QT Prolongation Risk Assessment Calculator
This calculator estimates your risk of developing Torsades de Pointes based on clinical factors. It is not a medical diagnosis and should not replace professional medical advice. Always consult your healthcare provider for medical decisions.
Risk Factors Assessment
Enter your information to assess your risk level. The calculator uses clinically validated factors from cardiac safety guidelines.
Imagine taking a common antibiotic or antidepressant, feeling fine, and then suddenly your heart starts racing uncontrollably - not from exertion, not from stress, but because of a silent, invisible change in your heart’s electrical rhythm. This isn’t science fiction. It’s Torsades de Pointes, a rare but deadly heart rhythm triggered by over 200 medications most people never question. And here’s the scary part: half the people who experience it have zero warning signs before it happens.
What Exactly Is Torsades de Pointes?
Torsades de Pointes (TdP) isn’t just any irregular heartbeat. It’s a specific, twisting form of ventricular tachycardia that shows up on an ECG like a ribbon of QRS complexes spiraling around the baseline - hence the French name, meaning "twisting of the points." It only occurs when the heart’s QT interval is abnormally long. That interval, measured from the start of the Q wave to the end of the T wave, reflects how long the heart’s lower chambers take to recharge between beats. When it stretches too far, the electrical system becomes unstable.
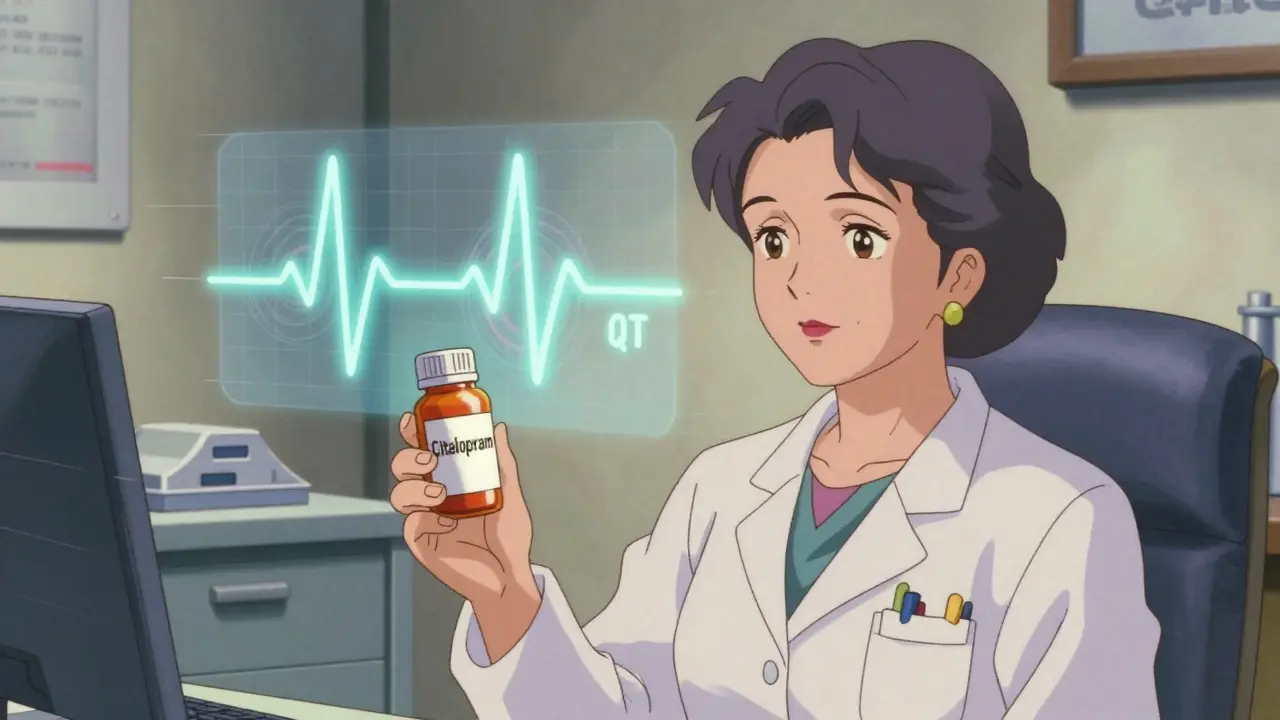
Normal QTc (corrected for heart rate) is under 450 ms in men and 460 ms in women. Once it hits 500 ms or increases by more than 60 ms from baseline, your risk of TdP doubles or triples. At that point, early afterdepolarizations - tiny, abnormal electrical sparks during repolarization - can ignite a runaway rhythm. Left unchecked, TdP can spiral into ventricular fibrillation and death within minutes.
