Insulin Carb-to-Insulin Ratio Calculator
Calculate Your Insulin Dose
Your Insulin Dose
Enter values to see calculation
If you have a blood sugar below 70 mg/dL, use 15g of fast-acting glucose (not more). Overcorrecting can cause rebound highs and weight gain.
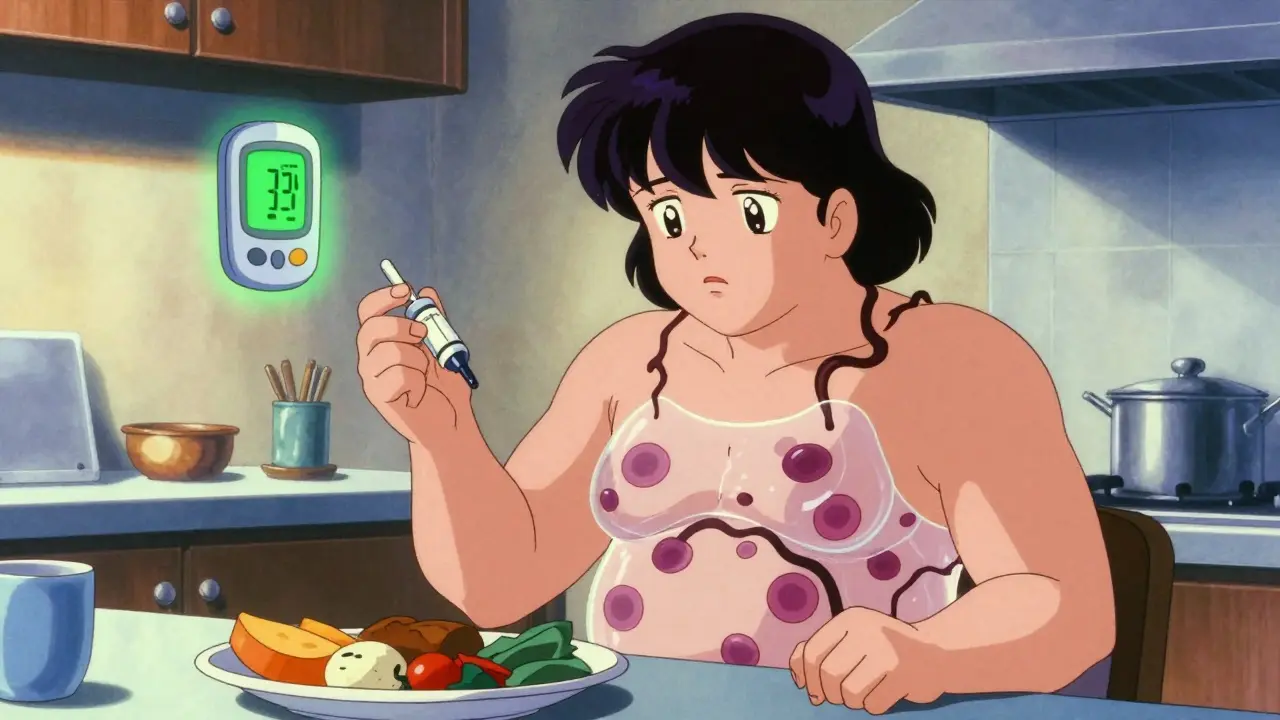
When you start insulin therapy, it’s not just about bringing your blood sugar down. It’s about doing it safely - and that’s where things get tricky. For many people with type 1 or advanced type 2 diabetes, insulin is life-saving. But it comes with two big, real-world problems: hypoglycemia and weight gain. These aren’t minor side effects. They shape how people live, what they eat, how they sleep, and whether they stick with their treatment at all.
