DocPanel survey, 92% of patients preferred ultrasound over MRI because it’s quicker and less claustrophobic.
When Is Imaging Really Necessary?
Here’s something most people don’t know: the American Academy of Orthopaedic Surgeons now recommends against routine imaging for patients whose symptoms clearly point to a rotator cuff tear. Why? Because many tears are asymptomatic, and imaging can lead to unnecessary worry or surgery.
Instead, doctors are starting with 6-8 weeks of physical therapy. If you don’t improve, then they order an MRI or ultrasound. This approach saves money, avoids false positives, and prevents over-treatment. If you’ve had shoulder pain for less than two months and it’s not getting worse, give rehab a real shot before jumping to scans.
Rehabilitation: The First Line of Defense
For many people - especially those with partial tears or older adults - rehab alone works. The Journal of Orthopaedic & Sports Physical Therapy found that 85% of patients with partial-thickness tears recover full function with a structured rehab program.
Rehab isn’t just stretching. It’s a phased process:
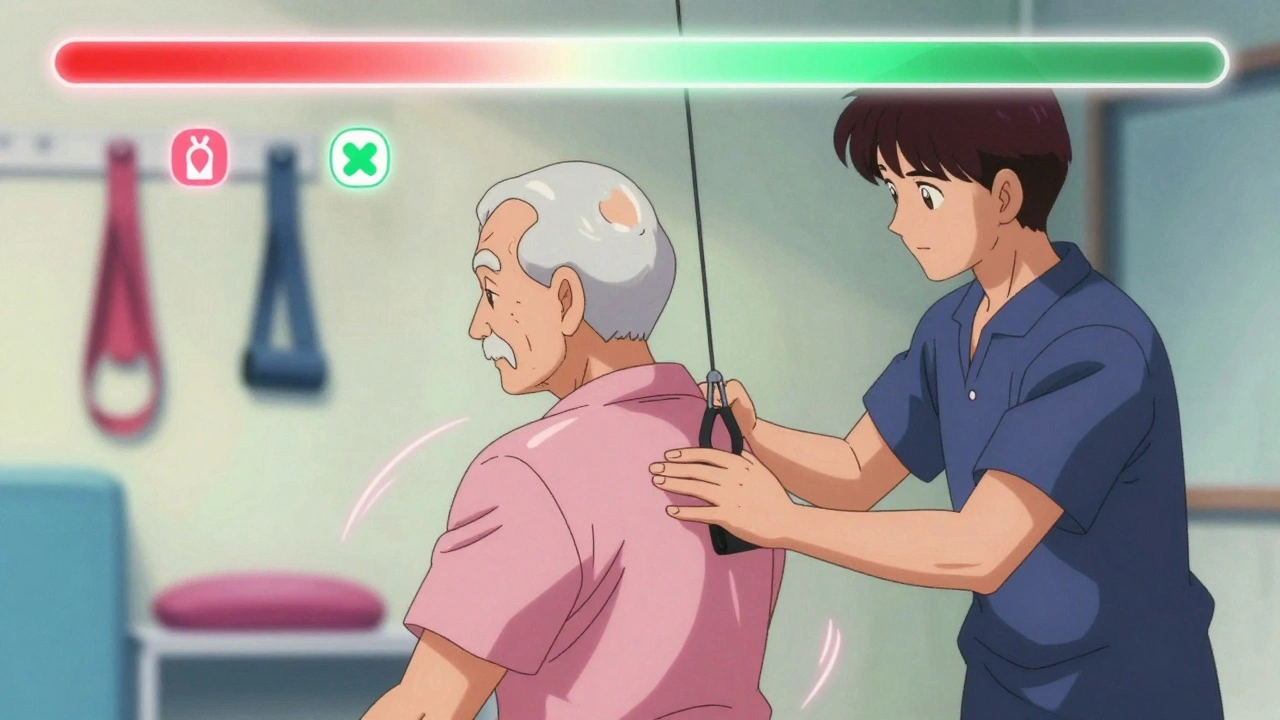
- Weeks 1-6: Passive motion - Your arm is moved for you, by a therapist or machine. No muscle effort. This keeps the joint from stiffening.
- Weeks 6-12: Active-assisted motion - You start moving your arm with help, like using your other hand or a pulley system.
- After 12 weeks: Strengthening - Focus on the rotator cuff muscles and scapular stabilizers. Exercises like external rotations with resistance bands and wall push-ups rebuild control.
Timing matters. Pushing too hard too soon can retear the tendon. Waiting too long leads to stiffness and muscle atrophy. A good physical therapist adjusts the plan based on your pain, mobility, and strength gains - not a rigid calendar.
