Medication Timing Checker
Check Your Medication Timing Needs
How does timing affect your specific medication? Enter the name of your medication below to find out.
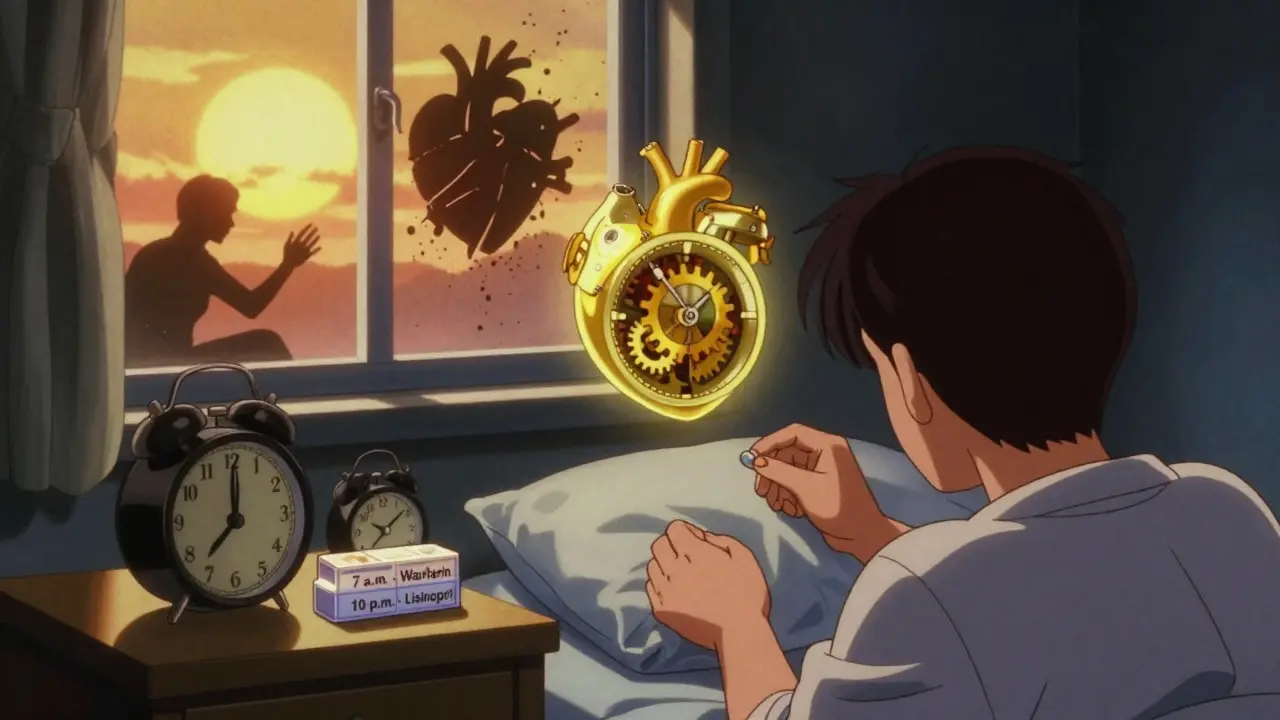
What if taking your pill 30 minutes earlier or later could make it work better-or worse? It’s not magic. It’s your body’s clock. Every day, your organs, enzymes, and hormones follow a 24-hour rhythm. And when you take your medication matters more than most people realize. For some drugs, getting the timing right can cut side effects in half. For others, it could mean the difference between a safe dose and a dangerous one.