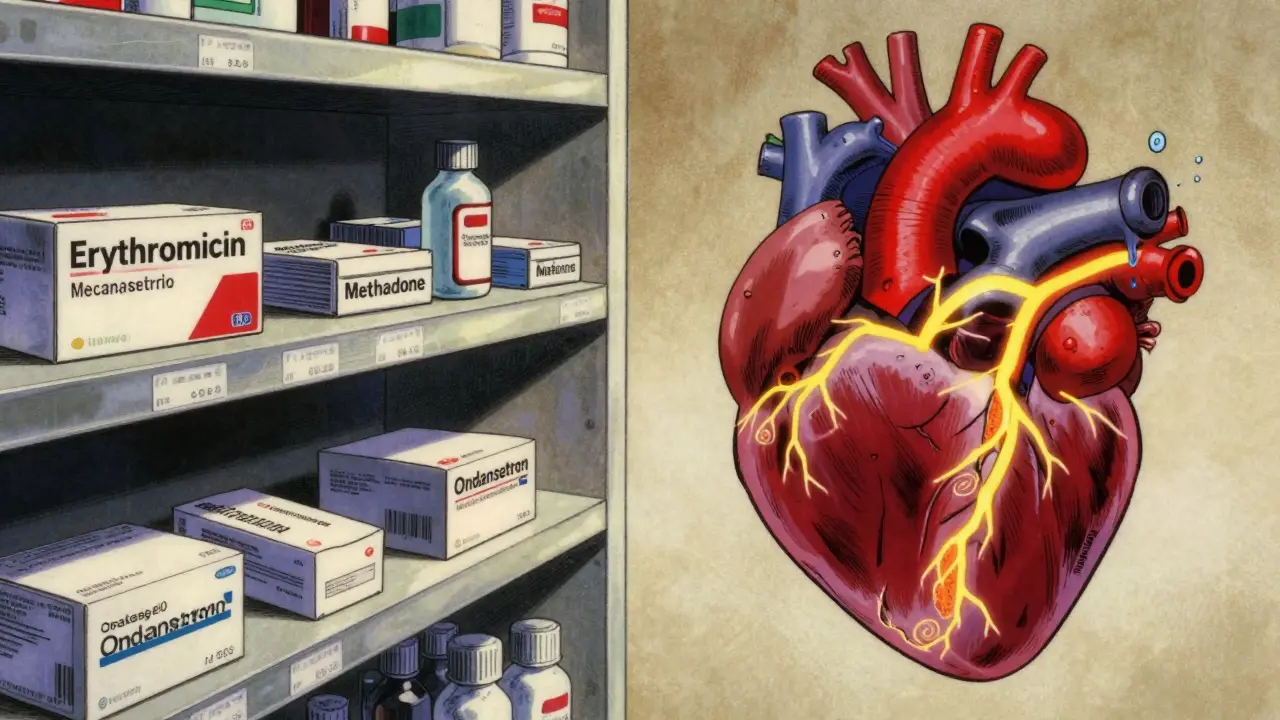
Which Medications Cause QT Prolongation?
It’s not just one drug class. It’s dozens, spread across common prescriptions you might be taking right now.
- Antibiotics: Erythromycin, clarithromycin, moxifloxacin
- Antifungals: Ketoconazole, voriconazole
- Antipsychotics: Haloperidol, thioridazine, ziprasidone
- Antidepressants: Citalopram, escitalopram (doses over 20 mg/day in elderly are especially risky)
- Anti-nausea drugs: Ondansetron (avoid IV doses above 16 mg)
- Heart drugs: Quinidine, sotalol, dofetilide - ironically, these are used to treat arrhythmias but can cause TdP themselves
- Opioid replacement: Methadone (risk spikes above 100 mg/day)
The CredibleMeds database classifies these drugs into three levels: Known Risk, Possible Risk, and Conditional Risk (meaning danger only with other factors like low potassium). Over 37 drugs carry FDA black box warnings. Ten have been pulled from the market entirely - like terfenadine, once in Seldane, which caused dozens of deaths before being withdrawn in 1998.
Who’s Most at Risk?
Not everyone who takes a QT-prolonging drug will get TdP. But certain factors stack the deck dangerously high.
- Women: 70% of cases occur in women, even though men and women experience similar QT prolongation. Hormonal differences and slower drug clearance play a role.
