Imagine you’re on vacation in Spain and your blood pressure medication runs out. Back home, you get it for €5 a month. In Spain, the same pill costs €22. You have a valid prescription from your doctor in Germany. Can you walk into a Spanish pharmacy and get it? Yes-if you know how the system works.
How the EU Lets You Buy Generic Drugs Across Borders
Since 2011, EU law has guaranteed patients the right to get medicines in any member state. But it wasn’t until 2025 that the system started working smoothly. The key is the ePrescription and eDispensation service, now active in all 27 EU and EEA countries. This isn’t just a digital form. It’s a secure, encrypted link between your home country’s health system and the pharmacy abroad. When you’re in another EU country, your doctor’s prescription is sent electronically to a pharmacy there. You show your national ID or health card, and the pharmacist pulls up your prescription through the MyHealth@EU platform. No paper. No fax. No waiting. The pharmacy dispenses the generic version-same active ingredient, same safety standards, often half the price. This system works because of the eHealth Digital Service Infrastructure (eHDSI). It’s not a single app. It’s a network connecting national health portals. Germany, France, Austria, the Netherlands, and others have fully integrated it. Even Iceland, which isn’t in the EU, will be fully connected by August 2025.What You Can Actually Get-And What You Can’t
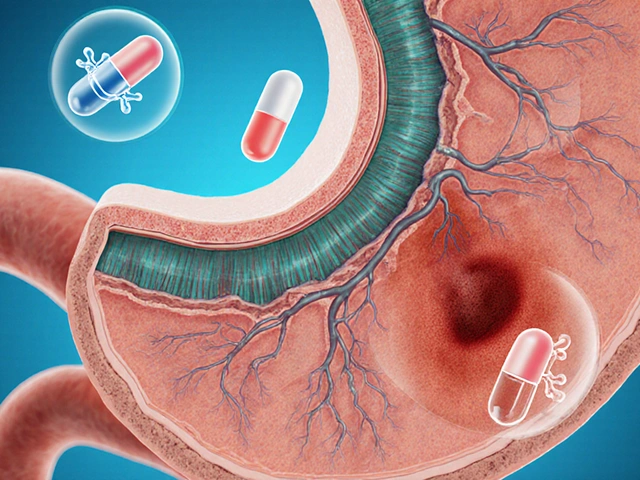
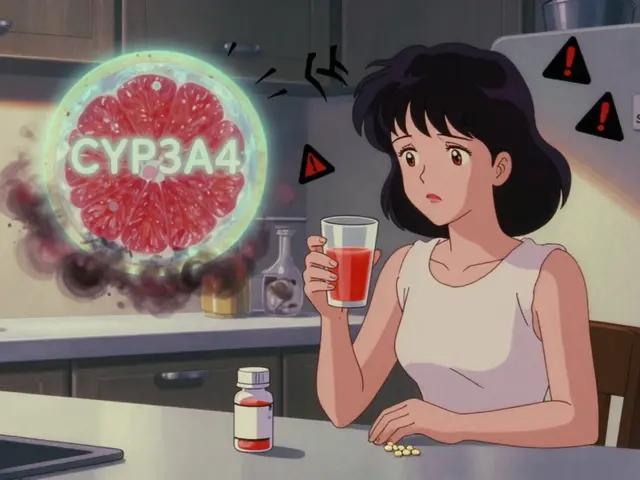
Not every drug is available everywhere. The system lets you get medicines that are legally sold in the country you’re visiting. If your generic blood pressure pill is approved in Spain, you can get it. If it’s not on Spain’s market, you can’t. That’s not a flaw-it’s regulation. You also can’t use prescriptions from outside the EU. Ireland, for example, rejects all prescriptions from the UK, even if they come from a licensed telehealth service. Pharmacists there must check the prescriber’s location, method of consultation, and registration status. A UK doctor’s e-prescription? Invalid. A German one? Valid. And here’s the catch: some medications are classified differently across countries. A drug sold as a generic in Poland might be classified as a branded medicine in Italy. That affects pricing and availability. Pharmacists abroad don’t always know your home country’s classification system. That’s why you might get a different brand name-even if the active ingredient is identical.Why This Matters for Generic Drugs