What Hypoglycemia Really Feels Like
Hypoglycemia means your blood sugar drops below 70 mg/dL (3.9 mmol/L). It’s not just feeling a little shaky. It’s your body screaming for help. Sweating, trembling, heart racing, confusion, blurred vision - these are the early signs. If you ignore them, it gets worse: slurred speech, seizures, passing out. In severe cases, you can end up in the hospital - or worse. People with type 1 diabetes on intensive insulin therapy have about 2 to 3 severe low-blood-sugar episodes every year. That’s not rare. That’s normal for many. And it’s not just a physical risk. It’s a mental burden. Many patients admit they intentionally keep their blood sugar higher than recommended - just to avoid a scary low. One woman in Durban told her nurse she’d rather have high sugar than wake up in the middle of the night, heart pounding, unable to move. That’s the fear driving behavior. And here’s the cruel twist: the longer you’re on insulin, the more likely you are to lose your warning signs. This is called hypoglycemia unawareness. About 25% of people with type 1 diabetes develop it after 15 to 20 years. No shaking. No sweating. No warning. One minute you’re fine. The next, you’re unconscious. That’s why continuous glucose monitors (CGMs) are no longer optional for high-risk patients. They’re lifesavers.Why Insulin Makes You Gain Weight
Insulin doesn’t just move sugar into your cells. It tells your body to store fat. That’s how it works. Before insulin therapy, your body was leaking glucose through your urine because it couldn’t use it. You were losing calories every time you peed. Once you start insulin, that stops. Every gram of glucose you eat now gets absorbed. And if you eat more than your body burns, insulin turns it into fat. Studies show people gain 4 to 6 kilograms in the first year of starting insulin. For someone already struggling with weight, that’s devastating. It’s not just about looks. Extra weight makes insulin less effective. It increases blood pressure. It raises your risk of heart disease. So you’re taking insulin to protect your organs - and gaining weight that hurts them. Many patients respond by skipping doses. One study found that 15 to 20% of people with type 2 diabetes intentionally underuse insulin to avoid weight gain. That’s dangerous. Skipping insulin leads to high blood sugar, which damages nerves, kidneys, and eyes. You trade one problem for another - and end up worse off.How to Fight Hypoglycemia Before It Starts
The key isn’t avoiding insulin. It’s managing it smarter.- Check your blood sugar at least 4 to 6 times a day - before meals, at bedtime, and if you feel off.
- Use a CGM if you can. These devices track your sugar in real time and alert you before you crash.
- Learn carb counting. Know how many grams of carbs are in your food and how much insulin you need per gram.
- Always carry fast-acting sugar: glucose tablets, juice, or candy. Don’t rely on your phone or a vending machine when you’re dizzy.
- Talk to your doctor about insulin analogues. Newer types like insulin glargine (Lantus) or degludec (Tresiba) have flatter, more predictable action. They lower your risk of nighttime lows by 20 to 40% compared to older insulins like NPH.
Stopping Weight Gain Without Stopping Insulin
You don’t have to accept weight gain as inevitable. There are proven ways to fight it.- Work with a dietitian. A structured eating plan that focuses on portion control, fiber, and protein can cut weight gain in half. One trial showed people who got early nutrition counseling gained only 2.8 kg in the first year - instead of 6.2 kg.
- Move more. Even 30 minutes of walking a day improves insulin sensitivity. That means you need less insulin to do the same job.
- Ask about GLP-1 agonists. Drugs like semaglutide (Ozempic) or liraglutide (Victoza) are now used alongside insulin. They help lower blood sugar, reduce appetite, and cause weight loss. In trials, people lost 5 to 10 kg over 30 weeks - while their A1c improved.
- Don’t treat lows with too much sugar. If your blood sugar is 65 mg/dL, take 15 grams of glucose - not a whole bottle of juice. Wait 15 minutes. Check again. Repeat if needed. Overcorrecting is a major cause of rebound highs and weight gain.
Technology Is Changing the Game
Five years ago, insulin pumps and CGMs were luxury items. Now, they’re essential tools for safety. Closed-loop systems - also called artificial pancreases - automatically adjust insulin based on your real-time glucose levels. In the International Diabetes Closed-Loop trial, these systems cut time spent in hypoglycemia by 72%. That’s huge. But access is still unequal. In South Africa, many patients can’t afford CGMs or pumps. Insurance doesn’t cover them. That’s why education matters even more. Knowing how to spot a low, how to treat it correctly, and how to adjust food and activity can be the difference between safety and crisis.