One key thing: don’t skip the scapular exercises. Weak shoulder blades are often the real culprit behind chronic shoulder pain. If your shoulder blade doesn’t move right, your rotator cuff is forced to overwork - even if it’s healthy.
Surgical Repair: When and How
Surgery is usually considered if:
- You have a full-thickness tear and conservative rehab failed after 3-6 months
- You’re under 65 and active - an athlete, construction worker, or someone who needs full shoulder function
- The tear is large (>3 cm) or the muscle has started to shrink
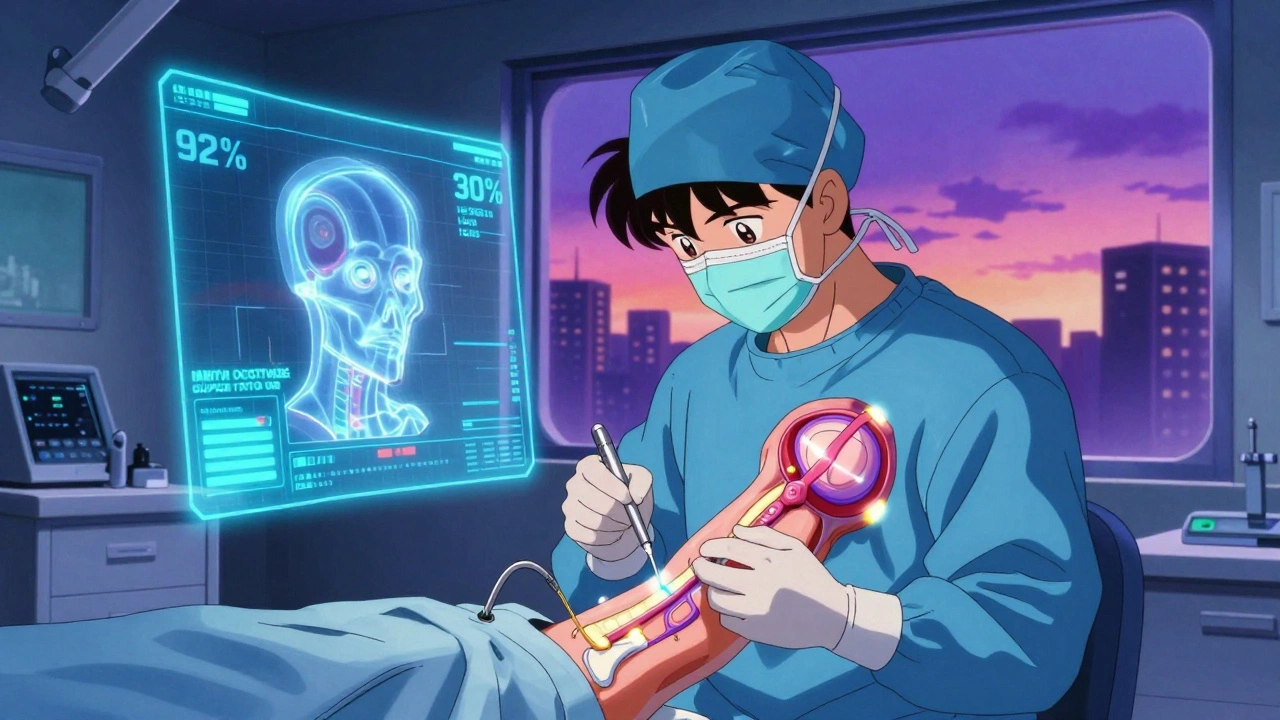
Today, 90% of repairs are done arthroscopically. That means three small incisions, a camera, and tiny instruments. The surgeon sews the tendon back to the bone using anchors. It’s less invasive than the old open surgery, which required cutting through muscle.
Arthroscopic repairs have a 30% lower complication rate than open surgery - 7.2% versus 10.3%, according to the Journal of Bone and Joint Surgery. Recovery is also faster: most people return to daily activities in 3-4 months instead of 6-8.
For massive tears - where the tendon is completely gone or the muscle is too damaged - surgeons might use patch augmentation. This involves sewing a biological graft (often from donor tissue) over the tear to give the tendon something to heal onto. It’s not standard yet, but it’s helping patients who were once told they had no options.
What Happens After Surgery?
Post-op rehab has changed dramatically. In the 1990s, patients wore slings for 6 weeks. Today, most surgeons allow passive motion within days of surgery. Why? Research shows early motion prevents stiffness and improves long-term outcomes.