Generic drugs are the backbone of affordable healthcare in the EU. They make up over 80% of prescriptions in countries like Germany and Sweden. But price differences are huge. A 30-day supply of metformin (a common diabetes drug) costs €2.50 in Bulgaria but €18 in Denmark. Cross-border mobility lets patients shop for the best price. The European Commission estimates this could cut medication costs for chronic disease patients by up to 30% over the next five years. For elderly patients on multiple generics, that’s hundreds of euros saved annually. And it’s not just about saving money. It’s about access. In rural areas of Eastern Europe, local pharmacies often run out of stock. A patient in Romania can now get their insulin from a pharmacy in Hungary if their local one is empty. The 2025 Critical Medicines Act is pushing this further. It requires manufacturers to report real-time supply data to a new EU-wide platform. If a generic drug is running low in France, the system can flag that and redirect supply from Germany or Poland. This isn’t just convenience-it’s a safety net.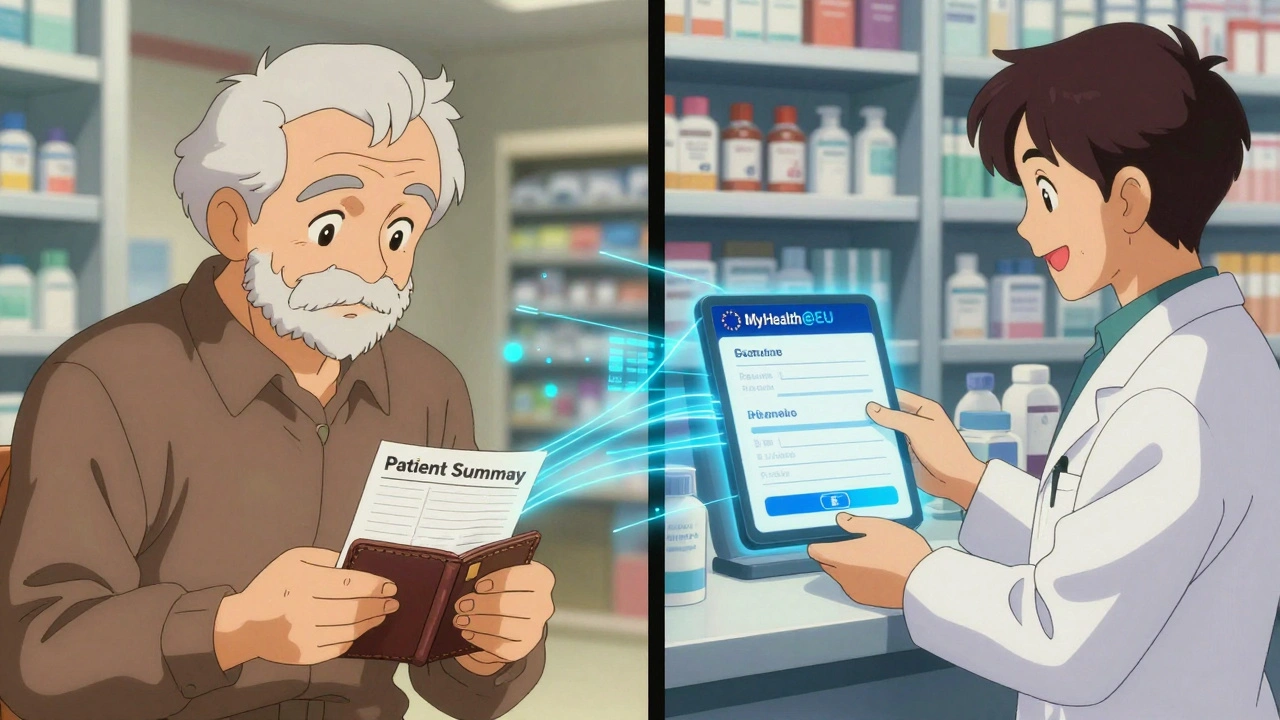
The Real Problems: Patchwork Rules and Confused Pharmacists
Here’s the truth: the system works well in theory, but not always in practice. Only 8 EU countries have clear rules for how pharmacists should handle cross-border e-prescriptions. In the rest, pharmacists are left guessing. Many don’t know how to access the eHDSI portal. Others fear liability if they dispense the wrong drug. A 2025 study by the European Association of E-Pharmacies found pharmacists need an average of 40 hours of training to handle these cases confidently. Language is another barrier. A patient from Poland gets a prescription in Polish, but the pharmacy in Portugal doesn’t have a translator. The Patient Summary feature-designed to show allergies, current meds, and history in the local language-isn’t always activated. Patients report having to print out their own summaries and carry them in their wallets. Even consent is a hurdle. To share your health data abroad, you must log into your national portal (like Germany’s eGK or Italy’s SPID), select which countries can access your records, and set a time window. Some users say it takes three separate logins and two-factor authentication steps just to get one refill. That’s not user-friendly. That’s bureaucratic.Border Regions Are Winning. Everyone Else Is Struggling
The biggest success stories are in border towns. In the Netherlands-Germany border region, 78% of patients report seamless access to cross-border pharmacy services. Why? Because they’ve been doing it for years. Local pharmacies have trained staff. Doctors coordinate across borders. Patients know the drill. In non-border areas, that number drops to 42%. In countries like Ireland, Greece, and Latvia, awareness is low. Only 38% of EU citizens even know they have the legal right to get medicines abroad. Most assume they need to fly home or pay full price. The European Commission’s 2025 review found that regions with high cross-border traffic-like the French-Spanish Pyrenees or the Austria-Czech border-have the most functional systems. They’ve built local networks. They’ve trained pharmacists. They’ve made it routine.