When to Ask for Help
If you’re having frequent lows - more than once a week - or you’re gaining weight despite eating well and exercising, talk to your doctor. Don’t wait. Your insulin regimen can be tweaked. Your dose timing can change. Your type of insulin can switch. You might benefit from a combination therapy. There are options. Also, wear a medical bracelet. It sounds simple, but if you pass out in public, it tells strangers you have diabetes and need sugar - not a slap or a cold shower. That’s life-saving.It’s a Balancing Act - Not a Failure
Insulin therapy isn’t perfect. But it’s the best tool we have. The goal isn’t to avoid side effects completely. It’s to manage them so they don’t control your life. Hypoglycemia and weight gain are real. But they’re not inevitable. With the right knowledge, tools, and support, you can use insulin safely. You can protect your organs. You can live without fear. You can stay in control - without gaining 10 kilos or ending up in the ER. The science is clear: tight control saves your kidneys, eyes, and nerves. But only if you survive the lows. That’s why managing side effects isn’t optional. It’s part of the treatment.Can insulin cause seizures?
Yes, severe hypoglycemia from insulin can cause seizures. When blood sugar drops too low, your brain doesn’t get enough fuel to function. This can trigger muscle twitching, convulsions, and loss of consciousness. If someone is having a seizure from low blood sugar, give them glucose if they’re conscious. If they’re unconscious, call emergency services immediately and give a glucagon injection if available.
Why do I gain weight even if I eat less?
Insulin helps your body store glucose as energy. Before insulin therapy, excess sugar was lost in your urine. Once you start insulin, that stops. All the calories you eat now get absorbed and stored - mostly as fat if you’re not burning them off. Even if you eat less, your body becomes more efficient at storing energy. That’s why combining insulin with diet and movement is critical.
Is it safe to skip insulin doses to avoid weight gain?
No. Skipping insulin leads to high blood sugar, which damages your kidneys, nerves, eyes, and heart over time. The weight gain from insulin is manageable. The damage from uncontrolled diabetes is not. If you’re struggling with weight, talk to your doctor about GLP-1 agonists, diet changes, or adjusting your insulin type - never skip doses.
Do newer insulins cause less hypoglycemia?
Yes. Newer long-acting insulins like insulin glargine (Lantus) and insulin degludec (Tresiba) have a smoother, more stable action than older types like NPH. Studies show they reduce nighttime lows by 20-40%. They’re less likely to peak unexpectedly, which means fewer dangerous drops in blood sugar.
Can continuous glucose monitors prevent hypoglycemia?
They don’t prevent it, but they dramatically reduce the risk. CGMs alert you when your sugar is dropping - often before you feel symptoms. Some systems can even pause insulin delivery automatically. In clinical trials, people using CGMs had 30-50% fewer hypoglycemic events. For those with hypoglycemia unawareness, they’re life-changing.
How long does it take to adjust to insulin-related weight gain?
Most weight gain happens in the first 6 to 12 months as your body stops losing glucose in urine and starts storing energy. After that, weight tends to stabilize - especially if you adopt healthy eating and regular activity. It’s not permanent if you act early. Working with a dietitian during the first three months can cut weight gain by more than half.





Michelle M
15 December, 2025 20:44 PMInsulin isn't the enemy - it's the bridge between survival and chaos. I used to dread my morning shots until I learned that hypoglycemia isn't a failure, it's feedback. My CGM told me I was overcorrecting lows with juice boxes like they were energy drinks. Now I use 15g glucose tabs, wait, recheck. Weight gain? Still there, but slower. Walking after dinner cut my basal needs by 20%. This isn't about perfection. It's about showing up, even when your body feels like it's betraying you.
And yes - wearing my medical bracelet saved me when I passed out at the grocery store. A stranger recognized the symbol. Gave me juice. Called 911. I'm alive because someone knew what to do.