Here’s the typical timeline after arthroscopic repair:
- Days 1-4: Pain control and gentle passive motion - No lifting, no reaching. Just pendulum swings and passive stretches.
- Weeks 1-6: Passive to active-assisted motion - Therapist moves your arm; you start helping.
- Weeks 6-12: Active motion and light strengthening - You lift your arm on your own. No weights yet.
- After 12 weeks: Progressive strengthening - Resistance bands, light dumbbells, and functional movements.
Full recovery takes 4-6 months. Don’t rush it. Returning to heavy lifting or sports too early is the #1 reason for retears.
Success Rates and Long-Term Outlook
Most patients are happy with the results. The American Journal of Sports Medicine found an 82% satisfaction rate at 5 years after arthroscopic repair.
But success isn’t guaranteed. Retear rates depend on tear size:
- Small tears (<1 cm): 12% retear rate
- Medium tears (1-3 cm): 18% retear rate
- Large tears (>3 cm): 27% retear rate
Age and smoking also matter. Smokers have nearly double the retear risk. So if you’re planning surgery, quitting smoking isn’t just good advice - it’s part of the treatment plan.
What About PRP and Stem Cells?
You’ve probably heard about platelet-rich plasma (PRP) injections. The idea is simple: inject concentrated healing factors from your own blood into the tear to speed recovery.
The reality? The Cochrane Review (2021) found only moderate evidence supporting PRP for rotator cuff tears. Some studies show slight pain reduction. Others show no difference compared to saline injections. It’s not a magic fix. Most insurance companies won’t cover it. And it’s not recommended as a standalone treatment - only as an add-on to surgery, and even then, the benefit is uncertain.
Stem cell therapies are even less proven. No major medical society endorses them for rotator cuff repair. Save your money. Focus on proven rehab and surgery when needed.
What’s Next in Rotator Cuff Care?
The field is getting smarter. Researchers are using machine learning to analyze MRI scans. A 2023 study in Radiology: Artificial Intelligence trained an algorithm to distinguish partial from full-thickness tears with 89% accuracy - matching expert radiologists.
That means faster, more consistent diagnoses. It also means fewer missed tears. As AI tools become standard, we’ll see fewer delays in treatment and better outcomes.
Another shift: doctors are moving away from the idea that all tears need fixing. If you’re not in pain and your shoulder works fine, sometimes the best treatment is doing nothing - and staying active.
Frequently Asked Questions
Can a rotator cuff tear heal without surgery?
Yes, many can - especially partial tears or tears in older, less active people. About 85% of patients with partial-thickness tears improve with physical therapy alone. Even some full-thickness tears stabilize over time if the surrounding muscles compensate. The key is consistent rehab, avoiding aggravating movements, and managing pain. Surgery isn’t always necessary if function and pain are under control.
Which is better for diagnosis: MRI or ultrasound?
Both are accurate for full-thickness tears, but they serve different purposes. MRI gives the most detailed anatomy, which is crucial for surgical planning. Ultrasound is faster, cheaper, and lets the doctor see the tendon move in real time. If you’re in a clinic with a skilled musculoskeletal sonographer, ultrasound is often the better first choice. If the tear is complex, or you’re planning surgery, MRI is the gold standard.
How long does recovery take after rotator cuff surgery?
Full recovery takes 4 to 6 months. You’ll be in a sling for the first few weeks, but you’ll start gentle motion within days. Strengthening doesn’t begin until 12 weeks post-op. Returning to heavy lifting or sports usually takes 6 months. Rushing the process increases the risk of retear. Patience is not optional - it’s part of the treatment.
Can I prevent a rotator cuff tear?
You can’t always prevent wear-and-tear tears, but you can reduce your risk. Strengthening the rotator cuff and shoulder blade muscles helps. Avoid repetitive overhead motions without rest. If you’re a swimmer, pitcher, or painter, take regular breaks. Maintain good posture - slouching puts extra strain on the shoulder. And if you feel pain, don’t ignore it. Early rehab can stop a small tear from becoming a big one.
Is it normal to still have pain after rotator cuff surgery?
Some discomfort is normal for the first few months, especially when moving the shoulder. But sharp pain, night pain, or sudden weakness could signal a problem - like a retear or infection. If pain doesn’t improve after 3 months of rehab, or gets worse, get imaging done. Persistent pain isn’t just part of healing - it’s a sign something else needs attention.
Next Steps: What to Do Now
If you’re dealing with shoulder pain:
- Start with 6-8 weeks of physical therapy - no imaging yet, unless you have trauma or neurological symptoms.