What’s Changing in 2025 and Beyond
The EU is pushing hard to fix these gaps. Italy replaced paper prescription stickers with GS1 DataMatrix codes in February 2025. These scannable codes hold all the drug’s info-batch number, expiry, prescriber ID-making verification faster and more secure. Other countries are expected to follow. The European Shortages Medicines Platform is now live. It tracks stock levels of 150 critical generic drugs across all member states. If a shortage hits Belgium, the system alerts pharmacies in Poland and Slovakia to increase supply. It’s not perfect yet, but it’s the first time the EU has a real-time map of generic drug availability. By 2027, the system will expand to include lab results, medical images, and hospital discharge reports. That means if you have a heart attack in Croatia and are treated there, your home doctor in Finland will automatically get your ECG and discharge summary.What You Should Do Right Now
If you take regular generic medications and travel often:- Check if your country participates in the ePrescription system. Most do-visit your national health portal to confirm.
- Enable cross-border access to your health data. Don’t wait until you’re abroad.
- Carry a printed copy of your Patient Summary (allergies, current meds, dosages) in English.
- Know the name of your generic drug in the local language. Use apps like Medscape or Epocrates to translate.
- Call ahead to pharmacies in your destination. Ask: “Do you accept ePrescriptions from [your country]?”
What’s Next for EU Generic Drug Mobility
The goal isn’t just cheaper drugs. It’s equal access. Right now, if you live in Luxembourg, you can get your meds anywhere. If you live in Malta, you’re stuck with local stock. The EU wants to fix that. The 2025 regulatory overhaul is a turning point. But progress depends on two things: political will and public awareness. If patients don’t know they can use this system, they won’t ask for it. If pharmacists aren’t trained, they won’t offer it. The numbers show it works. Cross-border pharmacy services reduced medication errors by 22% and improved chronic disease compliance by 17% in pilot regions. That’s not theoretical. That’s real health outcomes. The future isn’t about moving pills across borders. It’s about moving care-seamlessly, safely, and without paperwork. The EU has built the system. Now it’s up to patients and pharmacies to use it.Can I use my EU prescription in any EU country?