- Age over 65: 68% of reported cases are in older adults. Kidney and liver function decline, slowing drug removal.
- Low potassium (hypokalemia): Present in 43% of cases. Levels below 3.5 mmol/L increase risk 3.2-fold.
- Low magnesium: Found in 31% of cases. Below 1.6 mg/dL, risk jumps 2.7-fold.
- Slow heart rate: Bradycardia (under 60 bpm) occurs in 57% of cases - it gives the heart more time to develop dangerous electrical instability.
- Multiple QT drugs: 28% of TdP cases involve two or more QT-prolonging medications. Combining, say, citalopram and clarithromycin, increases risk by 63%.
- Heart disease: 41% of patients already have structural heart problems - heart failure, prior heart attack, or congenital LQTS.
Congenital long QT syndrome - inherited conditions like Romano-Ward syndrome (1 in 2,000 people) - can make someone extremely vulnerable, even to low-risk drugs. Many cases go undiagnosed until a medication triggers the first event.

How to Prevent It Before It Starts
TdP is almost always preventable - if you know where to look.
Start with a simple 5-step approach recommended by cardiac safety experts:
- Screen for inherited risk: Use the Schwartz score - a checklist of symptoms like fainting, family history, and ECG patterns - to flag possible congenital LQTS.
- Check your electrolytes: Get a basic metabolic panel before starting any high-risk drug. If potassium is below 4.0 mmol/L or magnesium below 2.0 mg/dL, correct it first.
- Review every medication: Use CredibleMeds.org (free public database) to check if any drug you’re taking - including OTC or herbal - is flagged for QT risk.
- Get a baseline ECG: Don’t skip this. Measure QTc before starting methadone, citalopram, or ondansetron. Repeat after dose increases.
- Plan follow-up monitoring: For high-risk drugs, schedule repeat ECGs at key points - like after starting methadone or increasing citalopram to 40 mg/day.
For example, VA Healthcare System data from 2018 to 2022 showed that following these steps reduced TdP incidence by 78% in patients on methadone or citalopram.
What to Do If TdP Happens
If someone collapses with a rapid, irregular pulse and loses consciousness, assume it’s TdP until proven otherwise. Time is everything.
- Give magnesium sulfate: 1-2 grams IV over 5-15 minutes. It works in 82% of cases, even if magnesium levels are normal. It stabilizes the heart’s electrical activity.
- Start pacing: Temporary transcutaneous or transvenous pacing to keep heart rate above 90 bpm. Faster rates shorten the QT interval and stop the arrhythmia. Success rate: 76%.
- Correct electrolytes: Push potassium and magnesium until levels are in the upper normal range.
- Isoproterenol: If pacing isn’t available, this IV drug can increase heart rate as a bridge.
- Stop all QT-prolonging drugs immediately.
Defibrillation is needed if TdP degenerates into ventricular fibrillation. But unlike typical VF, TdP often self-terminates - so avoid shocking unless the patient is unresponsive or in cardiac arrest.
The Bigger Picture: Regulation, Research, and Real-World Impact
Since the 1990s, drug makers have been forced to test every new molecule for QT effects under ICH E14 guidelines. That’s added $1.2 million and 6-8 months to drug development. The global QT testing market has grown from $285 million in 2018 to $412 million in 2022.
New tools are emerging. Mayo Clinic’s machine learning model, trained on 17 clinical variables, predicts individual TdP risk with 89% accuracy. The TENTACLE registry - tracking 15,000 patients - suggests that a QTc over 520 ms with a delta increase of 70 ms from baseline has a 94% chance of predicting TdP.
Regulators are shifting. The FDA no longer demands blanket avoidance of QT-prolonging drugs. Instead, they focus on risk management. That’s why methadone and citalopram aren’t banned - they’re labeled with clear dosing limits and monitoring requirements.
Still, the problem persists. In the U.S., an estimated 185-270 TdP-related deaths could be prevented yearly if standardized ECG monitoring became routine - which is why the 2022 PREVENT TdP Act was introduced in Congress.
Bottom Line: Don’t Panic - But Do Pay Attention
The absolute risk of TdP is still very low - about 4 in a million women, 2.5 in a million men. But it’s one of the few drug reactions that’s 100% preventable with simple steps: check electrolytes, review meds, get an ECG, and don’t ignore the signs.
If you’re on any of these medications - especially if you’re a woman over 65, have kidney disease, or take more than one drug - ask your doctor: "Could this affect my QT interval? Should I get an ECG?" That one question could save your life.
Can a normal ECG rule out risk for Torsades de Pointes?