Why Your Body’s Clock Controls How Medicines Work
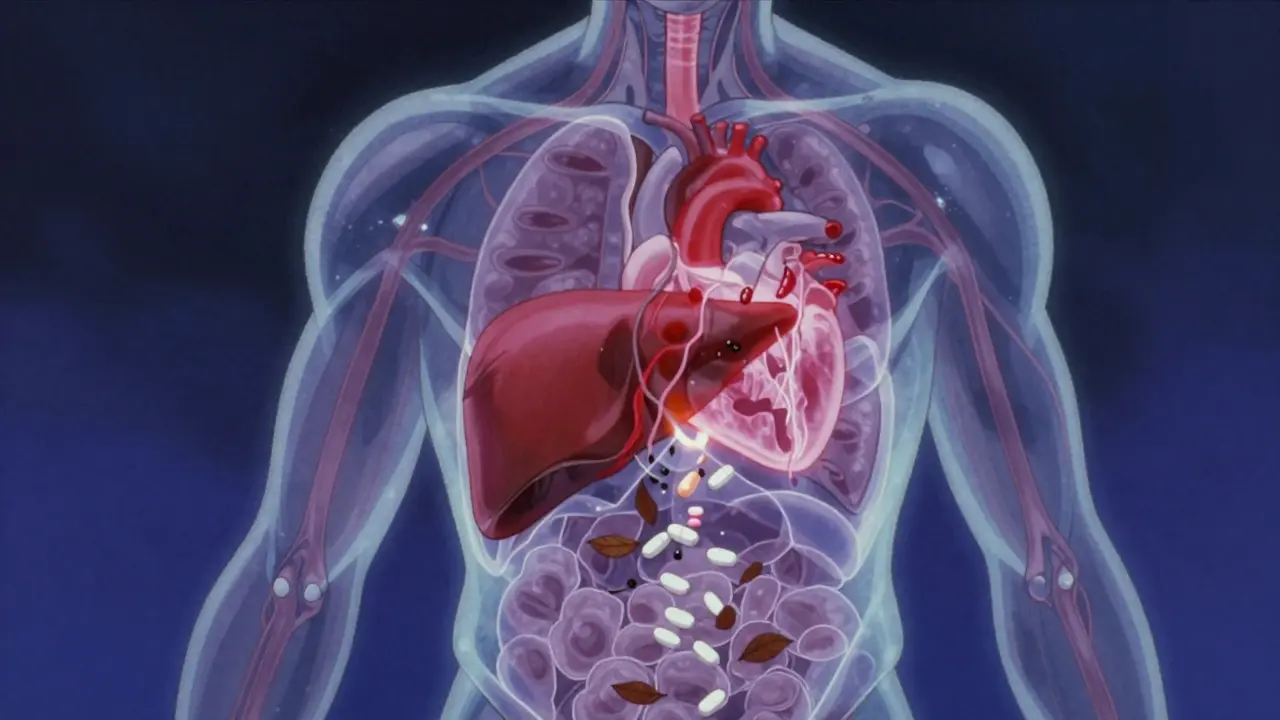
Your body doesn’t treat every hour the same. Liver enzymes that break down drugs peak at night. Blood pressure drops while you sleep. Cholesterol production spikes after midnight. These aren’t random fluctuations-they’re biological rhythms built into every cell. When you take a medication, your body doesn’t just absorb it. It processes, distributes, and eliminates it based on what time it is.
Take statins, for example. These cholesterol-lowering drugs work best when taken at night. Why? Because your liver makes most of its cholesterol while you’re asleep. Taking the pill in the evening means the drug is at its strongest when your body needs it most. Studies show nighttime statin use reduces LDL cholesterol by 15-20% more than morning doses. That’s not a small difference-it’s the kind of gap that can lower your risk of heart attack over time.
On the flip side, taking certain blood pressure meds in the morning can backfire. ACE inhibitors and ARBs work better when taken at bedtime. The MAPEC study found that patients who took these drugs at night had 29% fewer heart attacks, strokes, and other cardiovascular events. Why? Because blood pressure doesn’t just drop at night-it dips too early in some people, and morning doses can overcorrect, leading to dangerous lows. Nighttime dosing matches the body’s natural rhythm instead of fighting it.
High-Risk Medications That Can’t Wait
Not all drugs are forgiving. Some need to be taken within minutes of their scheduled time. Insulin is one. Mistiming insulin by even 15-30 minutes can trigger hypoglycemia in up to 22% of cases. A patient who takes their rapid-acting insulin after eating instead of before? They could pass out. A nurse who delays an IV insulin dose because of a call for another patient? That delay can send blood sugar crashing.
Anticoagulants like warfarin are another example. Timing errors here increase bleeding risk by up to 37%. Why? Because warfarin’s effect builds slowly over days. If you skip a dose or take it at a different time than usual, your blood’s ability to clot swings unpredictably. One day it’s too thin, the next too thick. Consistency isn’t just ideal-it’s life-saving.
Chemotherapy drugs are even more precise. Deviating from the scheduled time by more than 30 minutes can reduce effectiveness by 15-20%. Cancer cells divide at specific times, and chemo works best when it hits them at their most vulnerable. Miss the window, and you’re not just losing potency-you’re giving the cancer a chance to recover.