Yes-if the medicine is legally available in that country and your prescription is issued electronically through the ePrescription system. Paper prescriptions from outside the EU are not accepted in most countries. Always confirm with the pharmacy ahead of time.
Why can’t I use a UK prescription in Ireland?
Ireland only accepts prescriptions issued within the EU/EEA. UK prescriptions, even from licensed telehealth services, are considered invalid because the UK is no longer part of the EU’s health data systems. Pharmacists are legally required to reject them.
Do I need to pay for the medicine upfront?
Yes. You pay the local pharmacy price at the time of pickup. You can later apply for reimbursement from your home country’s health authority, but only if your medicine is covered under your national plan. Keep your receipt and prescription details.
Is my personal health data safe when shared across borders?
Yes. The eHDSI system uses strict EU data protection rules (GDPR). You must give explicit consent before your data is shared. You can set time limits and choose which countries can access your records. No data is stored outside your home country’s secure system.
What if the pharmacy doesn’t know how to use the ePrescription system?
Ask to speak with the pharmacist-in-charge. If they’re unsure, contact your home country’s national contact point for digital health. They can guide the pharmacy or provide documentation. You also have the legal right to request the service under EU Directive 2011/24/EU.




Courtney Blake
10 December, 2025 21:39 PMThis is why America needs to stop pretending it’s better than everyone else. We pay $300 for insulin while Europeans get it for $5 and call it ‘affordable.’ You think this is socialism? No, it’s common sense. Our system is broken and we’re too proud to fix it. 🤦♀️
Jean Claude de La Ronde
12 December, 2025 14:35 PMso uhm… the eu just invented… healthcare? wow. i thought we were still in the 19th century here. next they’ll tell us the sun rises in the east and water is wet. also, why is everyone so shocked? like… did we forget the eu exists? 🤔
Jim Irish
13 December, 2025 13:58 PMThis system represents a significant advancement in cross-border healthcare access. The technical infrastructure is sound and the legal framework is clear. Implementation remains inconsistent, but the foundation is strong. Patients should be encouraged to engage with their national health portals to enable access.
Documentation and preparation are key. A printed summary in English can bridge communication gaps where digital systems fall short.
Mia Kingsley
14 December, 2025 03:08 AMok but wait-so if i’m in spain and my pill is called ‘metformin’ here but they call it ‘glucophage’ there, do i just guess? or do i have to memorize 27 different brand names? also who made this system so complicated that i need 3 logins just to get my diabetes meds? 🤯 i swear if i have to fill out another form i’m moving to mars
Katherine Liu-Bevan
15 December, 2025 21:21 PMThe ePrescription system is one of the EU’s most underappreciated successes. The real challenge isn’t technology-it’s training and awareness. Pharmacists need standardized, country-agnostic protocols and multilingual support tools. Patients need simple guides-not 40-page PDFs.
Pro tip: Use the MyHealth@EU portal to pre-approve your data sharing before you travel. It takes 5 minutes and saves hours at the pharmacy. Also, download the generic drug names in your destination language using Medscape. It’s a game-changer.
john damon
16 December, 2025 08:44 AMOMG I JUST GOT MY INSULIN IN PORTUGAL FOR $3 😭😭😭 I CRIED IN THE PHARMACY LIKE A BABY 🥹💊 I’M SO HAPPY I CAN’T EVEN THINK ABOUT TAXES RIGHT NOW
matthew dendle
16 December, 2025 21:00 PMso the eu built a system so complex that you need a phd to get your blood pressure pills and we’re supposed to be impressed? lol. also why is everyone acting like this is new? i’ve been doing this since 2015. nobody told you? 🤡
Taylor Dressler
18 December, 2025 18:27 PMFor anyone new to this: start by checking your national health portal’s ePrescription status. Most EU countries have a simple toggle for cross-border access. Enable it now, before you need it.
Also, if a pharmacist seems unsure, ask for the ‘eHDSI support contact.’ Every pharmacy is supposed to have one. If they don’t, report it. This system only works if we push for it. You’re not being difficult-you’re helping fix it.