No. A normal ECG doesn’t eliminate risk. TdP can develop after starting a medication, especially if electrolytes drop or another drug is added later. That’s why baseline ECGs are just the start - follow-up monitoring is essential for high-risk drugs like methadone or citalopram.
Is QT prolongation always dangerous?
Not always. A mild QT prolongation (e.g., QTc 480 ms) without other risk factors rarely leads to TdP. The danger comes from combinations - multiple drugs, low potassium, slow heart rate, or pre-existing heart disease. The key is context, not just the number.
Can I take azithromycin if I’m on an antidepressant?
It depends. Azithromycin carries a low risk of QT prolongation compared to other macrolides. But if you’re on citalopram, escitalopram, or another QT-prolonging drug, the combination can be risky - especially if you’re elderly or have kidney issues. Talk to your doctor. They may switch you to a non-QT-prolonging antibiotic like amoxicillin.
Why do women have a higher risk of TdP than men?
Women naturally have longer baseline QT intervals than men. Hormones like estrogen slow down the repolarization process, and women often clear QT-prolonging drugs more slowly due to lower liver enzyme activity. These factors make their hearts more vulnerable to the same drug dose that might be safe in men.
Is magnesium safe to take if I’m not deficient?
Yes - and it’s recommended. Magnesium sulfate given intravenously during TdP works even if your levels are normal. It stabilizes heart cell membranes and blocks abnormal electrical triggers. Oral magnesium supplements are generally safe and can help prevent recurrence, especially if you’re on diuretics or have poor diet.
Are over-the-counter drugs or supplements risky for QT prolongation?
Yes. Some OTC antihistamines (like diphenhydramine in Benadryl), herbal supplements (like St. John’s Wort), and even high-dose zinc can prolong the QT interval. Many people don’t realize these interact with prescription meds. Always tell your doctor about everything you take - including vitamins and teas.






Renia Pyles
26 January, 2026 16:58 PMThis post is pure fearmongering. I’ve been on citalopram for five years and my ECGs are always normal. If every little QT prolongation meant death, we’d all be dead by now. Stop scaring people with stats that don’t apply to them.
Rakesh Kakkad
27 January, 2026 20:14 PMIt is imperative to underscore that the pharmacokinetic and pharmacodynamic profiles of QT-prolonging agents necessitate rigorous clinical vigilance, particularly in populations with comorbid renal impairment and polypharmacy. The statistical correlations cited are not merely academic-they are life-or-death imperatives in clinical practice.
Suresh Kumar Govindan
28 January, 2026 11:52 AMThey don’t want you to know this, but the FDA and Big Pharma quietly fund studies that downplay QT risks. The real goal? Keep people on profitable meds. They’ll scare you with ‘TdP’ but never mention the $12 billion profit from antidepressants and antibiotics. Wake up.
Karen Droege
28 January, 2026 21:34 PMOH MY GOD. I just realized my grandma was on methadone AND ondansetron after her hip surgery-and her potassium was 3.1. She had that weird fainting episode they called ‘just a spell.’ This post just gave me chills. I’m dragging her to her cardiologist TOMORROW. Thank you for writing this like someone who actually cares. We need more of this-no fluff, just life-saving clarity. You just might’ve saved her life.
Simran Kaur
29 January, 2026 11:07 AMIn India, so many people take antibiotics without prescriptions-azithromycin for every cold, cipro for fever, no ECG, no labs. I’ve seen elderly patients collapse after a simple cough syrup with diphenhydramine. This isn’t just a Western problem. We need community health workers to educate families, not just doctors. Thank you for making this accessible.
Neil Thorogood
31 January, 2026 01:18 AMSo let me get this straight: you’re telling me my 70-year-old mom can’t take Zpack for her sinus infection if she’s on escitalopram… unless she gets an ECG first? And you want me to pay $300 for that? 😂 Bless your heart, but I’m just gonna switch her to amoxicillin and hope for the best. At least I know what’s in that pill.
Jessica Knuteson
31 January, 2026 13:28 PMLow risk. Low probability. Low impact. You’re overreacting to a statistical blip. People die from car rides, coffee, and breathing air. This is just another medicalized anxiety loop. Stop pathologizing normal life.
Robin Van Emous
2 February, 2026 00:07 AMI appreciate the depth here. My dad had a near-miss with TdP after a combo of clarithromycin and citalopram. He’s fine now, but we didn’t know anything. This is the kind of info that should be on every pharmacy receipt. Thank you for being clear, calm, and kind. I’ll share this with my whole family.