Why Some Medications Don’t Care About Timing
But not every drug needs this level of precision. Hydrochlorothiazide, a common diuretic for high blood pressure, can be taken anytime within a 12-hour window without major risk. Same with many antibiotics, pain relievers, and supplements. Their effects don’t depend on daily biological peaks. Taking them at 7 a.m. or 7 p.m. won’t change how they work.
So how do you know which is which? It’s not always obvious. Many patients assume all meds need perfect timing. That’s not true-and trying to force it can make adherence harder. The key is understanding your specific meds. Ask your doctor or pharmacist: “Is timing important for this one?” If they say yes, find out why. If they say no, don’t stress. Save your energy for the drugs that really matter.

How Interruptions Make Timing Errors Worse
Even if you know the right time, life gets in the way. Nurses in hospitals report that five interruptions during a med pass make errors almost certain. A phone rings. A patient calls for help. A chart needs updating. Suddenly, the 9 a.m. dose gets given at 9:45. That’s not just inconvenient-it’s dangerous for high-risk drugs.
Studies show that with zero interruptions, medication errors drop from 61% to 39%. That’s a 22-percentage-point improvement-just from reducing distractions. In busy ERs or ICUs, this isn’t theoretical. Real people get hurt because someone was interrupted while giving a dose.
At home, it’s not much better. A survey of 1,200 patients found that 68% failed to take chronotherapeutic meds at the same time every day. Why? Work schedules, caregiving duties, forgetfulness. One in two timing errors happened because someone had to pick up kids or cover a shift. For people on strict regimens, this isn’t a minor inconvenience-it’s a health threat.
How Technology Is Helping (and Sometimes Hurting)
Electronic health records were supposed to fix this. But many systems still treat all meds the same. They don’t know that insulin needs precision while aspirin doesn’t. In 2023, Epic Systems released a new module called ChronoCare that flags high-risk timing windows and blocks late doses for critical meds. That’s progress.
Barcode scanning systems also help. Hospitals using them cut timing errors by 28%. Nurses scan the patient’s wristband, then the drug. If it’s the wrong time, the system alerts them. No more guessing.
But tech alone won’t fix everything. Many clinics still use paper charts. Others have systems that don’t allow flexible scheduling. A nurse who needs to give a statin at 9 p.m. but the system only lets her choose 7 a.m. or 7 p.m.? She’ll pick 7 p.m.-even if it’s less effective. That’s system failure, not human error.
What You Can Do Right Now
You don’t need a hospital system to get this right. Start simple:
- Make a list of all your meds and ask your doctor or pharmacist: “Does timing matter for any of these?”
- For high-risk drugs (insulin, anticoagulants, chemo, certain blood pressure meds), set two alarms: one for when to take it, one as a backup 15 minutes later.
- Use a pill organizer with time labels. Don’t just use “morning” and “night”-use “7 a.m.” and “10 p.m.”
- Don’t double up if you miss a dose. Call your provider. Taking two pills at once can be dangerous.
- Track your side effects in a notebook. Did you feel dizzy after taking your blood pressure pill at 7 a.m.? Try switching to 9 p.m. and see if it changes.
Small changes add up. One patient with atrial fibrillation reduced her episodes by 40% just by switching her beta-blocker from morning to bedtime. She didn’t change the dose. She didn’t switch drugs. She just changed the time.
The Bigger Picture: Chronotherapy Is Here to Stay
What was once called “alternative” is now mainstream. The FDA started requiring chronopharmacology data in 17 new drug applications in 2022-up from just 3 in 2018. The global market for timing-based therapies is projected to hit $32.4 billion by 2027. Hospitals are training staff. Pharmacies are updating labels. Even your insurance may soon cover timing-based dosing plans.
But the real win isn’t money. It’s safety. The World Health Organization says timing errors contribute to 6.5% of all adverse drug events worldwide. That’s tens of thousands of preventable injuries every year. Fixing timing isn’t about being perfect. It’s about being smart. It’s about listening to your body’s rhythm-and matching your meds to it.
You don’t need to be a scientist to benefit. You just need to know: timing matters. For some pills, it’s everything.
Does the time I take my medication really affect side effects?
Yes, for many medications. Your body’s internal clock affects how drugs are absorbed, processed, and eliminated. Taking a statin at night can reduce LDL cholesterol by 15-20% more than taking it in the morning. Taking blood pressure meds at bedtime can cut heart attack risk by nearly 30%. For insulin or anticoagulants, even a 30-minute delay can cause dangerous side effects like low blood sugar or bleeding.
Which medications are most sensitive to timing?