Cassie Henriques
17 December, 2025 20:42 PMLet’s talk pharmacokinetics. The reason newer analogs like degludec reduce nocturnal hypoglycemia isn’t magic - it’s molecular design. Tresiba’s hexamer stability and slow dissociation create a flatter PK/PD profile vs NPH’s unpredictable peak. Same with GLP-1 RAs: they enhance glucose-dependent insulin secretion, suppress glucagon, slow gastric emptying, and activate hypothalamic satiety centers - all while reducing HbA1c. It’s not just ‘weight loss’ - it’s metabolic reprogramming. If your provider won’t prescribe semaglutide alongside insulin, find one who will. This isn’t off-label - it’s guideline-supported.
Sai Nguyen
19 December, 2025 11:37 AMIndia has no insulin access crisis. We have a mindset crisis. People think insulin = failure. No. It’s science. You don’t skip your heart meds because you gained weight. Why skip insulin? We have cheap generics. We have government programs. Stop making excuses. Your kidneys don’t care about your pride.
John Brown
21 December, 2025 04:56 AMMy uncle started insulin at 68. Gained 18 lbs in 6 months. Thought he’d have to quit. Then he started walking with his grandkids after dinner - 20 minutes, no pressure. Lost 12 lbs in 4 months. Didn’t change his diet. Just moved. Insulin isn’t the villain. Inactivity is. You don’t need a gym. You need a reason to move. For him? It was seeing his granddaughter’s first steps. For you? Maybe it’s your next birthday party. Find your why.
Melissa Taylor
22 December, 2025 14:17 PMI used to hide my insulin pen in my purse like it was a secret weapon. Then I started saying it out loud: ‘I’m on insulin.’ And guess what? People didn’t stare. They asked questions. One coworker started checking her own sugar after talking to me. Another told me her dad had been undiagnosed for years. We’re not broken. We’re teachers. Speak up. Even if your voice shakes.
And yes - I carry glucose tabs. In my purse. In my car. In my sock drawer. Because if you wait until you’re dizzy to think about it, it’s already too late.
Nupur Vimal
23 December, 2025 08:13 AMWeight gain from insulin is just your body finally working right. Before insulin you were peeing out calories like a leaky faucet. Now you’re storing them. That’s not a flaw - that’s biology. Stop fighting your own metabolism. Eat less sugar not because insulin makes you fat but because sugar makes you crave more. Protein and fiber stabilize. Period. No fancy apps needed. Just eat real food. And if you’re still gaining? Your insulin dose is too high. Go back to your doc. Don’t guess.
Also CGMs are not a luxury. They’re your new eyes. If you can’t afford one ask for samples. Ask for charity programs. Ask until they say yes. Your life depends on it
John Samuel
24 December, 2025 22:36 PMDear community,
As a certified diabetes care and education specialist (CDCES) with over 17 years of clinical experience, I am compelled to underscore the critical importance of structured education in mitigating the adverse effects of insulin therapy. The data is unequivocal: patients who receive comprehensive, individualized nutrition counseling within the first 90 days of insulin initiation demonstrate a statistically significant reduction in both hypoglycemic events and weight gain (p < 0.01).
Moreover, the integration of continuous glucose monitoring (CGM) into routine care has demonstrated a 68% reduction in time spent below 70 mg/dL in real-world cohorts, per the ADA 2023 Standards of Care. It is not merely a tool - it is a paradigm shift.
For those concerned about weight, GLP-1 receptor agonists are not adjuncts - they are synergistic agents that address both glycemic control and energy homeostasis. Semaglutide, in particular, has demonstrated a mean weight loss of 8.7 kg over 52 weeks in patients on background insulin therapy (SUSTAIN 6 trial).
Let us move beyond fear-based narratives. Insulin is not a punishment. It is precision medicine. And with the right support, it can be a vessel for liberation - not limitation.
With deepest respect,
John Samuel, CDCES, CDE
Jocelyn Lachapelle
26 December, 2025 09:43 AMMy first low was at 3 a.m. I thought I was dying. Now I keep glucose tabs under my pillow. I don’t feel shame anymore. I feel prepared. And that’s all that matters.