- If rehab doesn’t help, get an ultrasound from a specialist. If the results are unclear or you’re considering surgery, follow up with an MRI.
- If surgery is recommended, ask about the surgeon’s retear rate and their rehab protocol. Not all surgeons follow the same post-op guidelines.
- Quit smoking if you do. It directly affects healing.
- Don’t believe in quick fixes. PRP, stem cells, and massage guns won’t repair a torn tendon. Consistent rehab and, if needed, surgery are the only proven paths.
Rotator cuff tears are common, but they’re not inevitable. With the right diagnosis, patience, and effort, most people get their shoulder function back - without surgery, or with it, and without long-term disability.


Christian Landry
8 December, 2025 06:18 AMthis is insane how much i didn't know about rotator cuffs... i thought if you had pain you just needed surgery. guess i'll try PT first next time my shoulder acts up 😅
Taya Rtichsheva
9 December, 2025 11:00 AMso basically if you're over 60 and your shoulder doesn't hurt you're just lucky lol
Katie Harrison
9 December, 2025 19:50 PMI've seen too many people rush to MRI's without trying rehab first... and then they panic when they see a 'tear' on the scan that's been there for years. It's not a death sentence. It's just anatomy.
My mom had a full-thickness tear at 68, never had surgery, did PT for 6 months, and now she's gardening, lifting groceries, and even plays pickleball. The body adapts.
Doctors need to stop treating imaging findings like diagnoses. A tear on an MRI is not the same as pain in your shoulder. One is a picture. The other is a lived experience.
Mona Schmidt
9 December, 2025 21:13 PMIt's important to note that the 85% recovery rate for partial-thickness tears through physical therapy is contingent upon adherence to a structured, progressive program-not just a few stretches at home. Many patients underestimate the discipline required.
Additionally, scapular stabilization is not optional; it's foundational. Weakness in the serratus anterior or lower trapezius creates abnormal kinematics that overload the rotator cuff, regardless of tendon integrity.
Furthermore, the distinction between 'asymptomatic tear' and 'pathological tear' must be emphasized in clinical education. The former requires monitoring; the latter, intervention.
Guylaine Lapointe
10 December, 2025 05:44 AMI can't believe people still waste money on PRP and stem cells. It's pure snake oil. You wouldn't buy a miracle cream for a broken leg, so why believe in magic injections for a torn tendon?
And don't get me started on the 'natural healing' hype. Your body doesn't magically fix a tendon just because you 'believe' in it. It needs load, time, and consistency. Not vibes.
Also, if you're smoking and thinking stem cells will save you, you're not just wasting money-you're sabotaging your own healing. Quit. Now.
Philippa Barraclough
10 December, 2025 15:38 PMThe shift away from routine imaging is long overdue. The overmedicalization of aging is a serious issue in modern healthcare. Many elderly patients are subjected to unnecessary scans, which then lead to unnecessary interventions, which then lead to unnecessary anxiety.
It’s not that tears aren’t real-it’s that they’re not always clinically relevant. The goal of treatment should be functional improvement, not radiological normalization.
Additionally, the cost disparity between ultrasound and MRI is not trivial, especially for patients without comprehensive insurance. In a system where access to care is already inequitable, choosing the most appropriate, cost-effective diagnostic tool isn’t just prudent-it’s ethical.
Tim Tinh
11 December, 2025 06:00 AMman i had a rotator cuff thing last year and my dr just told me to do bands and wait. i thought he was blowing me off but turns out he was right. 4 months later i'm back to lifting. no surgery, no magic shots. just patience and dumbbells.
also smokin' is the worst. i quit after my surgery and my buddy who didn't? reteared in 6 months. no joke.
Rich Paul
11 December, 2025 23:32 PMThe biomechanics here are textbook. You've got a 30% reduction in complication rates with arthroscopic repair due to reduced tissue trauma and faster revascularization of the tendon-bone interface. The anchors create a secure osteocartilaginous fixation point, which enhances fibrocartilage regeneration.
Also, the 89% AI accuracy on MRI classification? That's huge. Deep learning models trained on annotated datasets from high-volume centers are outperforming general radiologists because they don't get fatigued.
And let's not forget the role of muscle atrophy indices-fatty infiltration >30% on MRI is a contraindication for repair. That's the real gatekeeper, not tear size.
Tiffany Sowby
13 December, 2025 07:22 AMCanada's healthcare system is so broken they're telling people to wait 8 weeks for PT? In the US we just get the MRI right away and get it fixed. Why are we letting people suffer? This is why people hate the system.