High-risk medications include insulin (mistiming can cause hypoglycemia), anticoagulants like warfarin (timing errors increase bleeding risk by up to 37%), chemotherapy drugs (deviations over 30 minutes reduce effectiveness by 15-20%), and certain blood pressure meds like ACE inhibitors (bedtime dosing reduces cardiovascular events by 29%). Statins also benefit from evening dosing due to nighttime cholesterol production.
Can I take my medication at a different time if I forget?
It depends. For most routine meds like antibiotics or pain relievers, taking them a few hours late is fine. But for high-risk drugs like insulin or warfarin, never double up. Call your doctor or pharmacist. They’ll tell you whether to skip the dose, take a reduced amount, or adjust the next one. Always check before acting.
Why do some doctors not talk about medication timing?
Many clinicians still think all meds work the same no matter when you take them. It’s a gap in training. Only 14% of community hospitals have formal chronotherapy protocols, compared to 42% of academic centers. But awareness is growing. The American College of Clinical Pharmacy endorsed chronotherapy in 2022. If your doctor doesn’t mention timing, ask. It’s a simple question that could improve your safety and results.
How can I remember to take my meds at the right time?
Set two alarms on your phone-one for the scheduled time, one 15 minutes later as a backup. Use a pill organizer labeled with exact times (e.g., “7 a.m.”, “9 p.m.”). Link taking your pill to a daily habit like brushing your teeth or eating breakfast. For high-risk meds, consider a smart pill dispenser that alerts you and logs when you take it. Consistency beats perfection-just aim to take it at the same time each day.




Aysha Siera
17 January, 2026 23:24 PMThis is all government mind control disguised as science
Naomi Keyes
18 January, 2026 23:41 PMIt's important to note that chronopharmacology is not merely anecdotal-it's grounded in circadian biology, which has been peer-reviewed since the 1970s. The liver's cytochrome P450 enzymes exhibit diurnal variation, and pharmacokinetic modeling confirms that drug clearance rates fluctuate by up to 40% depending on administration time. Ignoring this is not just negligence-it's pharmacological malpractice.
Selina Warren
20 January, 2026 08:21 AMMy mom switched her blood pressure med to bedtime after reading this-she hasn't had a dizzy spell in six months. No magic, just biology. Stop treating your body like a machine that runs on ‘whenever I remember.’ It’s got a rhythm. Listen to it.
Stacey Marsengill
20 January, 2026 10:11 AMPeople think they’re being ‘responsible’ by taking pills at ‘the right time’-but let’s be real, most of you are just trying to feel like you have control over something in a world that’s falling apart. You’re not optimizing your health-you’re performing wellness. And honestly? The real side effect here is anxiety. Just take the damn pill when you’re not asleep and breathe.
Eric Gebeke
20 January, 2026 22:51 PMOf course timing matters. But who’s really to blame? The pharmaceutical companies that design drugs without considering circadian rhythms? The FDA that doesn’t mandate timing instructions on labels? Or the doctors who still think ‘morning’ is a valid dosage instruction for everything? This isn’t about patient discipline-it’s about systemic failure. And they want you to feel guilty for their incompetence.
rachel bellet
22 January, 2026 00:35 AMStatistical outliers aside, the effect sizes for chronotherapy in anticoagulants and insulin are clinically significant (p < 0.01 in multiple RCTs). The MAPEC trial’s HR for cardiovascular events was 0.71 (95% CI: 0.59–0.86). This isn’t ‘maybe helpful’-it’s a Category A recommendation per ACCP guidelines. If you’re not aligning your dosing with circadian biomarkers, you’re not practicing evidence-based medicine-you’re gambling with pharmacokinetics.
Robert Davis
22 January, 2026 20:09 PMLook, I’ve been a nurse for 22 years. I’ve seen people die because someone took their warfarin at 8 a.m. instead of 8 p.m. because the chart said ‘AM.’ The system is broken. The EHRs don’t differentiate between ‘important timing’ and ‘whatever.’ And nurses? We’re running on fumes. You want better outcomes? Hire more staff. Stop blaming the patient for a system that’s designed to fail.
Robert Cassidy
22 January, 2026 21:43 PMThey’re telling you to take your meds at night because they’re trying to make you sleep more. Less sleep means less productivity. Less productivity means less tax revenue. And who benefits? The corporations that sell sleep aids, melatonin, and smart pill dispensers. This isn’t science-it’s a controlled behavioral nudge. Wake up. Your body knows what it’s doing. Stop outsourcing your biology to an algorithm.